19/08/2015
Simuler en haute fidélité: Pas si sûr !
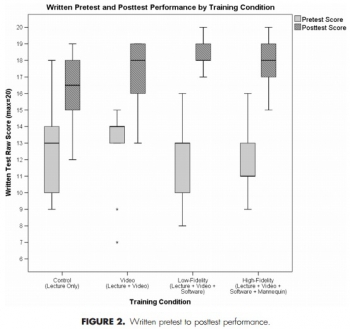
A Comparison of Teaching Modalities and Fidelity of Simulation Levels in Teaching Resuscitation Scenarios
Adams AJ et Al. J Surg Ed 2015, 72:778-785
-------------------------------
Il existe un très grand engouement pour le recours à la simulation haute fidélité, ce qui n'est pas sans impact financier. Un mannequin sophistiqué serait le gage d'une meilleure qualité de formation. Il semble que les bases scientifiques de ces démarches ne sont pas aussi solides que cela du moins pour les novices. Cet article a le mérite de montrer que l'on peut parfaitement conduire une formation de qualité avec des moyens plus conventionnels.
-------------------------------
Introduction
The purpose of our study was to examine the ability of novices to learn selected aspects of Advanced Cardiac Life Support (ACLS) in training conditions that did not incorporate simulation compared to those that contained low- and high-fidelity simulation activities. We sought to determine at what level additional educational opportunities and simulation fidelity become superfluous with respect to learning outcomes.
Methods
Totally 39 medical students and physician assistant students were randomly assigned to 4 training conditions: control (lecture only), video-based didactic instruction, low-, and high-fidelity simulation activities. Participants were assessed using a baseline written pretest of ACLS knowledge. Following this, all participants received a lecture outlining ACLS science and algorithm interpretation. Participants were then trained in specific aspects of ACLS according to their assigned instructional condition. After training, each participant was assessed via a Megacode performance examination and a written posttest.
Results
All groups performed significantly better on the written posttest compared with the pretest (p < 0.001); however, no groups outperformed any other groups. On the Megacode performance test, the video-based, low-, and high-fidelity groups performed significantly better than the control group (p = 0.028, p < 0.001, p = 0.019). Equivalence testing revealed that the high-fidelity simulation condition was statistically equivalent to the video-based and low-fidelity simulation conditions.
Conclusion
Video-based and simulation-based training is associated with better learning outcomes when compared with traditional didactic lectures only. Video-based, low-fidelity, and high-fidelity simulation training yield equivalent outcomes, which may indicate that high-fidelity simulation is superfluous for the novice trainee.
15/08/2015
Quel médecin en role 1 ?
Perceptions of Frontline Providers on the Appropriate Qualifi cations for Battalion Level Care in United States Army Ground Maneuver Forces
Malish RG et Al. Military Medicine, 176, 12:1369, 2011
--------------------------------
Il est habituel pour nous qu'un médecin déployé en role 1 soit un médecin généraliste. Ce n'est pas le cas dans d'autres armées notamment l'armée américaine où d'une part des spécialistes hospitaliers et d'autre part des officiers de santé ("physician assistant, souvent ancien combat medic) peuvent être déployés en role 1.
--------------------------------
Objectives:
Hypoxie d'altitude: Pour les AMET AUSSI !
Effects of Altitude-Related Hypoxia on Aircrews in Aircraft With Unpressurized Cabins
Nishi S. Military Medicine, 176, 1:79, 2011
--------------------------------------
La prise en charge de blessés en altitude ajoute à l'hémorragie le problème de l'hypoxie liée à la baisse de la PAO2 par baisse de la pression barométrique. Ceci joue aussi pour les sauveteurs, dès 1500 m, dont la performance peut être moindre avec une réduction de la capcité de concentration et une baisse d'acuité visuelle marquée à partir de 3000 m. Cela peut être le cas des équipes AMET dès lors que les cabines ne sont pas pressurisées
--------------------------------------
Introduction: Generally, hypoxia at less than 10,000 ft (3,048 m) has no apparent effect on aircrews. Nevertheless, several hypoxic incidents have been reported in flights below 10,000 ft. A recently introduced pulse oximeter using finger probes allows accurate monitoring of oxygen saturation (SPO 2 ) in the aeromedical environment. Using such a pulse oximeter, inflight SPO 2 levels were evaluated in aircrew in unpressurized aircraft. In addition, career in- flight hypoxic experiences were surveyed.
