14/05/2017
Crowd-sourced assessment ?
Crowd-sourced assessment of surgical skills in cricothyrotomy procedure.
Aghdasi Net Al. J Surg Res. 2015 Jun 15;196(2):302-6.
-------------------------------------
Evaluer la maîtrise de pratiques gestuelles est un véritable enjeu. Le recours à un avis d'expert est la méthode classiquement utilisée avec tous les enjeux d'identification, de disponibilité et de réduction de la dispersion des avis d'expert. Une autre approche fait jour, le recours à une communauté de professionnels pas forcément experts auxquels sont soumis un enregistrement vidéo du geste à évaluer. C'est le Crowd-sourced assessment, démarche initiée par l'université de Washington et qui semble promue par certaines équipes de chirurgie urologique robotisée. (2). Le travail proposé à la lecture porte sur la cricothyrotomie, geste de réalisation peu fréquente pour générer de véritables experts cliniques. Recourir à une démarche OSATS (1) et à un panel de visionneurs de gestes semble être aussi performant et surtout plus rapide que de recourir à quelques experts. le C(STAS, Une approche très différente de ce que nous faisons actuellement mais qui semble avoir dès à présent une application dans la vraie vie (3)
-------------------------------------
BACKGROUND:
Objective assessment of surgical skills is resource intensive and requires valuable time of expert surgeons. The goal of this study was to assess the ability of a large group of laypersons using a crowd-sourcing tool to grade a surgical procedure (cricothyrotomy) performed on a simulator. The grading included an assessment of the entire procedure by completing an objective assessment of technical skills survey.
MATERIALS AND METHODS:
Two groups of graders were recruited as follows: (1) Amazon Mechanical Turk users and (2) three expert surgeons from University of Washington Department of Otolaryngology. Graders were presented with a video of participants performing the procedure on the simulator and were asked to grade the video using the objective assessment of technical skills questions. Mechanical Turk users were paid $0.50 for each completed survey. It took 10 h to obtain all responses from 30 Mechanical Turk users for 26 training participants (26 videos/tasks), whereas it took 60 d for three expert surgeons to complete the same 26 tasks.
RESULTS:
The assessment of surgical performance by a group (n = 30) of laypersons matched the assessment by a group (n = 3) of expert surgeons with a good level of agreement determined by Cronbach alpha coefficient = 0.83.
CONCLUSIONS:
We found crowd sourcing was an efficient, accurate, and inexpensive method for skills assessment with a good level of agreement to experts' grading.
13/05/2017
Douleur: On doit mieux faire
Battlefield pain management: A view of 17 years in Israel Defense Forces.
INTRODUCTION:
Pain control in trauma is an integral part of treatment in combat casualty care (CCC). More soldiers injured on the battlefield will need analgesics for pain than those who will need life-saving interventions (LSI). It has been shown that early treatment of pain improves outcomes after traumatic injury, while inadequate treatment leads to higher rates of PTSD. The purpose of this article is to report the Israel Defense Forces Medical Corps (IDF-MC) experience with point of injury (POI) use of analgesia.
METHODS:
All cases documented in the IDF Trauma Registry (ITR) between January 1997 and December 2014 were examined. All cases of POI pain medications were extracted. Data collection included mechanism of injury, wound distribution, pain medication administered, mortality, and provider type.
RESULTS:
Of 8,576 patients, 1,056 (12.3%) patients who had at least one documented pain management treatment were included in this study. Demographics of the study population included 94.2% male and 5.8% female with a median age of 21 years. Injury mechanisms included 40.3% blast injuries (n=426) and 29% gunshot injuries (306). Of 1,513 injured body regions reported, 52% (787) were extremity wounds (upper and lower), 23% (353) were truncal wounds, and 17.7% (268) were head and neck injuries.
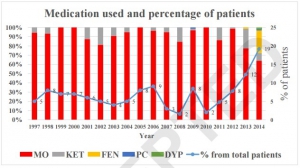
A total of 1,469 episodes of analgesic treatment were reported. The most common types of analgesics were morphine (74.7%, 1097 episodes), ketamine (9.6%, 141 episodes) and fentanyl (13.6%, 200 episodes).
