17/07/2019
Drainage thoracique chez l'enfant: La règle des 4
Rule of 4's: Safe and effective pleural decompression and chest drain insertion in severely injured children.
The intersecting scenarios of multi-trauma, thoracic injury and traumatic cardiac arrest present some of the most demanding moments in paediatric trauma. For these reasons, decision support through teamwork, checklists, technology and guidelines are central to ensuring quality paediatric trauma care. The 'Rule of 4's' is a simple aide-memoire, which guides clinicians of all grades, expertise and distractedness in a reliable approach to injured children who require safe and effective emergency pleural decompression and timely insertion of a chest drain.

The Rule of 4's enables these important therapeutic goals to be met through: (i) four steps in a 'good plan'; (ii) fourth (or fifth) intercostal space as the basis for siting a 'good hole'; (iii) 4× uncuffed endotracheal tube size (4× [age/4 + 4]) to guide selection of a 'good tube'; and (iv) 4 cm mark for a 'good stop' to ensure the drain is in far enough but not too far.
| Tags : drainage thorax
12/08/2015
Drainer un thorax sans drain
Improvised Chest Tube Drain for Decompression of an Acute Tension Pneumothorax
Vinson ED Mil Med. 2004 May;169(5):403-5.
---------------------------------------
Décomprimer un thorax est indispensable en cas de pneumothorax suffocant. Si la décompression à l'aiguille est souvent présentée comme la technique de référence, encore faut il que sa réalisation soit faite par voie latérale avec un cathéter de calibre et longueur suffisant. Néanmoins cette technique est sujette à échec. La thoracostomie au doigt est la méthode la plus efficiente et la moins dangereuse. La justification de la pose d'un drain thoracique est moins claire: durée de transport conséquent, reconstitution du pneumothorax. Encore faut il avoir un drain.Si le cathéter du minitrach percut 2 peut être utilisé, c'est aussi le cas d'une ligne et d'une poche de perfusion qui semblent être une alternative à ne pas méconnaitre.
---------------------------------------
A case of a woman presenting with an acute tension pneumothorax during a Navy humanitarian mission in East Timor is presented. The patient was treated at a local rural clinic run by our medical team. Prompt insertion of a chest tube saved the woman’s life; however, there were no chest tube drains available. A field chest tube drain constructed out of an IV bag, a sterile water bottle, and tubing provided an adequate underwater seal and drain. Because of the remote location and limited resources, standard prehospital chest tube management had to be modified. A brief review of simple and tension pneumothoraces and management along with a description of the field chest tube drain is presented
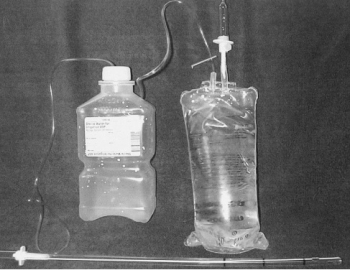
"The equipment needed includes a 24-French chest tube, a 100-mL NS IV bag, a 1,000-mL plastic sterile saline bottle, and two standard primary IV tube sets. The sterile water bottle is prepared by first emptying the contents. Next, two holes should be cut large enough to fit the surgical tubing, one in the cap, and one in the top of the bottle. The IV bag and primary IV tubing should be attached and the tube should be cut between the filter and reservoir. This end is left open for a vent. The other outlet port should be cut open to allow one end of a surgical tube to be inserted. The chest tube is then attached to the plastic spike of the other IV tubing. The other end of the tube is placed into the sterile water bottle through the hole in the cap. The surgical tube from the IV bag outlet port should be attached to the sterile water bottle through the hole in the side. The surgical tubing from the sterile water bag needs to be long enough to reach the top of the IV bag. To operate the system, the IV bag should be inverted to keep the underwater seal to the sterile water bottle. This allows the long tube to stay underwater while the short tube vents air out of the bag. To dispose of any accumulated fluid, the chest tube is first clamped near the patient. The water bottle can then be removed and emptied while the cap remains attached to the chest tube. It is then a simple matter to reattach the bottle and unclamp the chest tube"
| Tags : drainage thorax
09/06/2015
Faut il drainer avant de décoller: Non ?
Air Transport of Patients with Pneumothorax: Is Tube Thoracostomy Required Before Flight ?
Braude D et Al. Air Med J. 2014 Jul-Aug;33(4):152-6
Objective: It is conventionally thought that patients with pneumothorax (PTX) require tube thoracostomy (TT) before air medical transport (AMT), especially in unpressurized rotor-wing (RW) aircraft, to prevent deterioration from expansion of the PTX or development of tension PTX. We hypothesize that patients with PTX transported without TT tolerate RW AMT without serious deterioration, as defined by hypotension, hypoxemia, respiratory distress, intubation, bag valve mask ventilation, needle thoracostomy (NT), or cardiac arrest during transport.
Methods: We conducted a retrospective review of a case-series of trauma patients transported to a single Level 1 trauma center via RW with confirmed PTX and no TT. Using standardized abstraction forms, we reviewed charts for signs of deterioration. Those patients identified as having clinical deterioration were independently reviewed for the likelihood that the clinical deterioration was a direct consequence of PTX.
