25/12/2015
Transfusion de CGR: Les + graves seulement
Red Blood Cell Transfusion and Mortality in Trauma Patients: Risk-Stratified Analysis of an Observational Study
Perel P et Al. PLoS Med. 2014 Jun 17;11(6):e1001664
-------------------------------------
Les données qui suivent sont extraites de la cohorte des patients inclus dans l'étude CRASH2. Cette réinterprétation des données a pour objectif d'analyser le lien entre la mortalité à 28 jours et la transfusion de CGR. Les auteurs retrouvent un effet délétère de la transfusion de CGR pour les patients les moins à risque de mortalité. Ceci est en faveur des démarches de stratégies transfusionnelles sinon restrictives du moins raisonnées en fonction du contexte notamment préhospitalier où cette pratique associée à l'apport de fractions coagulantes semble être d'un grand intérêt(1).
-------------------------------------
Background:
Haemorrhage is a common cause of death in trauma patients. Although transfusions are extensively used in the care of bleeding trauma patients, there is uncertainty about the balance of risks and benefits and how this balance depends on the baseline risk of death. Our objective was to evaluate the association of red blood cell (RBC) transfusion with mortality according to the predicted risk of death.
Methods and Findings:
A secondary analysis of the CRASH-2 trial (which originally evaluated the effect of tranexamic acid on mortality in trauma patients) was conducted. The trial included 20,127 trauma patients with significant bleeding from 274 hospitals in 40 countries. We evaluated the association of RBC transfusion with mortality in four strata of predicted risk of death: ,6%, 6%–20%, 21%–50%, and .50%. For this analysis the exposure considered was RBC transfusion, and the main outcome was death from all causes at 28 days. A total of 10,227 patients (50.8%) received at least one transfusion. We found strong evidence that the association of transfusion with all-cause mortality varied according to the predicted risk of death (p-value for interaction ,0.0001). Transfusion was associated with an increase in all-cause mortality among patients with , 6% and 6%–20% predicted risk of death (odds ratio [OR] 5.40, 95% CI 4.08–7.13, p,0.0001, and OR 2.31, 95% CI 1.96–2.73, p,0.0001, respectively), but with a decrease in all-cause mortality in patients with .50% predicted risk of death (OR 0.59, 95% CI 0.47–0.74, p,0.0001). Transfusion was associated with an increase in fatal and non-fatal vascular events (OR 2.58, 95% CI 2.05–3.24, p,0.0001). The risk associated with RBC transfusion was significantly increased for all the predicted risk of death categories, but the relative increase was higher for those with the lowest (,6%) predicted risk of death (p-value for interaction ,0.0001). As this was an observational study, the results could have been affected by different types of confounding. In addition, we could not consider haemoglobin in our analysis. In sensitivity analyses, excluding patients who died early; conducting propensity score analysis adjusting by use of platelets, fresh frozen plasma, and cryoprecipitate; and adjusting for country produced results that were similar.
Conclusions:
The association of transfusion with all-cause mortality appears to vary according to the predicted risk of death. Transfusion may reduce mortality in patients at high risk of death but increase mortality in those at low risk. The effect of transfusion in low-risk patients should be further tested in a randomised trial.
| Tags : hémorragie
22/12/2015
Tourniquet: Contrefaçons=Danger
Le regain d'intérêt pour la mise en place de garrot en cas d'hémorragie massive des membres ne doit pas faire oublier deux choses: Avoir appris correctement et utiliser un matériel adhoc.
Concernant ce dernier point apparaissent sur le marché nombre de garrots qui soit n'ont pas été validés soit sont des contrefaçons de ce dernier, soit des garrots proposés dans le cadre d'activité de type Softball.
Plutôt que d'utiliser un garrot de piêtre qualité, il vaut probablement mieux avoir recours à un garrot artisanal dont l'efficacité n'est pas remise en cause sous réserve d'une technique de pose maîtrisée.
On rappelle que les 3 seuls garrots validés par l'armée américaine sont le CAT, le SOFTT et le Delfi EMT. Les SEULS garrots en service dans l'armée française sont le SOFTT et le Delfi EMT. Ces garrots sont produits par des industriels au terme de travaux de recherche et de démarche d'évolution et de politique qualité aboutis, toutes démarches absentes chez les copieurs et les contrefacteurs.