Of the patients, 39% (413) received more than one type of analgesic. In 90.5% of cases, analgesia was administered by a physician or a paramedic. Over the span of the study period (1997-2014), types of analgesics given by providers at POI had changed, as fentanyl was introduced to providers. A total of 801 LSIs were performed on 379 patients (35.9%) receiving analgesia and no adverse events were found in any of the casualties.
CONCLUSION:
Most casualties at POI did not receive any analgesics while on the battlefield. The most common analgesics administered at POI were opioids and the most common route of administration was intravenously (IV). This study provides evidence that over time analgesic administration has gained acceptance and has been more common place on the battlefield. Increasingly, more casualties are receiving pain management treatment early in CCC along with LSIs. We hope that this shift will impact CCC by reducing PTSD and overall morbidity resulting from inadequate management of acute pain.
12/05/2017
Membrane Cricoïdienne: Histoire de hauteur
The height of the cricothyroid membrane on computed tomography scans in trauma patients
Nutbeam T. et Al. Anaesthesia. 2017 May 2. doi: 10.1111/anae.13905.
---------------------------------
Un travail très intéressant qui met en avant le fait que la hauteur de la membrane cricoïdienne est moindre que ce que l'on pensait, qu'elle est en fait peu dépendante des conditions d'extension du cou et qu'une canule de 6 mm n'est pas celle qui sera insérée le plus facilement.
---------------------------------
Emergency cricothyrotomy is a common feature in all difficult airway algorithms. It is the final step following a ‘can’t intubate, can’t oxygenate’ scenario. It is rarely performed and has a significant failure rate. There is variation in the reported size of the cricothyroid membrane, especially across population groups. Procedural failure may result from attempting to pass a device with too large an external diameter through the cricothyroid membrane. We aimed to determine the maximum height of the cricothyroid membrane in a UK trauma population. Electronic callipers were used to measure the maximum height of the cricothyroid membrane on 482 reformatted trauma computed tomography scans, 377 (78.2%) of which were in male patients. The mean (SD) height of the cricothyroid membrane, as independently measured by two radiologists, was 7.89 (2.21) mm and 7.88 (2.22) mm in male patients, and 6.00 (1.76) mm and 5.92 (1.71) mm in female patients. The presence of concurrent tracheal intubation or cervical spine immobilisation was found not to have a significant effect on cricothyroid membrane height.
| Device | External diameter; mm | Proportion of study population in whom the mean cricothyroid membrane height > external diameter of device |
|---|---|---|
| 6.0 mm internal diameter tracheal tube | 8.0 | 36.2% |
| 5.0 mm internal diameter tracheal tube | 6.7 | 60.5% |
| 4.0 mm internal diameter tracheal tube | 5.6 | 77.6% |
| 3.0 mm internal diameter tracheal tube | 4.2 | 93.2% |
| Shiley tracheostomy 7.5 mm internal diameter | 10.8 | 7.7% |
| Melker cricothyrotomy set | 8.2 | 34.6% |
| TracheoQuick cricothyrotomy set | 5.0 | 86.5% |
The cricothyroid membrane height in the study population was much smaller than that previously reported.Practitioners encountering patients who may require an emergency surgical airway should be aware of these data. Rescue airway equipment with variety of external diameters should be immediately available.
| Tags : airway
08/05/2017
Hémorragie: De la glace sur le visage ?
Face Cooling Increases Blood Pressure during Simulated Blood Loss
B. Johnson et Al. Proceedings of Experimental Biology 2017 Chicago
-------------------------------------
Une constatation qui ne devrait pas surprendre ceux qui s'intéressent à la médecine de plongée et au réflexe d'immersion (1, 2, 3, 4), dont le facteur principal de déclenchement est l'exposition de la face à de l'eau froide.
-------------------------------------
Introduction
Blood loss causes central hypovolemia and in severe instances, it can decrease blood pressure and lead to cardiovascular decompensation. Simple and quick interventions that can be used to prevent cardiovascular decompensation in pre-hospital settings could be a valuable tool for first responsders. Cooling the forehead and cheeks using an ice/water slurry mixture has been shown to increase blood pressure for over 15 minutes. Therefore, face cooling could be used to mitigate decreases in blood pressure during blood loss.