Methods: In-fl ight SPO 2 was measured in aircrews operating UH-60J helicopters at up to 13,000 ft, and 338 aircrew members operating unpressurized cabin aircraft were surveyed concerning possible in-fl ight hypoxic experiences.
Results: In aircrews operating UH-60J helicopters, SPO 2 decreased significantly at altitudes over 5,000 ft, most markedly at 13,000 ft (vs. ground level). The survey identified three aircrew members with experiences suggesting hypoxemia at below 5,000 ft.
Conclusions: Careful attention should be paid to the possibility of hypoxia in aircrews operating unpressurized cabin aircraft.
| Tags : altitude
12/08/2015
Airway: Pratiques UK en Helmand
A review of pre-admission advanced airway management in combat casualties, Helmand Province 2013
Pugh HE et Al. J R Army Med Corps. 2015 Jun;161(2):121-6.
--------------------------------------------
Il faut savoir intuber et ouvrir un cou. Ce qui fait la médicalisation de l'avant n'est pas la présence d'un docteur en médecine mais d'un professionnel de santé ayant la pratique de gestes de réanimation préhospitalière et capable de les mettre en oeuvre de faon opportune. La gestion des voies aériennes en est l'exemple.
--------------------------------------------
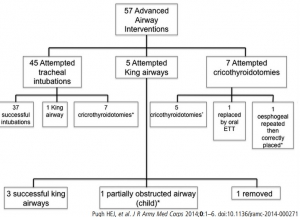
OBJECTIVES:
Airway compromise is the third leading cause of potentially preventable combat death. Pre-hospital airway management has lower success rates than in hospital. This study reviewed advanced airway management focusing on cricothyroidotomies and supraglottic airway devices in combat casualties prior to admission to a Role 3 Hospital in Afghanistan.
METHODS:
This was a retrospective review of all casualties who required advanced airway management prior to arrival at the Role 3 Hospital, Bastion, Helmand Province over a 30-week period identified by the US Joint Theatre Trauma Registry. The notes and relevant X-rays were analysed. The opinions of US and UK clinical Subject Matter Experts (SME) were then sought.
RESULTS:
Fifty-seven advanced airway interventions were identified. 45 casualties had attempted intubations, 37 (82%) were successful and of those who had failed intubations, one had a King LT Airway (supraglottic device) and seven had a rescue cricothyroidotomy. The other initial advanced airway interventions were five attempted King LT airways and seven attempted cricothyroidotomies. In total, 14 cricothyroidotomies were performed; in this group, there were nine complications/significant events.
CONCLUSIONS:
The SMEs suggested that dedicated surgical airway kits should be used and students in training should be taught to secure the cricothyroidotomy tube as well as how to insert it. This review re-emphasises the need to 'ensure the right person, with the right equipment and the right training, is present at the right time if we are to improve the survival of patients with airway compromise on the battlefield'. The audit reference number is RCDM/Res/Audit/1036/12/0368.
| Tags : airway
Drainer un thorax sans drain
Improvised Chest Tube Drain for Decompression of an Acute Tension Pneumothorax
Vinson ED Mil Med. 2004 May;169(5):403-5.
---------------------------------------
Décomprimer un thorax est indispensable en cas de pneumothorax suffocant. Si la décompression à l'aiguille est souvent présentée comme la technique de référence, encore faut il que sa réalisation soit faite par voie latérale avec un cathéter de calibre et longueur suffisant. Néanmoins cette technique est sujette à échec. La thoracostomie au doigt est la méthode la plus efficiente et la moins dangereuse. La justification de la pose d'un drain thoracique est moins claire: durée de transport conséquent, reconstitution du pneumothorax. Encore faut il avoir un drain.Si le cathéter du minitrach percut 2 peut être utilisé, c'est aussi le cas d'une ligne et d'une poche de perfusion qui semblent être une alternative à ne pas méconnaitre.