Tous les autres garrots n'ont pas suivis les mêmes process de développement, ce qui ne permet pas de garantir ni leur efficacité dans le temps, ni leur fiabilité.
Un exemple de copie du SOFTT est ici présenté
Un point d'alerte majeur aux USA
| Tags : tourniquet
20/12/2015
Coagulopathie: Du fibrinogène avant tout
Trauma-induced coagulopathy: impact of the early coagulation support protocol on blood product consumption, mortality and costs
Nardi G et al. Critical Care (2015) 19:83
------------------------------------
Le damage control resuscitation fait largement appel à l'apport de plasma, concentrés de globules rouges et de plaquettes dans un rapport de 1/1/1 (1). Malgré la relative correction de la coagulopathie la survie à long terme ne semble pas être améliorée (2). Aussi certains proposent d'avoir plutôt recours à l'administration précoce de fibrinogène plutôt que l'administration de plasma. Le travail suivant qui propose l'apport précoce de 2g de fibrinogène est en faveur d'une telle démarche.
------------------------------------
INTRODUCTION:
Hemorrhage is the principal cause of death in the first few hours following severe injury. Coagulopathy is a frequent complication of critical bleeding. A network of Italian trauma centers recently developed a protocol to prevent and treat trauma-induced coagulopathy. A pre-post cohort multicenter study was conducted to assess the impact of the early coagulation support (ECS) protocol on blood products consumption,mortality and treatment costs.
METHODS:
We prospectively collected data from all severely injured patients (Injury Severity Score (ISS) >15) admitted to two trauma centers in 2013 and compared these findings with the data for 2011. Patients transfused with at least 3 units of packed red blood cells (PRBCs) within 24 hours of an accident were included in the study. In 2011, patients with significant hemorrhaging were treated with early administration of plasma with the aim of achieving a high (≥1:2) plasma-to-PRBC ratio. In 2013, the ECS protocol was the treatment strategy. Outcome data, blood product consumption and treatment costs were compared between the two periods.
RESULTS:
The two groups were well matched for demographics, injury severity (ISS: 32.9 in 2011 versus 33.6 in 2013) and clinical and laboratory data on admission. In 2013, a 40% overall reduction in PRBCs was observed, together with a 65% reduction in plasma and a 52% reduction in platelets. Patients in the ECS group received fewer blood products: 6.51 units of PRBCs versus 8.14 units. Plasma transfusions decreased from 8.98 units to 4.21 units (P <0.05), and platelets fell from 4.14 units to 2.53 units (P <0.05). Mortality in 2013 was 13.5% versus 20% in 2011 (13 versus 26 hospital deaths, respectively) (nonsignificant). When costs for blood components, factors and point-of-care tests were compared, a €76,340 saving in 2013 versus 2011 (23%) was recorded.
CONCLUSIONS:
The introduction of the ECS protocol in two Italian trauma centers was associated with a marked reduction in blood product consumption, reaching statistical significance for plasma and platelets, and with a non-significant trend toward a reduction in early and 28-daymortality. The overall costs for transfusion and coagulation support (including point-of-care tests) decreased by 23% between 2011 and 2013.
| Tags : coagulopathie
Brûlés: Pas plus de suicides que les autres ?
Postdischarge Cause-of-Death Analysis of Combat-Related Burn Patients
Escolas SM et Al. J Burn Care Res 2015;XXX:00–00
----------------------------------------------
Le document proposé rapporte le devenir des blessés brûlés par l'armée américiane lors des conflits afhgans et irakiens. Ces brûlés ont une surface moyenne relativement faible de l'ordre de 12% pour un ISS de 9 et une durée moyenne d'hospitalisation de 15 jours. La mortalité à long terme apparaît elle aussi plutôt faible de l'ordre de 1.3%. La brûlure ne serait donc pas un facteur aggravant notamment de suicide chez ces combattants. L'inclusion des ces combattants dans des programmes très structuré de réhabilitation et un lien social très fort expliquerait ces données.
