21/06/2015
Pneumothorax en vol: Merci l'écho
In-flight thoracic ultrasound detection of pneumothorax in combat
Madill JJ J Emerg Med. 2010 Aug;39(2):194-7
-----------------------------------------------
Ce cas clinique est intéressant car il démontre que le recours à l'échographie est dans ce cas non seulement possible mais indispensable compte tenu des difficultés d'auscultation en vol. Ceci étant dit il faut cependant être bien conscient du caractère opérateur dépendant de l'échographie qui peut être peu parlante et nécessiter donc une pratique réelle au delà d'une simple formation à la FAST échographie
-----------------------------------------------
Background: Ultrasonography is the only portable imaging modality available in the helicopter medical evacuation environment where physical examination is limited, auscultation is impossible, long transport times may occur, and altitude variations are frequent. Although the use of ultrasonography by aviation medical personnel has been documented, minimal literature exists on the contribution of in-flight ultrasonography to patient management. Objectives: This case demonstrates an indication for the use of in-flight ultrasonography. It shows how it can affect in-flight management and direct lifesaving intervention.
Case Report: A patient with blast injury developed hemodynamic instability of unclear etiology during transport in the combat aviation environment. To our knowledge, this is the first reported case where in-flight thoracic ultrasonography augmented physical examination and diagnosed an untreated pneumothorax when auscultation was impossible. It directed the decision to perform in-flight procedural intervention with tube thoracostomy. This rapidly improved the patient’s hemodynamic stability in a remote and hostile setting.
Conclusion: In-flight thoracic ultrasonography is a portable imaging tool that can be used by aviation medical personnel to detect pneumothorax in environments where physical examination is limited and auscultation is impossible
| Tags : pneumothorax, échographie
03/04/2015
Echographiste en quelques heures ?
Limited intervention improves technical skill in focus assessed transthoracic echocardiography among novice examiners.
Frederiksen et al. BMC Med Educ. 2012 Aug 3;12:65
-------------------------------------------------------------------
La généralisation de l'échographie est une avancée majeure. Mais comment apprendre ? La pratique de l'échographie ciblée se développe notamment en médecine d'urgence. A côté des formations classiques de type DU existent de nombreuses formations de courte durée, certaines de quelques heures. Le travail présenté met en évidence qu'un tel type de formation permet une manipulation relativement fiable des équipements et l'obtention de coupes sonographiques propres à être interprétées. On notera que ceci est obtenu A CONDITION qu'au moins 10 examens supervisés soient conduits, ce qui n'est souvent pas fait avec suffisamment de rigueur dans ce que nous pouvons proposer actuellement. Par ailleurs voir et interpréter de manière fiable ne sont pas superposables (1).
-------------------------------------------------------------------
BACKGROUNDS:
Previous studies addressing teaching and learning in point-of-care ultrasound have primarily focussed on image interpretation and not on the technical quality of the images. We hypothesized that a limited intervention of 10 supervised examinations would improve the technical skills in Focus Assessed Transthoracic Echocardiography (FATE) and that physicians with no experience in FATE would quickly adopt technical skills allowing for image quality suitable for interpretation.
METHODS:
Twenty-one physicians with no previous training in FATE or echocardiography (Novices) participated in the study and a reference group of three examiners with more than 10 years of experience in echocardiography (Experts) was included. Novices received an initial theoretical and practical introduction (2 hours), after which baseline examinations were performed on two healthy volunteers. Subsequently all physicians were scheduled to a separate intervention day comprising ten supervised FATE examinations. For effect measurement a second examination (evaluation) of the same two healthy volunteers from the baseline examination was performed.
RESULTS:
At baseline 86% of images obtained by novices were suitable for interpretation, on evaluation this was 93% (p = 0.005). 100% of images obtained by experts were suitable for interpretation. Mean global image rating on baseline examinations was 70.2 (CI 68.0-72.4) and mean global image rating after intervention was 75.0 (CI 72.9-77.0), p = 0.0002. In comparison, mean global image rating in the expert group was 89.8 (CI 88.8-90.9).
