26/02/2013
Combat en altitude: Le point de vue OTAN
24/02/2013
Intubation: Encore une étude POUR
Comparison of Neurological Outcome between Tracheal Intubation and Supraglottic Airway Device Insertion of Out-of-hospital Cardiac Arrest Patients: A Nationwide, Population-based, Observational Study
J Emerg Med. 2013 Feb;44(2):389-97
BACKGROUND:
The effect of prehospital use of supraglottic airway devices as an alternative to tracheal intubation on long-term outcomes of patients with out-of-hospital cardiac arrest is unclear.
STUDY OBJECTIVES:
We compared the neurological outcomes of patients who underwent supraglottic airway device insertion with those who underwent tracheal intubation.
METHODS:
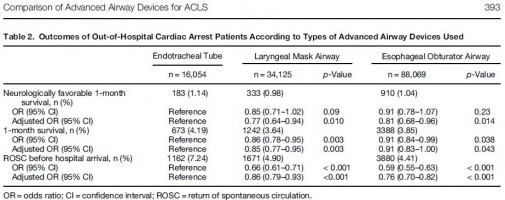
We conducted a nationwide population-based observational study using a national database containing all out-of-hospital cardiac arrest cases in Japan over a 3-year period (2005-2007). The rates of neurologically favorable 1-month survival (primary outcome) and of 1-month survival and return of spontaneous circulation before hospital arrival (secondary outcomes) were examined. Multiple logistic regression analyses were performed to adjust for potential confounders. Advanced airway devices were used in 138,248 of 318,141 patients, including an endotracheal tube (ETT) in 16,054 patients (12%), a laryngeal mask airway (LMA) in 34,125 patients (25%), and an esophageal obturator airway (EOA) in 88,069 patients (63%).
RESULTS:
The overall rate of neurologically favorable 1-month survival was 1.03% (1426/137,880). The rates of neurologically favorable 1-month survival were 1.14% (183/16,028) in the ETT group, 0.98% (333/34,059) in the LMA group, and 1.04% (910/87,793) in the EOA group. Compared with the ETT group, the rates were significantly lower in the LMA group (adjusted odds ratio 0.77, 95% confidence interval [CI] 0.64-0.94) and EOA group (adjusted odds ratio 0.81, 95% CI 0.68-0.96).
CONCLUSIONS:
Prehospital use of supraglottic airway devices was associated with slightly, but significantly, poorer neurological outcomes compared with tracheal intubation, but neurological outcomes remained poor overall.
| Tags : airway, intubation
21/02/2013
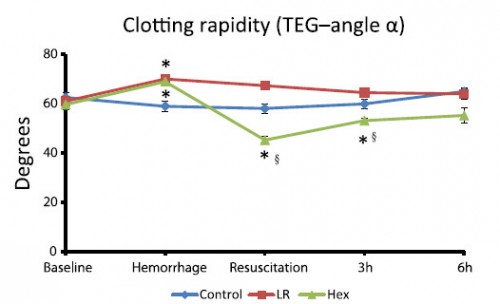
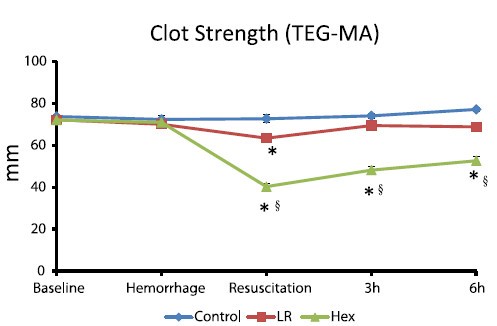
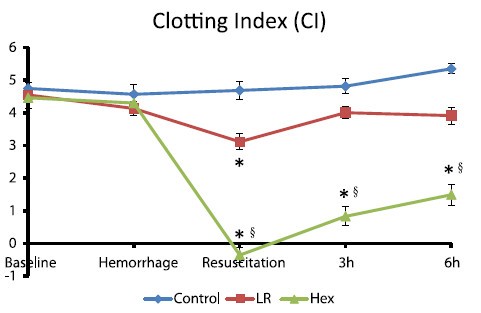
Pour la coagulation: HEA de haut PM pas bon ?
Comparisons of lactated Ringer’s and Hextend resuscitation on hemodynamics and coagulation following femur injury and severe hemorrhage in pigs
Wenjun Z et all J Trauma Acute Care Surg. 2013;74: 732-740
After traumatic hemorrhage, coagulation function was restored within 6 hours with LR resuscitation but not with Hextend. The lack of recovery after Hextend is likely caused by greater hemodilution and possible effects of starches on coagulation substrates and further documents the need to restrict the use of high-molecular-weight starch in resuscitation fluids for bleeding casualties.