----------------------------------------------
Combat operations in Iraq and Afghanistan have resulted in up to 8.8% of combat-related casualties suffering burns. From World War I through Desert Storm, burns have been associated with approximately 4% of the combat-related deaths. Experiencing a blast injury and exposure to killing and death while deployed has been shown to increase suicide risk. Although several studies of military populations have investigated risk factors for death among burn patients during the acute phase, no studies have reported mortality rates, cause-of-death, or the prevalence of suicide after hospital discharge. This study examined the case fatality rate, causes of death, and the prevalence of suicide among 830 combat burn patients discharged from the sole burn center in the U.S. Department of Defense, between March 7, 2003 and March 6, 2013. Cause-of-death was determined through the Armed Forces Medical Examiner’s Office and the Office of the Secretary of Defense’s National Death Index. A total of 11 deaths occurred among the 830 burn survivors, for an overall case fatality rate of 1.3%. Of the 11 who died, five deaths were related to accidental poisoning by exposure to drugs; three were related to operations of war (two after returning to the war zone), and the remaining three died from other accidental causes (one explosion and two vehicle crashes). There was no indication of suicide or suspicion of suicide as a cause-of-death for the former patients included in this study, suggesting that combat burn injury did not appear to increase the risk of death by suicide in our study population. Further research is needed to understand the factors that contribute to the apparent resilience of combat burn survivors.
| Tags : brûlure
19/12/2015
Military medicine in the 21st
Amputé des jambes: Le bassin aussi !
The incidence of pelvic fractures with traumatic lower limb amputation in modern warfare due to improvised explosive devices
Cross AM et Al. J R Nav Med Serv 2014;100(2):152-6
---------------------------------------------
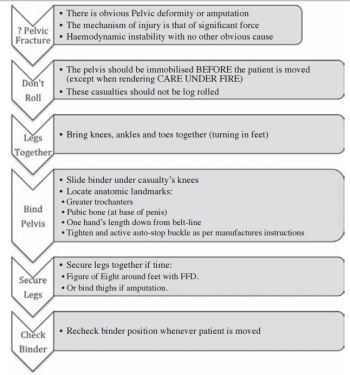
Excepté l'extraction d'urgence de blessés sous le feu, la prise en charge den cas d'amputation traumatique doit inclure la forte probabilité de traumatisme du bassin. Une utilisation large des immobilisations pelviennes doit donc être à l'esprit. On rappelle simplement la gravité et la difficulté de prise en charge des hémorragies liées aux fractures de bassin.
---------------------------------------------
AIMS:
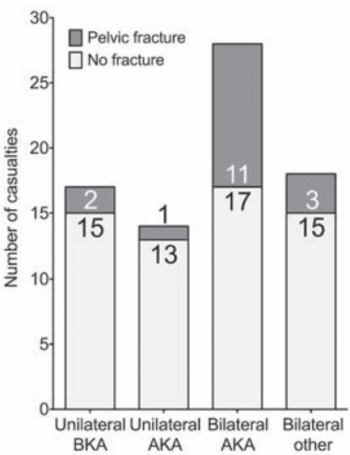
A frequently-seen injury pattern in current military experience is traumatic lower limb amputation as a result of improvised explosive devices (IEDs). This injury can coexist with fractures involving the pelvic ring. This study aims to assess the frequency of concomitant pelvic fracture in IED-related lower limb amputation.
METHODS:
A retrospective analysis of the trauma charts, medical notes, and digital imaging was undertaken for all patients arriving at the Emergency Department at the UK military field hospital in Camp Bastion, Afghanistan, with a traumatic lower limb amputation in the six months between September 2009 and April 2010, in order to determine the incidence of associated pelvic ring fractures.
RESULTS:
Of 77 consecutive patients with traumatic lower limb amputations, 17 (22%) had an associated pelvic fracture (eleven with displaced pelvic ring fractures, five undisplaced fractures and one acetabular fracture). Unilateral amputees (n = 31) had a 10% incidence of associated pelvic fracture, whilst 30 % of bilateral amputees (n = 46) had a concurrent pelvic fracture. However, in bilateral, trans-femoral amputations (n = 28) the incidence of pelvic fracture was 39%.