CONCLUSIONS:
Improvement of technical skills in FATE can be achieved with a limited intervention and upon completion of intervention 93% of images achieved are suitable for clinical interpretation.
| Tags : échographie
31/03/2015
Focus assessed transthoracic Echo (FATE)
Un document pdf qui synthétise les données à connaître pour l'examen échographique cardio-respiratoire. Une approche standardisée appelée est visualisable ici.
| Tags : échographie
24/03/2015
Airway et Echographie
| Tags : airway, échographie
22/03/2015
L'échographie: Investir de son temps pour avoir une pratique fiable
Ultrafest: A Novel Approach to Ultrasound in Medical Education Leads to Improvement in Written and Clinical Examinations
Connolly K et All. West J Emerg Med. 2015 Jan;16(1):143-8.
----------------------------------------------------------------------------------
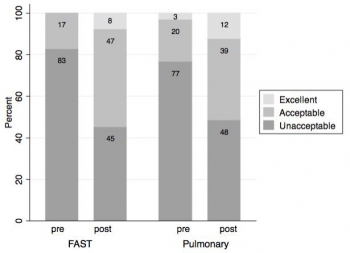
L'apprentissage de l'échographie est un impératif en médecine d'urgence. Cependant une véritable qualification ne peut être obtenue qu'au travers de formations universitaires assorties de pratiques réelles et régulières. La pratique des certains protocoles simplifiés comme le FAST serait d'acquisition plus simples. Aussi sont souvent proposées des formations de courtes durées. Ces dernières semblent en théorie très intéressantes en contexte militaire. Une analyse raisonnée de la réalité doit tempérer cet enthousiasme. Le travail présenté montre que si les connaissances théoriques des étudiants sont améliorées par une formation d'une journée, cette dernière ne permet pas l'acquisition d'une pratique suffisamment fiable. Ainsi la formation de nos personnels, qui repose souvent sur des formations de courtes durée, doit elle vue comme une découverte de cette pratique et non pas comme permettant l'acquisition d'un réel savoir faire.
Introduction:
Our objective was to evaluate the effectiveness of hands-on training at a bedside ultrasound (US) symposium (“Ultrafest”) to improve both clinical knowledge and image acquisition skills of medical students. Primary outcome measure was improvement in multiple choice questions on pulmonary or Focused Assessment with Sonography in Trauma (FAST) US knowledge. Secondary outcome was improvement in image acquisition for either pulmonary or FAST.
Methods:
Prospective cohort study of 48 volunteers at “Ultrafest,” a free symposium where students received five contact training hours. Students were evaluated before and after training for proficiency in either pulmonary US or FAST. Proficiency was assessed by clinical knowledge through written multiple-choice exam, and clinical skills through accuracy of image acquisition. We used paired sample t-tests with students as their own controls.
Results:
Pulmonary knowledge scores increased by a mean of 10.1 points (95% CI [8.9-11.3], p<0.00005), from 8.4 to a posttest average of 18.5/21 possible points. The FAST knowledge scores increased by a mean of 7.5 points (95% CI [6.3-8.7] p<0.00005), from 8.1 to a posttest average of 15.6/ 21. We analyzed clinical skills data on 32 students. The mean score was 1.7 pretest and 4.7 posttest of 12 possible points. Mean improvement was 3.0 points (p<0.00005) overall, 3.3 (p=0.0001) for FAST, and 2.6 (p=0.003) for the pulmonary US exam.
Conclusion:
This study suggests that a symposium on US can improve clinical knowledge, but is limited in achieving image acquisition for pulmonary and FAST US assessments. US training external to official medical school curriculum may augment students’ education
| Tags : échographie
07/01/2015
Gonflez le ballonnet à l'eau et échographiez le au niveau de la fourchette sternale !
Tracheal rapid ultrasound saline test (T.R.U.S.T.) for confirming correct endotracheal tube depth in children
Tessaro MO et Al. Resuscitation. 2014 Sep 17. pii: S0300-9572(14)00741-2
------------------------------------------------------------------------------------
On parle beaucoup de l'apport de l'échographie en préhospitalier et plus particulièrement de l'échographie des voies aériennes. Ce travail réalisé dans un contexte de pédiatrie hospitalière est intéressant car il peut peut-être être transposé à nos besoins. Etre rapidement certain du caractère effectif de l'intubation peut être difficile. L'échographie peut être d'un apport important par la visualisation d'un glissement pleural bilatéral. On peut aussi gonfler le ballonnet de la sonde [Ce qui est fait lors de transports aériens non ou mal préssurisés], ce qui permettra d'observer non un cône d'ombre en arriere du ballonnet mais les structures anatomiques du fait de la transmissions des ondes permise par l'eau présente dans le ballonnet.