---------------------------------------
A case of a woman presenting with an acute tension pneumothorax during a Navy humanitarian mission in East Timor is presented. The patient was treated at a local rural clinic run by our medical team. Prompt insertion of a chest tube saved the woman’s life; however, there were no chest tube drains available. A field chest tube drain constructed out of an IV bag, a sterile water bottle, and tubing provided an adequate underwater seal and drain. Because of the remote location and limited resources, standard prehospital chest tube management had to be modified. A brief review of simple and tension pneumothoraces and management along with a description of the field chest tube drain is presented
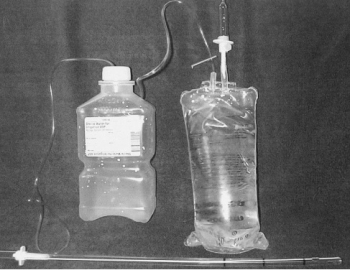
"The equipment needed includes a 24-French chest tube, a 100-mL NS IV bag, a 1,000-mL plastic sterile saline bottle, and two standard primary IV tube sets. The sterile water bottle is prepared by first emptying the contents. Next, two holes should be cut large enough to fit the surgical tubing, one in the cap, and one in the top of the bottle. The IV bag and primary IV tubing should be attached and the tube should be cut between the filter and reservoir. This end is left open for a vent. The other outlet port should be cut open to allow one end of a surgical tube to be inserted. The chest tube is then attached to the plastic spike of the other IV tubing. The other end of the tube is placed into the sterile water bottle through the hole in the cap. The surgical tube from the IV bag outlet port should be attached to the sterile water bottle through the hole in the side. The surgical tubing from the sterile water bag needs to be long enough to reach the top of the IV bag. To operate the system, the IV bag should be inverted to keep the underwater seal to the sterile water bottle. This allows the long tube to stay underwater while the short tube vents air out of the bag. To dispose of any accumulated fluid, the chest tube is first clamped near the patient. The water bottle can then be removed and emptied while the cap remains attached to the chest tube. It is then a simple matter to reattach the bottle and unclamp the chest tube"
| Tags : drainage thorax
10/08/2015
Célo: Au frigo, c'est vraiment mieux
Impact of Temperature Exposure on Stability of Drugs in a Real-World Out-of-Hospital Setting
De Winter S. et Al. Ann Emerg Med. 2013 Oct;62(4):380-387
------------------------------------------
Le maintien au frais des médicaments de l'urgence est réglementé. Malheureusement le maintien à +4c de plusieurs médicaments de l'urgence n'est pas toujours possible. Ce travail plutôt récent confirme la sensibilité des ces derniers aux conditions de stockage. Il faut donc dès lors envisager le renouvellement très régulier de ces produits quand ils sont stockés de manière non conforme aux spécifications des fabriquants et quand les conditions sont extrêmes avoir recours à des solutions de transports comme celui-ci
------------------------------------------
Study objective:
The aim of this study is to determine the content of 5 important emergency medical services
(EMS) drugs after being stored at the recommended refrigerated temperature, room temperature, or in an emergency physician transport vehicle operating under real-world working conditions.
Methods:
Adrenaline hydrochloride, cisatracurium besylate, lorazepam, methylergonovine maleate, and succinylcholine chloride were stored for 1 year under the 3 conditions. For each storage condition, samples of the drugs were taken after 1, 2, 3, and 4 weeks and after 2, 4, 6, 8, 10, and 12 months. For adrenaline hydrochloride, however, the samples were taken after 1, 2, 4, 6, 8, 10, and 12 months. The samples were analyzed with a validated high-performance liquid chromatography assay. A drug was considered stable if its content was above 90%.
Results:
Adrenaline hydrochloride and methylergonovine maleate remained stable for 1 year at room temperature and in the emergency physician transport vehicle. At room temperature and in the emergency physician transport vehicle, lorazepam became unstable within 4 weeks. Succinylcholine chloride was stable for 2 months at room temperature and for 1 month in the emergency physician transport vehicle. Cisatracurium besylate became unstable within 4 months at room temperature. However, it remained stable for 4 months in the emergency physician transport vehicle.
Conclusion:
When stored at room temperature or in the emergency physician transport vehicle, lorazepam became unstable within weeks, whereas succinylcholine chloride and cisatracurium besylate became unstable within months. Adrenaline hydrochloride and methylergonovine maleate remained stable for several months, even under room temperature and emergency physician transport vehicle conditions. Thus, real-world EMS working conditions pose challenges for maintaining optimal efficacy of these important EMS drugs.
07/08/2015
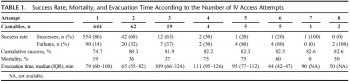
Intraosseux: Une place réelle à la guerre
Saving the critically injured trauma patient: a retrospective analysis of 1000 uses of intraosseous access
Lewis P et Al. Emerg Med J. 2015 Jun;32(6):463-7
OBJECTIVE:
Intraosseous access (IO) is becoming increasingly accepted in adult populations as an alternative to peripheral vascular access; however, there is still insufficient evidence in large patient groups supporting its use.