Results: During the study period, 66 patients with confirmed PTX underwent RW AMT with an average altitude gain of 1890 feet, an average barometric pressure 586-600 mmHg, and average flight duration of 28 minutes. All patients received oxygen therapy; 14/66 patients (21%) were supported with positive pressure ventilation. Eleven of 66 patients (17%) had NT placed before flight and 4/66 (6%) had NT placed during flight. Four of 66 patients (6% CI0.3-11.7) may have deteriorated during AMT as a result of PTX; all were successfully managed with NT.
Conclusions: In this series, 6% of patients with PTX deteriorated as result of AMT without TT, yet all patients were managed successfully with NT. Routine placement of TT in patients with PTX before RW AMT may not be necessary. Further prospective evaluation is warranted.
| Tags : pneumothorax, drainage thorax
13/11/2014
Drain thoracique: Confirmation, pas si simple
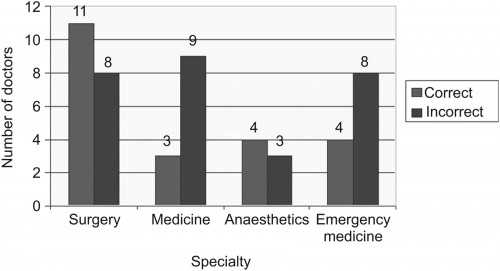
An audit of the complications of intercostal chest drain insertion in a high volume trauma service in South Africa.
Kong V. et All. Ann R Coll Surg Engl. 2014 Nov;96(8):609-13
Intercostal chest drain (ICD) insertion is a commonly performed procedure in trauma and may be associated with significant morbidity.
METHODS:
This was a retrospective review of ICD complications in a major trauma service in South Africa over a four-year period from January 2010 to December 2013.
RESULTS:
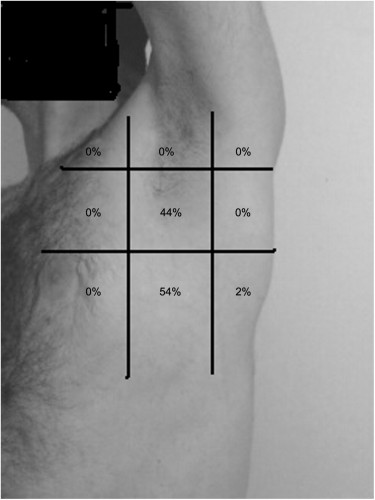
clic sur l'image pour accéder au document SAMU 69
A total of 1,050 ICDs were inserted in 1,006 patients, of which 91% were male. The median patient age was 24 years (interquartile range [IQR]: 20-29 years). There were 962 patients with unilateral ICDs and 44 with bilateral ICDs. Seventy-five per cent (758/1,006) sustained penetrating trauma and the remaining 25% (248/1006) sustained blunt trauma. Indications for ICD insertion were: haemopneumothorax (n=338), haemothorax (n=314), simple pneumothorax (n=265), tension pneumothorax (n=79) and open pneumothorax (n=54). Overall, 203 ICDs (19%) were associated with complications: 18% (36/203) were kinked, 18% (36/203) were inserted subcutaneously, 13% (27/203) were too shallow and in 7% (14/203) there was inadequate fixation resulting in dislodgement. Four patients (2%) sustained visceral injuries and two sustained vascular injuries. Forty-one per cent (83/203) were inserted outside the 'triangle of safety' but without visceral or vascular injuries. One patient had the ICD inserted on the wrong side. Junior doctors inserted 798 ICDs (76%) while senior doctors inserted 252 (24%). Junior doctors had a significantly higher complication rate (24%) compared with senior doctors (5%) (p<0.001). There was no mortality as a direct result of ICD insertion. </sec> Conclusions ICD insertion is associated with a high rate of complications. These complications are significantly higher when junior doctors perform the procedure. A multifaceted quality improvement programme is needed to improve the situation.
| Tags : drainage thorax
31/01/2012
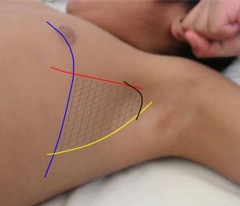
Le triangle de sécurité pour la thoracostomie
Chest drain insertion is not a harmless procedure – are we doing it safely ?
Elsayed H. et All. Interactive CardioVascular and Thoracic Surgery 11 (2010) 745–749
Près de la moitié des drains thoraciques ne sont pas posés au bon endroit
On rappelle la notion de triangle de sécurité (Le BTS Guideline)
http://www.surgeryjournal.co.uk/article/S0263-9319%2811%2...
La réalisation d'une thoracostomie au doigt et l'insertion d'un drain doit se faire de manière sécuritaire.
Le choix de la voie axillaire est certainement à privilégier.
| Tags : thorax, drainage thorax
26/12/2010
Drainage thoracique en images
Le drainage thoracique en condition de combat doit rester l'exception. Il peut se justifier en cas d'échec ou d'insuffisance de l'exsufflation ou de la thoracostomie au doigt. Il peut également s'envisager selon les conditions tactiques si le délai d'EVASAN es long. Le document ci-après présente de manière très didactique la réalisation de ce geste pas si anodin qu'il n'y paraît.
http://www.copacamu.org/IMG/pdf/3-roch.pdf
| Tags : drainage thorax, pneumothorax