------------------------------------------------------------------------------------
OBJECTIVES:
We evaluated the accuracy of tracheal ultrasonography of a saline-inflated endotracheal tube (ETT) cuff for confirming correct ETT insertion depth.
METHODS:
We performed a prospective feasibility study of children undergoing endotracheal intubation for surgery. Tracheal ultrasonography at the suprasternal notch was performed during transient endobronchial intubation and inflation of the cuff with saline, and with the ETT at a correct endotracheal position. Ultrasound videos were recorded at both positions, which were confirmed by fiberoptic bronchoscopy. These videos were shown to two independent blinded reviewers, who determined the presence or absence of a saline-inflated cuff. The primary outcome was accuracy of tracheal ultrasonography for appropriate ETT insertion depth.
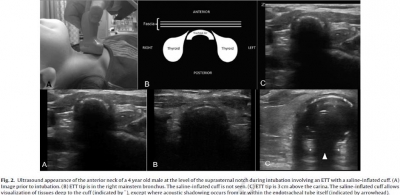
RESULTS:
Forty-two patients were enrolled. For correct endotracheal versus endobronchial positioning, pooled results from the reviewers revealed a sensitivity of 98.8% (95% CI=90-100%), a specificity of 96.4% (95% CI=87-100%), a PPV of 96.5% (95% CI=87-100%), a NPV of 98.8% (95% CI=89-100%), a positive likelihood ratio of 32 (95% CI=6-185), and a negative likelihood ratio of 0.015 (95% CI=0.004-0.2). Agreement between reviewers was high (kappa co-efficient=0.93; 95% CI=0.86 to 1). The mean duration of the ultrasound exam was 4.0s (range 1.0-15.0s).
CONCLUSIONS:
Sonographic visualization of a saline-inflated ETT cuff at the suprasternal notch is an accurate and rapid method for confirming correct ETT insertion depth in children.
| Tags : airway, intubation, échographie
10/12/2014
Echographie: 10 bonnes raisons POUR
Ten good reasons to practice ultrasound in critical care
Lichtenstein D. et AL Anaesthesiol Intensive Ther. 2014 Nov-Dec;46(5):323-35
-----------------------------------------------------------------
Le document proposé est une réflexion faite par un des promoteurs mondial de l'échographie pulmonaire. Il s'agit donc d'un document référence à lire en cliquant sur le lien proposé dans le titre.
-----------------------------------------------------------------
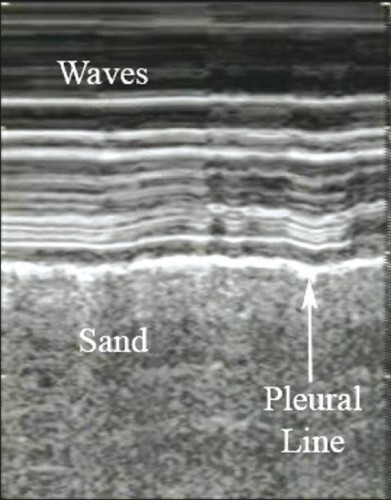
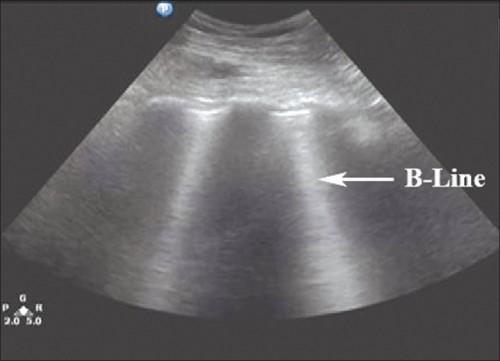
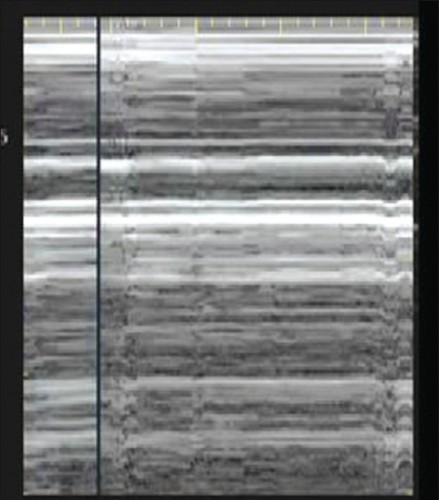
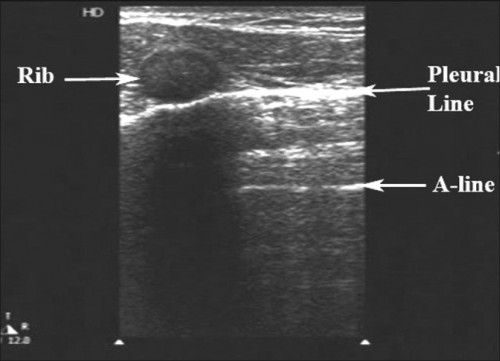
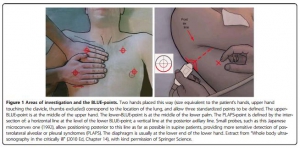