METHODS:
Retrospective review. This paper reports on the use of IO devices over a 7-year period from August 2006 to August 2013 during combat operations in Afghanistan. A database search of the Joint Theatre Trauma Registry (JTTR) was carried out looking for all the incidences of IO access use during this time. Excel (Microsoft) was used to manage the dataset and perform descriptive statistics on the patient demographics, injuries, treatments and complications that were retrieved.
RESULTS:
1014 IO devices were used in 830 adult patients with no major complications. The rate of minor complications, the majority of which were device failure, was 1.38%. 5124 separate infusions of blood products or fluids occurred via IO access, with 36% being of packed red cells. On average, each casualty received 6.95 different infusions of blood products and fluids, and 3.28 separate infusions of drugs through IO access. 32 different drugs were infused to 367 patients via IO, the most frequent being anaesthetic agents. IO access was used in the prehospital environment, during tactical helicopter evacuation and within hospitals.
CONCLUSIONS:
IO access can be used to administer a wide variety of life-saving medications quickly, easily and with low-complication rates. This highlights its valuable role as an alternative method of obtaining vascular access, vital when resuscitating the critically injured trauma patient.
| Tags : intraosseux
Intraosseux tibial: Pas l'idéal !
Intraosseous infusion rates under high pressure: a cadaveric comparison of anatomic sites
Pasley J et al. J Trauma Acute Care Surg 2015;78(2):295-9.
-------------------------------------------------
Dans notre pratique le choix d'un abord tibial est le plus fréquent mais certainement pas le plus pertinent chez l'adulte. Le taux de succès de 1ère pose, le débit atteint les les aléas de perfusion font qu'un abord huméral ou sternal sont un meilleur choix. C'est ce laisse supposer ce document.
-------------------------------------------------
BACKGROUND:
When traditional vascular access methods fail, emergency access through the intraosseous (IO) route can be lifesaving. Fluids, medications, and blood components have all been delivered through these devices. We sought to compare the performance of IO devices placed in the sternum, humeral head, and proximal tibia using a fresh human cadaver model.
METHODS:
Commercially available IO infusion devices were placed into fresh human cadavers: sternum (FAST-1), humeral head (EZ-IO), and proximal tibia (EZ-IO). Sequentially, the volume of 0.9% saline infused into each site under 300 mm Hg pressure over 5 minutes was measured. Rates of successful initial IO device placement and subjective observations related to the devices were also recorded.
RESULTS:
For 16 cadavers over a 5-minute bolus infusion, the total volume of fluid infused at the three IO access sites was 469 (190) mL for the sternum, 286 (218) mL for the humerus, and 154 (94) mL for the tibia. Thus, the mean (SD) flow rate infused at each site was as follows: (1) sternum, 93.7 (37.9) mL/min; (2) humerus, 57.1 (43.5) mL/min; and (3) tibia, 30.7 (18.7) mL/min. The tibial site had the greatest number of insertion difficulties.
CONCLUSION:
This is the first study comparing the rate of flow at the three most clinically used adult IO infusion sites in an adult human cadaver model. Our results showed that the sternal site for IO access provided the most consistent and highest flow rate compared with the humeral and tibial insertion sites. The average flow rate in the sternum was 1.6 times greater than in the humerus and 3.1 times greater than in the tibia.
| Tags : intraosseux
Intraosseux = Embolie graisseuse
Fat Intravasation from Intraosseous Flush and Infusion Procedures
Rubal BJ et Al. Prehosp Emerg Care. 2015 Jul-Sep;19(3):376-90
----------------------------------
On s'en doutait mais cela est objectivé: Le recours à la perfusion intraosseuse est responsable d'embolie graisseuse. La survenue d'une telle complication est moindre quand la procédure de flush ne dépasse pas 300mmHg et que le débit est lent. Dont acte au moins pour le flush.
----------------------------------
STUDY HYPOTHESIS:
The primary study objective was to delineate the procedural aspects of intraosseous (IO) infusions responsible for fatintravasation by testing the hypothesis that the fat content of effluent blood increases during IO infusions.