CONCLUSIONS:
The study demonstrates a high incidence of pelvic fractures in patients with traumatic lower limb amputations, supporting the routine pre-hospital application of pelvic binders in this patient group
| Tags : hémorragie, immobilisation, blast
18/12/2015
Ejector ventilator: Quésaco ?
Ventrain: an ejector ventilator for emergency use
Hamaekers AE et Al. Br J Anaesth. 2012 Jun;108(6):1017-21
----------------------------------------
La ventilation sur cathéter de coniotomie n'est pas chose aisée du fait de l'importance des résistances à l'écoulement des gaz dans un cathéter de petit diamètre. On considère que sans dispositif d'injection de type manujet, il faut un cathéter d'au moins 4 mm pour assurer un minimum acceptable. Certains ont proposé d'avoir recours à une expiration active. Il s'agissait de dispositifs expérimentaux. Ce n'est pas le cas du Ventrain qui apparaît être un produit abouti. A suivre
----------------------------------------
The Use of Ventrain from Ventinova Medical BV on Vimeo.
| Tags : coniotomie
17/12/2015
Médicaliser: Pour faire quoi ?
Doctor on board ? What is the optimal skill-mix in military pre-hospital care ?
Calderbank P. et Al. Emerg Med J (2010). doi:10.1136/emj.2010.097642
--------------------------------
Le document proposé à la lecture porte sur l'intérêt de la présence d'un médecin dans la plus avancée des structures medevac qui existe actuellement: Les MERT-E des anglais. Seule 1 medevac sur 5 justifiait la présence d'un médecin. L'intervention la plus fréquemment réalisée a été l'intubation/induction en séquence rapide. Bien loin devant d'autres gestes comme la thoracostomie ou le drainage thoracique. Ceci étant dit ce constat est fait dans un contexte spécifique afghan qui ne correspond pas aux opérations actuelles où les délais de prise en charge chirurgicales peuvent être long. Cette pratique est donc essentielle à maîtriser et procède d'une véritable stratégie de formation, avec une rythmicité semestrielle, débutée dès la formation initiale, associant un parcours structuré de mises à jour technique personnelle (passage en bloc opératoire, participation à des ateliers sur simulateurs de taches) et collective. Il s'agit d'un exemple parmi d'autres où une implication personnelle forte doit être présente.
--------------------------------
Background
In a military setting, pre-hospital times may be extended due to geographical or operational issues. Helicopter casevac enables patients to be transported expediently across all terrains. The skill-mix of the prehospital team can vary. Aim To quantify the doctors’ contribution to the Medical Emergency Response TeameEnhanced (MERT-E).
Methods
A prospective log of missions recorded urgency category, patient nationality, mechanism of injury, medical interventions and whether, in the crew’s opinion, the presence of the doctor made a positive contribution.
Results
Between July and November 2008, MERT-E flew 324 missions for 429 patients. 56% of patients carried were local nationals, 35% were UK forces. 22% of patients were T1, 52% were T2, 21.5% were T3 and 4% were dead. 48% patients had blast injuries, 25% had gunshot wounds, 6 patients had been exposed to blast and gunshot wounds. Median time from take-off to ED arrival was 44 min. A doctor flew on 88% of missions. It was thought that a doctor’s presence was not clinically beneficial in 77% of missions. There were 62 recorded physician’s interventions: the most common intervention was rapid sequence induction (45%); other interventions included provision of analgesia, sedation or blood products (34%), chest drain or thoracostomy (5%), and pronouncing life extinct (6%).