Over the past decade, critical care ultrasound has gained its place in the armamentarium of monitoring tools. A greater understanding of lung, abdominal, and vascular ultrasound plus easier access to portable machines have revolutionised he bedside assessment of our ICU patients. Because ultrasound is not only a diagnostic test, but can also be seen as a component of the physical exam, it has the potential to become the stethoscope of the 21st century. Critical care ultrasound is a combination of simple protocols, with lung ultrasound being a basic application, allowing assessment of urgent diagnoses in combination with therapeutic decisions. The LUCI (Lung Ultrasound in the Critically Ill) consists of the identification of ten signs: the bat sign (pleural line); lung sliding (seashore sign); the A-lines (horizontal artefact); the quad sign and sinusoid sign indicating pleural effusion; the fractal and tissue-like sign indicating lung consolidation; the B-lines and lung rockets indicating interstitial syndromes; abolished lung sliding with the stratosphere sign suggesting pneumothorax; and the lung point indicating pneumothorax. Two more signs, the lung pulse and the dynamic air bronchogram, are used to distinguish atelectasis from pneumonia. The BLUE protocol (Bedside Lung Ultrasound in Emergency) is a fast protocol (< 3 minutes), also including a vascular (venous) analysis allowing differential diagnosis in patients with acute respiratory failure. With this protocol, it becomes possible to differentiate between pulmonary oedema, pulmonary embolism, pneumonia, chronic obstructive pulmonary disease, asthma, and pneumothorax, each showing specific ultrasound patterns and profiles. The FALLS protocol (Fluid Administration Limited by Lung Sonography) adapts the BLUE protocol to be used in patients with acute circulatory failure. It makes a sequential search for obstructive, cardiogenic, hypovolemic, and distributive shock using simple real-time echocardiography in combination with lung ultrasound, with the appearance of B-lines considered to be the endpoint for fluid therapy. An advantage of lung ultrasound is that the patient is not exposed to radiation, and so the LUCI-FLR project (LUCI favouring limitation of radiation) can be unfolded in trauma patients. Although it has been practiced for 25 years, critical care ultrasound is a relatively young but expanding discipline and can be seen as the stethoscope of the modern intensivist. In this review, the usefulness and advantages of ultrasound in the critical care setting are discussed in ten points. The emphasis is on a holistic approach, with a central role for lung ultrasound.
| Tags : échographie
07/12/2014
Echographe et situation isolée: Quid en 2013 ?