METHODS:
IO cannulas were inserted into the proximal tibiae of 35 anesthetized swine (Sus scrofa, 50.1 ± 3.5 kg) and intravasated fat was assessed using a lipophilic fluoroprobe (Nile red) and by vascular ultrasound imaging. Effluent blood bone marrow fat was assessed at baseline, during flush, and with regimens of controlled infusion pressures (73-300 mmHg) and infusion flow rates (0.3-3.0 mL per second). Fat intravasation was also assessed with IO infusions at different tibial cannulation sites and in the distal femur. In 7 animals, the lipid uptake of alveolar macrophages and lung tissue assessed for fat embolic burden using oil red O stain 24 hours post infusion. Additionally, bone marrow shear-strain was assessed radiographically with IO infusions.
RESULTS:
Fat intravasation was observed during all IO infusion regimens, with subclinical pulmonary fat emboli persisting 24 hours post infusion. It was noted that initial flush was a significant factor in fat intravasation, low levels of intravasation occurred with infusions ≤300 mmHg, fat intravasationand bone marrow shear-strain increased with IO infusion rates, and intravasation was influenced by cannula insertion site. Ultrasound findings suggest that echogenic particles consistent with fat emboli are carried in fast and slow venous blood flow fields. Echo reflective densities were observed to rise to the nondependent endovascular margins and coalesce in accordance with Stoke's law. In addition, ultrasound findings suggested that intravasated bone marrow fat was thrombogenic.
CONCLUSION:
Results suggest that in swine the intravasation of bone marrow fat is a common consequence of IO infusion procedures and that its magnitude is influenced by the site of cannulation and infusion forces. Although the efficacy and benefits of IO infusions for emergent care are well established, emergency care providers also should be cognizant that infusion procedures affect bone marrow fat intravasation.
| Tags : intraosseux
06/08/2015
Thoracostomie: ni en antérieur ou postérieur mais par voie latérale
Evaluation of the Risk of Intercostal Artery Laceration During Thoracentesis in Elderly Patients by Using 3D-CT Angiography
Yoneyama H. et Al Inter Med 49: 289-292, 2010
--------------------------------------------
Les artères intercostales ne cheminent pas toujours au rebord inférieur de de la côte supérieure. Il existe de plus des rameaux latéraux plutôt postérieurs. Donc il faut aborder le thorax par voie latérale. Une approche latérale au niveau des 4/5èmes espaces intercostaux sur la lgne axillaire moyennne est sécuritaire.
--------------------------------------------
Objective
Our study was undertaken to determine the location of the tortuous intercostal artery in elderly patients by using 3D-CT angiography in order to prevent laceration during thoracentesis.
Methods
We evaluated the data of 3D-CT angiography of the intercostal artery in consecutive patients who had undergone contrast chest CT scan in our hospital from December 2007 to April 2008. We considered the “percent safe space” (the shortest lower rib-to-intercostal artery distance/the upper rib-to-lower rib distance) to be an index of safety that can be used to prevent laceration of the intercostal artery during thoracentesis. We measured this index at 3 points: the total site (5-10 cm lateral to the spine), the lateral site (9-10 cm lateral to the spine), and the medial site (5-6 cm lateral to the spine).
Results
We evaluated 33 cases (25 males and 8 females; mean age, 74.2 years). The mean percent safe space at the total site was 58.6%. The percent safe space at the total site tended to decrease with advancing age, but the correlation was low (p=0.0378, r=-0.3631). The percent safe space at the lateral site (mean, 79.8%) was significantly higher than that at the medial site (61.2%, p<0.0001).
Conclusion
We showed that the intercostal artery is tortuous and does not always lie along the inferior edge of the rib and that the percent safe space at the lateral site is significantly higher than that at the medial site in elderly patients
| Tags : exsufflation
05/08/2015
Décompression à l'aiguille: Pas fiable
Does needle thoracostomy provide adequate and effective decompression of tension pneumothorax?