Conclusion
MERT-E is a high value asset which makes an important contribution to patient care. A relatively small proportion of missions require interventions beyond the capability of well-trained military paramedics; the indirect benefits of a physician are more difficult to quantify.
| Tags : airway
Tourniquet:Oui, mais bien posé= Serrer FORT
Evaluation of rapid training in ultrasound guided tourniquet application skills
Jaffer U. et Al. International Journal of Surgery 10 (2012) 563-567
-------------------------------------------------
Il existe actuellement un engouement justifié pour l'emploi du tourniquet comme moyen d'hémostase. Néanmoins il est important de rappeler que la pose d'un garrot a pour objectif l'arrêt d'un saignement important le plus souvent d'origine artérielle. Ils se doivent donc d'être serrés fort. Le travail proposé rappelle que la formation à la pose d'un garrôt n'est pas simplement sa manipulation mais qu'elle doit porter de manière spécifique sur les critères d'arrêt du saignement. En effet dans un modèle classique d'instruction de pose sur patient sain, les critères d'arrêt du serrage ne correspondent pas à ceux nécessaires en réel. Dans le travail proposé la pose à l'aveugle d'un garrot ne permet d'obtenir l'arrêt du saignement que dans moins d'1/4 à 1/5 des cas. Un enseignement donc à conduire par ceux qui en ont une pratique avancée. L'apport de simulateurs de saignement objectif comme celui du TOMMAN est certainement très intéressant.
Pour info: Fiche memento Garrot tactique
-------------------------------------------------
Tourniquet application has been widely accepted to improve survival for major limb trauma. Colour duplex ultrasound (US) can be used as a non-invasive method of confirming cessation of arterial flow. Participants with no or limited experience of ultrasound were taught to apply the Tourniquet with ultrasound guidance. Following this, participants were tested in effective tourniquet application: Blind and with ultrasound guidance. US guidance improved abolition of limb perfusion from 22 to 93 per cent in upper limb; from 25 to 100 per cent in lower limb (p ¼ 0.0027 and <0.0001).


Membre Sup Membre inf
No significant difference was found in application time for the lower limb; less time was taken for application with US guidance in the upper limb 8.1 (7.1, 8.6) vs 4.5 s (4.0, 5.3; median (IQR)), p ¼ 0.002. Tourniquet ultrasound skills are rapidly acquired by novice operators. Accuracy improves with ultrasound guidance, this may have a role in improving survival.
10/12/2015
L'enfant blessé balistique: Vraiment spécial
Prehospital interventions in severely injured pediatric patients: Rethinking the ABCs
Sokol KK et Al. J Trauma Acute Care Surg. 2015;79: 983-990
-----------------------------------------------
Des résultats qui ne sont pas surprenants mais qui confirme la spécificités des trauma ballistiques et l'inadéquation d'algorithmes issus de la traumatologie routière.
-----------------------------------------------
BACKGROUND: The current conflict in Afghanistan has resulted in a high volume of significantly injured pediatric patients. The austere environment has demanded emphasis on prehospital interventions (PHIs) to sustain casualties during transport.
METHODS: The Department of Defense Trauma Registry was queried for all pediatric patients (e18 years) treated at Camp Bastion from 2004 to 2012. PHIs were grouped by Advanced Trauma Life Support categories into (1) airway (A) intubation or surgical airway; 2) breathing (B) chest tube or needle thoracostomy; and 3) circulation (C) tourniquet or hemostatic dressing. Outcomes were assessed based on injury severity, hemodynamics, blood products and fluids, as well as mortality rates.
RESULTS: There were 766 injured children identified with 20% requiring one or more PHIs, most commonly circulation (C, 51%) followed by airway (A, 40%) and breathing (B, 8.7%). The majority of C interventions were tourniquets (85%) and hemostatic dressings (15%). Only 38% of patients with extremity vascular injury or amputation received a C intervention, with a significant reduction in blood products and intravenous fluids associated with receiving a C PHI (both p G 0.05). A interventions consisted of endotracheal intubation for depressed mental status (Glasgow Coma Scale [GCS] score G 8). Among patients with traumatic brain injury, A interventions were associated with higher unadjusted mortality (56% vs. 20%, p G 0.01) and remained independently associated with increased mortality after multivariate adjustment (odds ratio, 5.9; p = 0.001). B interventions were uncommon and performed in only 2% of patients with no recorded adverse outcomes.
CONCLUSION: There is a high incidence of PHIs among pediatric patients with severe wartime injuries. The most common and effective were C PHI for hemorrhage control, which should remain a primary focus of equipment and training. A interventions were most commonly performed in the setting of severe traumatic brain injury but were associated with worse outcomes. B interventions seem safe and effective and may be underused