13/05/2017
Douleur: On doit mieux faire
Battlefield pain management: A view of 17 years in Israel Defense Forces.
INTRODUCTION:
Pain control in trauma is an integral part of treatment in combat casualty care (CCC). More soldiers injured on the battlefield will need analgesics for pain than those who will need life-saving interventions (LSI). It has been shown that early treatment of pain improves outcomes after traumatic injury, while inadequate treatment leads to higher rates of PTSD. The purpose of this article is to report the Israel Defense Forces Medical Corps (IDF-MC) experience with point of injury (POI) use of analgesia.
METHODS:
All cases documented in the IDF Trauma Registry (ITR) between January 1997 and December 2014 were examined. All cases of POI pain medications were extracted. Data collection included mechanism of injury, wound distribution, pain medication administered, mortality, and provider type.
RESULTS:
Of 8,576 patients, 1,056 (12.3%) patients who had at least one documented pain management treatment were included in this study. Demographics of the study population included 94.2% male and 5.8% female with a median age of 21 years. Injury mechanisms included 40.3% blast injuries (n=426) and 29% gunshot injuries (306). Of 1,513 injured body regions reported, 52% (787) were extremity wounds (upper and lower), 23% (353) were truncal wounds, and 17.7% (268) were head and neck injuries.
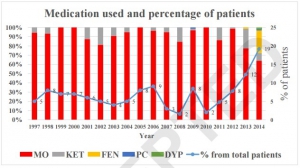
A total of 1,469 episodes of analgesic treatment were reported. The most common types of analgesics were morphine (74.7%, 1097 episodes), ketamine (9.6%, 141 episodes) and fentanyl (13.6%, 200 episodes).
Of the patients, 39% (413) received more than one type of analgesic. In 90.5% of cases, analgesia was administered by a physician or a paramedic. Over the span of the study period (1997-2014), types of analgesics given by providers at POI had changed, as fentanyl was introduced to providers. A total of 801 LSIs were performed on 379 patients (35.9%) receiving analgesia and no adverse events were found in any of the casualties.
CONCLUSION:
Most casualties at POI did not receive any analgesics while on the battlefield. The most common analgesics administered at POI were opioids and the most common route of administration was intravenously (IV). This study provides evidence that over time analgesic administration has gained acceptance and has been more common place on the battlefield. Increasingly, more casualties are receiving pain management treatment early in CCC along with LSIs. We hope that this shift will impact CCC by reducing PTSD and overall morbidity resulting from inadequate management of acute pain.
30/04/2012
Recours à la morphine et PTSD
Morphine Use after Combat Injury in Iraq and Post-Traumatic Stress Disorder.
Holbrook TL et all. N Engl J Med 2010;362:110-7.
Background
Post-traumatic stress disorder (PTSD) is a common adverse mental health outcome among seriously injured civilians and military personnel who are survivors of trauma. Pharmacotherapy in the aftermath of serious physical injury or exposure to traumatic events may be effective for the secondary prevention of PTSD.
Methods
We identified 696 injured U.S. military personnel without serious traumatic brain injury from the Navy–Marine Corps Combat Trauma Registry Expeditionary Medical Encounter Database. Complete data on medications administered were available for all personnel selected. The diagnosis of PTSD was obtained from the Career History Archival Medical and Personnel System and verified in a review of medical records.
Results
Among the 696 patients studied, 243 received a diagnosis of PTSD and 453 did not. The use of morphine during early resuscitation and trauma care was significantly associated with a lower risk of PTSD after injury. Among the patients in whom PTSD developed, 61% received morphine; among those in whom PTSD did not develop, 76% received morphine (odds ratio, 0.47; P<0.001). This association remained significant after adjustment for injury severity, age, mechanism of injury, status with respect to amputation, and selected injury-related clinical factors.
Conclusions
Our findings suggest that the use of morphine during trauma care may reduce the risk of subsequent development of PTSD after serious injury.