Martin M et Al. J Trauma Acute Care Surg. 2012;73: 1412-1417
-----------------------
La décompression thoracique est une des mesures qui vise à réduire le nombre de morts évitables. Il s'agit d'une procédure mise en oeuvre peu fréquemment. L'exsufflation à l'aiguille est la méthode enseignée. Il existe beaucoup de débats concernant le lieu de ponction (plutôt par voie axillaire et non par voie antérieure), la longueur du cathéter (certains proposent 8 cm au risque de ponction parenchymateuse et des gros vaisseaux), le diamètre. Le travail proposé est très intéressant car il exprime toute les réserves qui doivent encadrer ce geste qui ne semble pas aussi efficace que cela car outre les problèmes mécanique il apparaît bien qu'un cathéter de 14G risque d'être insuffisant. On rappelle quand même que la thoracostomie au doigt est toujours possible et que votre doigt a de fortes chances de mesurer 8 cm donc de pouvoir pénétrer dans un thorax après création d'un stomie intercostale à la pince de monro-kelly.
-----------------------
BACKGROUND:
Tension pneumothorax (tPTX) is a common and potentially fatal event after thoracic trauma. Needle decompression is the currently accepted first-line intervention but has not been well validated. The purpose of this study was to evaluate the effectiveness of a properly placed and patent needle thoracostomy (NT) compared with standard tube thoracostomy (TT) in a swine model of tPTX.
METHODS:
Six adult swine underwent instrumentation and creation of tPTX using thoracic CO2 insufflation via a balloon trocar. A continued 1 L/min insufflation was maintained to simulate an ongoing air leak. The efficacy and failure rate of NT (14 gauge) compared with TT (34F) was assessed in two separate arms: (1) tPTX with hemodynamic compromise and (2) tPTX until pulseless electrical activity (PEA) obtained. Hemodynamics was assessed at 1 and 5 minutes after each intervention.
RESULTS:
A reliable and highly reproducible tPTX was created in all animals with a mean insufflation volume of 2441 mL. tPTX resulted in the systolic blood pressure declining 54% from baseline (128Y58 mm Hg), cardiac output declining by 77% (7Y1.6 L/min), and equalization of central venous pressure and wedge pressures. In the first arm, there were 19 tPTX events treated with NT placement. All NTs were patent on initial placement, but 5 (26%) demonstrated mechanical failure (due to kinking, obstruction, or dislodgment) within 5 minutes of placement, all associated with hemodynamic decline. Among the 14 NTs that remained patent at 5 minutes, 6 (43%) failed to relieve tension physiology for an overall failure rate of 58%. Decompression with TTwas successful in relieving tPTX in 100%. In the second arm, there were 21 tPTX with PEA events treated initially with either NT (n = 14) or TT (n = 7). The NT failed to restore perfusion in nine events (64%), whereas TT was successful in 100% of events as a primary intervention and restored perfusion as a rescue intervention in eight of the nine NT failures (88%).
CONCLUSION: Thoracic insufflation produced a reliable and easily controlled model of tPTX. NT was associated with high failure rates for relief of tension physiology and for treatment of tPTX-induced PEA and was due to both mechanical failure and inadequate tPTX evacuation. This performance data should be considered in future NT guideline development and equipment design
| Tags : exsufflation, pneumothorax
04/08/2015
Exsufflation: Ø plutôt que longueur
Needle thoracostomy for tension pneumothorax: the Israeli Defense Forces experience
Chen J et Al. Can J Surg 2015;58(3):S118-S124
-----------------------------
Il existe un grand débat sur la nature du cathéter à utiliser pour décomprimer un thorx sous pression. Ce travail est intéressant car, alors qu'il existe une forte pression pour recourir à des cathéters de 8cm, il rapporte une expérience de terrain conséquente où le recours à un angiocath n'a pas été lié à un taux d'échec rédhibitoire puisque 8 fois sur 1 une amélioration clinique est notée. Pour ces auteurs le débat porte plus sur le diamètre du cathéter que sa longueur. Ce document insiste également sur la disparition unilatérale du murmure vésiculaire comme repère du côté à ponctionner.
-----------------------------
Contexte :
La thoracotomie à l’aiguille (TA) pour le pneumothorax sous tension sur les lieux mêmes du traumatisme peut sauver des vies. Des données récentes ont mis en doute l’efficacité des dispositifs de TA classiques. C’est pourquoi le corps médical de l’armée israélienne (CMAI) a récemment proposé un cathéter plus long, plus large et plus résistant pour décomprimer rapidement le pneumothorax. Le présent article résume l’expérience du CMAI en matière de décompression des pneumothorax au moyen de la TA.
Méthodes :
Nous avons passé en revue le registre des traumatismes de l’armée israé- lienne entre janvier 1997 et octobre 2012 pour relever tous les cas où une TA a été tentée.