Purpose
We tested the hypothesis that face cooling during simulated blood loss will increase blood pressure. Methods Ten healthy participants (22 ± 2 years, 3 women) completed two randomized trials on separate days. Both trials began with 30 mmHg of lower body negative pressure (LBNP) to simulate blood loss for 6 minutes. Then, either a 2.5 L plastic bag of an ice/water slurry mixture (0 ± 0°C) (LBNP+FC) or a 2.5 L plastic bag of thermoneutral water (34 ± 1°C) (LBNP+SHAM) was placed on the forehead and eyes and 30 mmHg of LBNP was maintained for an additional 15 minutes.

We continuously measured blood pressure (Penaz method), heart rate (ECG), stroke volume (Modelflow), cardiac output, total peripheral resistance, and forehead temperature throughout the protocol.
Results
Forehead temperature did not change from LBNP (34.2 ± 0.6°C) to LBNP+SHAM (33.9 ± 1.4°C, P > 0.999) and decreased from LBNP (34.4 ± 0.5°C) to LBNP+FC (11.0 ± 1.6°C, P < 0.001). Mean arterial pressure did not change from LBNP (82 ± 10 mmHg) to LBNP+SHAM (80 ± 8 mmHg, P = 0.978), but markedly increased during LBNP+FC. The peak increase from LBNP (77 ± 9 mmHg) was observed after 3 minutes of LBNP+FC (98 ± 15 mmHg, P < 0.001). Heart rate during LBNP (76 ± 14 bpm, P = 0.978) was not different from LBNP+SHAM (75 ± 13 bpm). Heart rate was lower throughout LBNP+FC beginning at 2 minutes of FC (60 ± 16 bpm) versus LBNP (80 ± 19 bpm, P < 0.001). Stroke volume did not change from LBNP (72 ± 15 mL) to LBNP+SHAM (67 ± 18 mL, P = 0.857). However, stroke volume increased from LBNP (78 ± 16 mL) to LBNP+FC, and peaked after 5 minutes of FC (97 ± 32 mL, P < 0.001). Cardiac output did not change from LBNP (5.4 ± 1.0 L/min) to LBNP+SHAM (4.9 ± 1.0 L/min, P > 0.415). Cardiac output slightly decreased from LBNP (6.2 ± 1.5 L/min) to 2 minutes of LBNP+FC (5.3 ± 1.6 L/min, P = 0.038). Total peripheral resistance did not change from LBNP (15.6 ± 3.7 mmHg/L/min) to LBNP+SHAM (17.3 ± 3.2 mmHg/L/min, P = 0.613). Total peripheral resistance throughout LBNP+FC was greater than LBNP. The peak increase in total peripheral resistance was observed after 2 minutes of LBNP+FC (20.0 ± 6.2 mmHg/L/min) versus LBNP (13.2 ± 3.9 mmHg/L/min, P < 0.001).
Conclusions
Face cooling during simulated moderate blood loss increases blood pressure through an increase in total peripheral resistance. Although more research is warranted, face cooling during blood loss is a potential simple and quick intervention that could delay cardiovascular decompensation. Support or Funding InformationUniversity at Buffalo IMPACT Award
| Tags : choc, hémorragie
System to achieve ZERO preventable deaths
05/05/2017
Fractions coagulantes: Mieux que PFC ?
Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial.
-------------------------------------------------
Un travail dont les conclusions sont très claires. La prise en charge de la coagulopathie traumatique bénéficie bien plus d'une stratégie d'apports ciblés de fractions coagulantes concentrées, notamment de fibrinogène ici 50 mg/kg, qu'une stratégie classique basée sur l'apport de PFC.
-------------------------------------------------
Background
Effective treatment of trauma-induced coagulopathy is important; however, the optimal therapy is still not known. We aimed to compare the efficacy of first-line therapy using fresh frozen plasma (FFP) or coagulation factor concentrates (CFC) for the reversal of trauma-induced coagulopathy, the arising transfusion requirements, and consequently the development of multiple organ failure.
