29/04/2017
Une ceinture pour tourniquet ? Plutôt l'inverse.
Belts Evaluated as Limb Tourniquets: BELT Study Comparing Trouser Supporters Used as Medical Devices in a Manikin Model of Wound Bleeding.
Bequette BW et Al Wilderness Environ Med. 2017 Apr 19. pii: S1080-6032(17)30060-1.
--------------------------------
Une idée, qui n'est pas nouvelle de même que celui de pantalon intégrant un garrot (1), mais on devrait plutôt dire un tourniquet pour ceinture. Ce travail est par ailleurs intéressant car il aborde la problématique des garrots insuffisamment serrés.
--------------------------------
OBJECTIVE:
The purpose of the present study is to compare several models of commercially designed belts as used as a tourniquet.
METHODS:
In the Belts Evaluated as Limb Tourniquets (BELT) study, an experiment was designed to test the effectiveness of pants belts as non improvised medical devices to control hemorrhage in a manikin. Models of belts included Tourni-belt, Tourniquet Belt, ParaBelt, and Battle Buddy. Data collected included effectiveness, time to stop bleeding, total time of application, pressure, blood loss, and composite results (score count of good results; composite outcome good if every component was good).
RESULTS:
Differences in effectiveness percentages among models were not statistically significant. The difference in mean between users was statistically significant for stop time, total time, pressure, blood loss, composite score, and composite outcome. Mean time to stop bleeding differed for only 1 pair of models after the Tukey-Kramer adjustment; ParaBelt was faster than Tourniquet Belt. Mean total time of application differed between ParaBelt-Tourniquet Belt and Tourni-belt-Tourniquet Belt; the former model in both pairs was faster. No significant difference in mean blood loss measured by model was found. For composite outcome score, no pairwise difference between models was significant. For composite outcome (good-bad), ParaBelt had good results in 75% of tests; the other 3 models had significantly worse results.
CONCLUSIONS:
In a preliminary laboratory analysis of belt tourniquet models using a manikin, performance differed by model. ParaBelt performed better than other models for the composite outcome.our tourniquet ?
| Tags : tourniquet
22/04/2017
3 côtés: Non occlusif ? Pas tous égaux
Do vented chest seals differ in efficacy? An experimental evaluation using a swine hemopneumothorax model
--------------------------------
Un travail très pratique qui fait le point sur la performance des pansements 3 côtés non occlusifs. Plusieurs sont disponibles sur le marché. Mais qu'en est il des divers dispositifs proposés sur le marché. On dispose déjà de données concernant les propriétés "adhésives" de ces dispositifs (1). Avec ce travail, on a en plus une idée sur la capacité de ces pansements à permettre l'écoulement de saignement intra-thoraciques. L'historique valve d'asherman doit être considérée comme obsolète.
--------------------------------
OBJECTIVE:
Hemopneumothorax (HPTX) is the second leading cause of potentially preventable death among combat casualties. We investigated the ability of five FDA-approved non-occlusive chest seals (CSs) to seal a bleeding chest wound and prevent tension HPTX in a swine model.
METHODS:
Following instrumentation, an open chest wound was created in the left thorax of spontaneously air-breathing anesthetized pigs (n=26, 43 Kg). Autologous fresh blood (226 mL) was then infused into the pleural cavity to produce HPTX. The chest wounds were then sealed with CSs. The sealant strength and venting function of CSs were challenged by infusion of 50 mL more blood directly into the chest wound and incremental air injections into the pleural cavity. Tension HPTX was defined as intrapleural (IP) pressure ≥ +1 mmHg and >20% deviation in physiological measurements.
RESULTS:
An open chest wound with HPTX raised IP pressure (~ -0.7 mmHg) and caused labored breathing and reductions in PaO2 and SvO2 (P<0.01). Sealing the wounds with the CSs restored IP pressure, and improved breathing and oxygenation. Subsequent blood infusion into the wound and IP air injections produced CS-dependent responses.
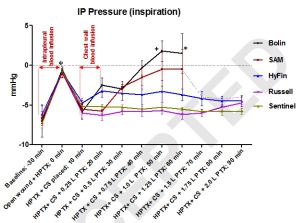
CSs with one-way valves (Bolin and SAM) did not evacuate the blood efficiently; pooled blood either detached the CSs from skin and leaked out (75%), or clotted and clogged the valve and led to tension HPTX (25%). Conversely, CSs with laminar venting channels allowed escape of blood and air from the pleural cavity and maintained IP pressure and oxygenation near normal levels. Success rates were 100% for Sentinel and Russell (6/6); 67% for HyFin (4/6); 25% for SAM (1/4); and 0% for Bolin (0/4) CSs (p=0.002).
CONCLUSION:
The sealant and valve function of vented CS differed widely in the presence of bleeding chest wounds. Medics should be equipped with more effective CSs for treating HPTX in the field.
| Tags : pneumothorax
20/04/2017
Envenimations scorpioniques
| Tags : envenimations
11/04/2017
Tourniquet: Les israéliens, pour +++
Point of injury tourniquet application during Operation Protective Edge - what do we learn?
BACKGROUND:
Hemorrhage is a leading cause of preventable death on the battlefield. Timely tourniquet application to massively bleeding extremity wounds is critical for casualty survival albeit with reported adverse effects to extremity integrity. The aim of this study was to describe the immediate and short term outcomes of point of injury (POI) tourniquet applications during 'Operation Protective Edge' (OPE).
METHODS:
A case series study regarding tourniquet application at the POI during OPE was collected. The data gathered included reports by medical providers at the POI, aerial and land evacuation vehicles, and receiving hospitals. Variables collected included, the number of tourniquet applications, caregiver level, tourniquet type, limb characters, tourniquet effectiveness, in-hospital procedures, complications and short term limb outcome.
RESULTS:
During OPE, the Israeli Defense Forces Medical Corps (IDF-MC) treated 704 casualties. Out of these, 90 casualties were treated with 119 tourniquets out of which 79 survived. Penetrating trauma was the mechanism of injury in 97.8% (88/90) of the casualties. Injuries sustained from Improvised explosive devices (IED) and shrapnel were related to the use of more than one tourniquet per casualty and per limb (p=0.034). The success rate of the first tourniquet was reported to be 70% (84/119), regardless of caregiver level (P=0.56), tourniquet type (P=0.16) or limb characters (p=0.48). two of the conversions failed and thus a new tourniquet was applied. Fasciotomy was performed on 8 casualties (a single limb in each). Vascular injury was presumed to be the indication for fasciotomy in three of these cases, in the other five limbs (6%, 5/85) no vascular involvement was discovered during surgery and the fasciotomy is suspected as tourniquet related. 7%) 6/85) suffered from neurological sequela that could not be explained by their primary injury. Total complication rate was 11.7% (10/85) (one patient had both fasciotomy and neural complication without vascular injury)
CONCLUSION:
Tourniquet use on the battlefield is a simple method of eliminating preventable death, we believe that clinical practice guidelines should promote liberal use of tourniquets by trained combatants and medical personnel with abilities to convert to direct pressure hemorrhage control when possible since an unjustified tourniquet application risks low rates minor morbidity whereas a justifiable tourniquet not applied may be lethal.
| Tags : tourniquet