Résultats :
Durant la période de l’étude 111 patients en tout ont subi une décompression à l’aide d’une TA. La plupart des cas (54 %) résultaient de blessures par balles; les accidents de la route venaient au second rang (16 %). La plupart (79 %) des TA ont été effectuées sur les lieux, tandis que les autres ont été effectuées durant l’évacuation par ambulance ou par hélicoptère (13 % et 4 %, respectivement). L’atténuation des bruits respiratoires du côté affecté était l’une des indications cliniques les plus fréquentes de la TA, enregistrée dans 28 % des cas. L’atténuation des bruits respiratoires était plus fréquente chez les patients qui ont survécu (37 % c. 19 %, p < 0,001). Un drain thoracique a été installé sur le terrain chez 35 patients (32 %), à chaque fois après une TA.
Conclusion :
La TA standard s’accompagne d’un taux d’échec élevé sur le champ de bataille. Une autre mesure de décompression, comme le cathéter Vygon, semble être une solution de rechange envisageable à la TA classique.
| Tags : exsufflation
Collier cervical: Pas utile ?
Cervical spine injury in dismounted improvised explosive device trauma
Taddeo j et Al. Can J Surg. 2015 Jun; 58(3 Suppl 3): S104–S107
-------------------------------
La mise en place d'un collier cervical est une mesure classique en traumaotlogie routière. Elle n'est cependant pas recommandée en cas de traumatisme d'origine ballistique. La probabilité de lésions instables du rachis semble faible surtout si il s'agit de blessures survenues lors de combat à pied et sans atteinte crânienne associée. L'étude présentée conforte cette position.
-------------------------------
Background
The injury pattern from improvised explosive device (IED) trauma is different if the target is in a vehicle (mounted) or on foot (dismounted). Combat and civilian first response protocols require the placement of a cervical collar on all victims of a blast injury.
Methods
We searched the Joint Theatre Trauma Registry (JTTR) and the Role 3 Hospital, Kandahar Airfield (KAF) database from Mar. 1, 2008, to May 31, 2011. We collected data on cervical fracture; head injury; traumatic amputation; initial blood pressure, pulse, injury severity score (ISS), Glasgow Coma Scale (GCS) score and base excess; and patient demographic information.
Results
The concordance rate between JTTR and KAF databases was 98%. Of the 15 693 admissions in JTTR, 326 patients with dismounted IED injuries were located. The rate of cervical collar prehospital placement was 7.6%. Cervical fractures were found in 19 (5.8%) dismounted IED victims, but only 4 (1.2%) were considered radiographically unstable. None of these 19 patients had prehospital placement of a collar. Patients with cervical spine fractures were more severely injured than those without (ISS 18.2 v. 13.4; GCS 10.1 v. 12.5). Patients with head injuries had significantly higher risk of cervical spine injury than those with no head injury recorded (13.6% v. 3.9%). No differences in frequency of cervical spine injury were found between patients who had associated traumatic amputations and those who did not (5.4% v. 6.0%).
Conclusion
Dismounted IED is a mechanism of injury associated with a low risk for cervical spine trauma. A selective protocol for cervical collar placement on victims of dismounted IED blasts is possible and may be more amenable to combat situations.
| Tags : rachis
03/08/2015
Accès veineux: Vision israélienne
Intravenous access in the prehospital settings: What can be learned from point-of-injury experience
Nadler R et Al. J Trauma Acute Care Surg. 2015;79: 221-226
-----------------------------------
La réalisation d'un abord vasculaire est un des gestes le plus souvent pratiqué. On rappelle qu'il s'agit là de pouvoir injecter certains médicaments (morphine, adrénaline, TXA, antibiotiques), d'initier un remplissage vasculaire raisonné voire d'administrer des dérives sanguins ou fractions coagulantes. Un document intéressant qui émane de l'armée israélienne fait le point sur cette pratique. Dans cette dernière (qui on le rappelle est assez spécifique compte tenu de la grande proximité des zones de combat et des structures hospitalières), il apparaît qu'il ne faille pas aller au delà de deux tentatives de pose de VVP au risque de retarder la prise en charge chirurgicale des blessés. Par ailleurs les taux de succès des médecins, combat medics et paramédics (pour nous nos infirmiers) soit superposable. Enfin la médiocre performance de l'accès intra-osseux doit interpeller.