Methods
This single-centre, parallel-group, open-label, randomised trial was done at the Level 1 Trauma Center in Innsbruck Medical University Hospital (Innsbruck, Austria). Patients with trauma aged 18–80 years, with an Injury Severity Score (ISS) greater than 15, bleeding signs, and plasmatic coagulopathy identified by abnormal fibrin polymerisation or prolonged coagulation time using rotational thromboelastometry (ROTEM) were eligible. Patients with injuries that were judged incompatible with survival, cardiopulmonary resuscitation on the scene, isolated brain injury, burn injury, avalanche injury, or prehospital coagulation therapy other than tranexamic acid were excluded. We used a computer-generated randomisation list, stratification for brain injury and ISS, and closed opaque envelopes to randomly allocate patients to treatment with FFP (15 mL/kg of bodyweight) or CFC (primarily fibrinogen concentrate [50 mg/kg of bodyweight]). Bleeding management began immediately after randomisation and continued until 24 h after admission to the intensive care unit. The primary clinical endpoint was multiple organ failure in the modified intention-to-treat population (excluding patients who discontinued treatment). Reversal of coagulopathy and need for massive transfusions were important secondary efficacy endpoints that were the reason for deciding the continuation or termination of the trial. This trial is registered with ClinicalTrials.gov, number NCT01545635.
Findings
Between March 3, 2012, and Feb 20, 2016, 100 out of 292 screened patients were included and randomly allocated to FFP (n=48) and CFC (n=52). Six patients (four in the FFP group and two in the CFC group) discontinued treatment because of overlooked exclusion criteria or a major protocol deviation with loss of follow-up. 44 patients in the FFP group and 50 patients in the CFC group were included in the final interim analysis. The study was terminated early for futility and safety reasons because of the high proportion of patients in the FFP group who required rescue therapy compared with those in the CFC group (23 [52%] in the FFP group vs two [4%] in the CFC group; odds ratio [OR] 25·34 [95% CI 5·47–240·03], p<0·0001) and increased needed for massive transfusion (13 [30%] in the FFP group vs six [12%] in the CFC group; OR 3·04 [0·95–10·87], p=0·042) in the FFP group. Multiple organ failure occurred in 29 (66%) patients in the FFP group and in 25 (50%) patients in the CFC group (OR 1·92 [95% CI 0·78–4·86], p=0·15).
Interpretation
Our results underline the importance of early and effective fibrinogen supplementation for severe clotting failure in multiple trauma. The available sample size in our study appears sufficient to make some conclusions that first-line CFC is superior to FFP.
| Tags : coagulopathie
TCCC. Point sur la recherche US
01/05/2017
Intraosseux ? Ne pas aller trop profond
Intramedullary placement of intraosseous cannulas inserted in the preclinical treatment of polytrauma patients : A retrospective, computed tomography-assisted evaluation
Jansen Get Al. Anaesthesist. 2017 Mar;66(3):168-176
-------------------------------
Le recours à la voie intra-osseuse trouve a sa place lors de la prise en charge de traumatisé sévère. Il faut néanmoins s'assurer du bon positionnement intra-médullaire de l'aiguille. Ce travail appelle à de la prudence car il met en évidence la fréquence de positionnements non optimaux notamment un peu trop profond. Une vérification régulière s'impose dans le contexte de la traumatologie sévère.
-------------------------------
BACKGROUND:
Use of intraosseous access to the vascular system is rare in the pre-hospital setting (<1%). However, as patients for which the use of an intraosseous device is indicated are usually in a critical condition, awareness of possible application errors is vital. A survey was performed to evaluate intramedullary needle placement by means of computed axial tomography.
METHODS:
In the period of 01/01/2011 to 31/12/2015 all multislice-CT trauma scans performed in a trauma center were monitored for intraosseous devices in situ. The placement site, type of intraosseous device and needle deployed, thickness of bone and soft tissues, site for optimum needle placement, and both deviation from gold standard placement and visible complications were also recorded.
RESULTS:
In 11 out of 982 patients with suspected polytrauma that were studied during the observation period, 13 intraosseous cannulas were found (1.12%). In all cases, the EZ-IO® (Teleflex, P.O. Box 12600, Research Triangle Park, NC 27709, USA) intraosseous vascular access system was used. All applications were placed correctly in the medullary cavity, but none concurred with the current guidelines: The site of the puncture deviated laterally in seven cases, medially in two cases, cranially in four cases, and caudally in two cases.
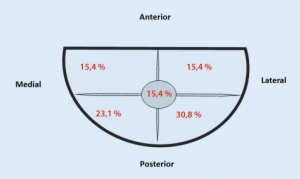
The most common error in all 13 cases was overshooting during needle introduction.
CONCLUSION:
Even though clinical criteria may suggest correct placement of an intraosseous device, the results of this survey provide evidence that deviations in positioning are common. Placement of the needle too deep can cause complications within the soft tissues or potentially impede intraosseous infusion.
| Tags : intraosseux