On rappelle que l'Hextend est un HEA 670/0.75 et que le voluven est un HEA 130/0,4 dont les effets sur la coagulation sont réputées étant moindres.
| Tags : coagulopathie, remplissage, hémorragie
18/02/2013
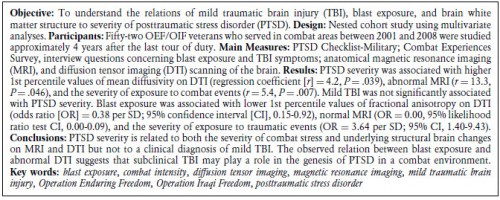
PTSD et Mild TBI: Convergence à l'IRM
The Relation Between Posttraumatic Stress Disorder and Mild Traumatic Brain Injury Acquired During Operations Enduring Freedom and Iraqi Freedom
| Tags : ptsd, psychiatrie
17/02/2013
Ballistic trauma. A practical guide
| Tags : balistique
09/02/2013
Paludisme: Directives 2012 pour le traitement
Les dérivés de l'artémisine sont recommandés avant la quinine pour le traitement des formes graves. Des schémas de traitement avant transfert ayant recours à la voie intrarectale sont proposés.
Le paludisme grave en pages 39 à 53
04/02/2013
Causes de mortalité: Actualisation 2012
Death on the battlefield (2001Y2011): Implications for the future of combat casualty care
Eastridge BJ et all. J Trauma Acute Care Surg. 2012;73: S431YS437
BACKGROUND:Critical evaluation of all aspects of combat casualty care, including mortality, with a special focus on the incidence and causes of potentially preventable deaths among US combat fatalities, is central to identifying gaps in knowledge, training, equipment, and execution of battlefield trauma care. The impetus to produce this analysis was to develop a comprehensive perspective of battlefield death, concentrating on deaths that occurred in the preYmedical treatment facility (pre-MTF) environment.
METHODS:The Armed Forces Medical Examiner Service Mortality Surveillance Division was used to identify Operation Iraqi Freedom and Operation Enduring Freedom combat casualties from October 2001 to June 2011 who died from injury in the deployed environment. The autopsy records, perimortem records, photographs on file, and Mortality Trauma Registry of the Armed Forces Medical Examiner Service were used to compile mechanism of injury, cause of injury, medical intervention performed, Abbreviated Injury Scale (AIS) score, and Injury Severity Score (ISS) on all lethal injuries. All data were used by the expert panel for the conduct of the potential for injury survivability assessment of this study.
RESULTS:For the study interval between October 2001 and June 2011, 4,596 battlefield fatalities were reviewed and analyzed. The stratification of mortality demonstrated that 87.3% of all injury mortality occurred in the pre-MTF environment. Of the pre-MTF deaths, 75.7% (n = 3,040) were classified as nonsurvivable, and 24.3% (n = 976) were deemed potentially survivable (PS). The injury/physiologic focus of PS acute mortality was largely associated with hemorrhage (90.9%). The site of lethal hemorrhage was truncal (67.3%), followed by junctional (19.2%) and peripheral-extremity (13.5%) hemorrhage.
CONCLUSION:Most battlefield casualties died of their injuries before ever reaching a surgeon. As most pre-MTF deaths are nonsurvivable, mitigation strategies to impact outcomes in this population need to be directed toward injury prevention. To significantly impact the outcome of combat casualties with PS injury, strategies must be developed to mitigate hemorrhage and optimize airway management or reduce the time interval between the battlefield point of injury and surgical intervention. Understanding battlefield mortality is a vital component of the military trauma system. Emphasis on this analysis should be placed on trauma system optimization, evidence-based improvements in Tactical Combat Casualty Care guidelines, data-driven research, and development to remediate gaps in care and relevant training and equipment enhancements that will increase the survivability of the fighting force. (J Trauma Acute Care Surg. 2012;73: S431YS437. Copyright * 2012 by Lippincott Williams & Wilkins
Le CROC: Une validation expérimentale
Assessment of users to control simulated junctional hemorrhage with the combat ready clamp (CRoC™).
Mann-Salinas EA et all. Int J Burn Trauma 2013;3(1):49-54
The Combat Ready Clamp (CRoC™) was designed to control hemorrhage from the groin region, on the battlefield. The purpose of this experiment was to determine whether CRoC™ user performance varied by the surface the casualty laid on (flat-hard, flat-soft, and curved-soft) and how quickly the device could be applied. The commercial manikin selected to assess user performance was designed to train soldiers in CRoC™ use. The manikin simulated severe hemorrhage from an inguinal wound, controllable by correct use of the CRoC™. Each individual (n = 6) performed 3 iterations on each of the 3 surfaces (54 iterations total). The CRoC™ achieved hemorrhage control 100% of the time (54/54). Patient surface affected time to stop bleeding. The flat-soft surface (padded, 55 ± 9.7 seconds) was significantly different from the curved-soft surface (litter, 65 ± 16.5 seconds) and had the lowest overall total time (p = 0.007); time for the hard-flat surface was 58 ± 9.5 seconds. Users were trained to use the Combat Ready Clamp effectively, and the surface the casualty was lying on made some difference to user performance. All six persons trained had success in all nine of their iterations of CRoC™ use– a 100% rate. These findings indicate that training was effective and that training of other users is plausible, feasible, and practical within the scope of the present evidence.