-----------------------------------
BACKGROUND:
Intravenous (IV) access has an essential role in the care provided for trauma patients, allowing for transfusion of blood products, fluids, and drugs. Decisions should be made regarding the necessity of IV access while considering cost-benefit of the procedure in terms of delayed evacuation times.
METHODS:
A retrospective review of all trauma patients in whom at least one attempt at IVaccess was performed were reviewed. Data were abstracted from the Israeli Defense Force Trauma Registry.
RESULTS:
Of 7,476 patients, 1,082 patients who had at least one documented attempt at IV access between January 1997 and April 2013 were included in this study. Overall cumulative success rate at IV access was 82%. Success rates for IVaccess were 86%, 68%, 63%, 50%, 20% for the first, second, third, fourth, and fifth attempts, respectively. The first and second attempts accounted for 96% of the successful procedures. Mortality in patients for whom IV access was successful was 13%; mortality in patients for whom IV access was not successful was 35%.
CONCLUSION:
The success rate of IV access declined with each subsequent attempt. There was minimal improvement of overall success rate seen after the second attempt. Our findings suggest that the inability to obtain peripheral venous access is associated with severe injuries. These finding support a policy of limiting the number of venous access attempts to two attempts, followed by a reevaluation of need for parenteral access. Improved training of combat medics and paramedics might marginally increase the success rates of IVaccess. Point-of-injury data, used for ongoing learning and research, form the ground for improving combat casualty care and thus help saving lives.
| Tags : perfusion
02/08/2015
CICO: Un cours en ligne
| Tags : airway
01/08/2015
Milieu isolé: Mieux vaut avoir été préparé(e)
Preparing for Operations in a Resource-Depleted and/or Extended Evacuation Environment
Corey G et Al. J Spec Oper Med. 2013 Fall;13(3):74-80
The wars in Afghanistan and Iraq are the only conflicts to which many medics have ever been exposed. These mature theaters have robust medical systems that ensure rapid access to full-spectrum medical care for all combat-wounded and medically injured personnel. As current conflicts draw to a close, U.S. medics may be deployed to environments that will require the ability to stabilize casualties for longer than 1 hour. Historical mission analysis reveals the need to review skills that have not been emphasized during upgrade and predeployment training. This unit’s preparation for the extended care environment can be accomplished using a 4-point approach: (1) review of specific long-term skills training, (2) an extended care lab that reviews extended care skills and then lets the medic practice in a real-time scenario, (3) introduction to the HITMAN mnemonic tool, which helps identify and address patient needs, and (4) teleconsultation.
Simulation préhospitalière: Etat des lieux
Mapping the use of simulation in prehospital care - a literature review
Abelsson et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2014, 22:22
BACKGROUND:
High energy trauma is rare and, as a result, training of prehospital care providers often takes place during the real situation, with the patient as the object for the learning process. Such training could instead be carried out in the context of simulation, out of danger for both patients and personnel. The aim of this study was to provide an overview of the development and foci of research on simulation in prehospital care practice.
METHODS:
An integrative literature review were used. Articles based on quantitative as well as qualitative research methods were included, resulting in a comprehensive overview of existing published research. For published articles to be included in the review, the focus of the article had to be prehospital care providers, in prehospital settings. Furthermore, included articles must target interventions that were carried out in a simulation context.
RESULTS:
The volume of published research is distributed between 1984- 2012 and across the regions North America, Europe, Oceania, Asia and Middle East. The simulation methods used were manikins, films, images or paper, live actors, animals and virtual reality. The staff categories focused upon were paramedics, emergency medical technicians (EMTs), medical doctors (MDs), nurse and fire fighters. The main topics of published research on simulation with prehospital care providers included: Intubation, Trauma care, Cardiac Pulmonary Resuscitation (CPR), Ventilation and Triage.
CONCLUSION:
Simulation were described as a positive training and education method for prehospital medical staff. It provides opportunities to train assessment, treatment and implementation of procedures and devices under realistic conditions. It is crucial that the staff are familiar with and trained on the identified topics, i.e., intubation, trauma care, CPR, ventilation and triage, which all, to a very large degree, constitute prehospital care. Simulation plays an integral role in this. The current state of prehospital care, which this review reveals, includes inadequate skills of prehospital staff regarding ventilation and CPR, on both children and adults, the lack of skills in paediatric resuscitation and the lack of knowledge in assessing and managing burns victims. These circumstances suggest critical areas for further training and research, at both local and global levels.
| Tags : simulateurs