Ultrasound in the Austere Environment: A Review of the History, Indications, and Specifications
Russel TC et AL. Military Medicine, 178, 1:21, 2013
----------------------------------------------------------------------------------
L'échographie s'est très largement démocratisée et du fait des améliorations technologiques continues est en passe de devenir un outil incontournable non seulement en médecine d'urgence (1) mais tout simplement en médecine générale. La maîtrise de cette pratique est donc incontournable pour tout médecin militaire projeté. Cependant connaître une technique et la maîtriser sont deux choses différentes, c'est dire l'importance non seulement de la nature des formations initiales et surtout des modalités de maintien des compétences (2). Intégrer cet outil dans son raisonnement clinique impose une réflexion personnelle sur son niveau d'expertise comme celui de pouvoir réaliser de manière fiable l'acquisition de toutes les coupes d'une FAST Echo en 5 min. D'autres indications plus médicales sont bien réelles voire même plus fréquentes. Très certainement, le recours à des outils de simulation trouvera très rapidement une place (3)
----------------------------------------------------------------------------------
In the last 10 years, the use of ultrasound has expanded because of its portability, safety, real-time image display, and rapid data collection. Simultaneously, more people are going into the backcountry for enjoyment and employment. Increased deployment for the military and demand for remote medicine services have led to innovative use and study of ultrasound in extreme and austere environments. Ultrasound is effective to rapidly assess patients during triage and evacuation decision making. It is clinically useful for assessment of pneumothorax, pericardial effusion, blunt abdominal trauma, musculoskeletal trauma, high-altitude pulmonary edema, ocular injury, and obstetrics, whereas acute mountain sickness and stroke are perhaps still best evaluated on clinical grounds. Ultrasound performs well in the diverse environments of space, swamp, jungle, mountain, and desert. Although some training is necessary to capture and interpret images, real-time evaluation with video streaming is expected to get easier and cheaper as global communications improve. Although ultrasound is not useful in every situation, it can be a worthwhile tool in the austere or deployed environment.
| Tags : échographie
02/12/2014
Echo: Quels requis ?
L’échographie ciblée en médecine d’urgence. Nouvelles normes et applications avancées. Position conjointe de l’Association des médecins d’urgence du Québec (AMUQ) et de l’Association des spécialistes en médecine d’urgence du Québec (ASMUQ) adoptée le 7 novembre 2012
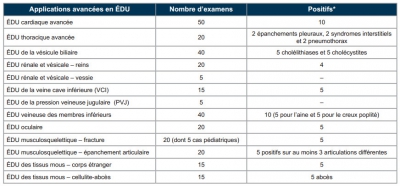
La pratique de l'échographie aux urgences est très régulière. Si des formations courtes permettent un apprentissage rapide de techniques de débrouillage comme la FAST Echo, seule une pratique régulière encadrée permet l'acquisition d'une véritable expertise. Le tableau présenté rappelle les prérequis nécessaires à un exercice indépendant chez nos cousins québécois.
| Tags : échographie
22/11/2014
Echographie en role2/3
Trauma resuscitation using echocardiography in a deployed military intensive care unit
Hutchings Sj et Al. JICS 2013:14, 120-125
30/10/2014
The Blue protocol
Lung ultrasound in the critically ill
Lichtenstein D. Annals of Intensive Care 2014, 4:1
Une approche systématisée de l'échographie pulmonaire simpllfie et fiabilise cet examen. C'est ce qu'explique cette publication
24/06/2013
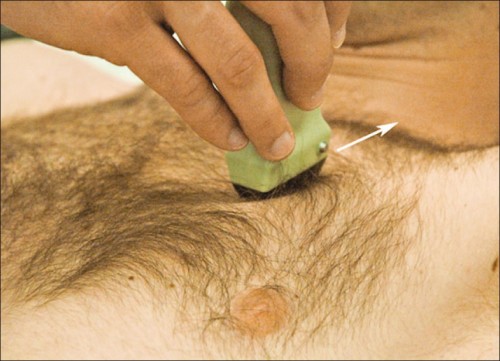
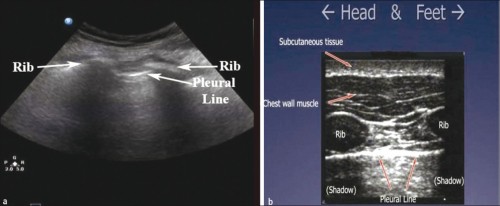
Pneumothorax: Echographie
Husain LF et All. Sonographic diagnosis of pneumothorax.
J Emerg Trauma Shock 2012;5:76-81
Position de la sonde
Images normales
Le glissement pleural Vidéo
La chauve-souris
Le bord de plage
Les lignes B
Images Anormales attestant du pneumothorax
Pas de glissement Vidéo
Le signe du Barcode
Les lignes A
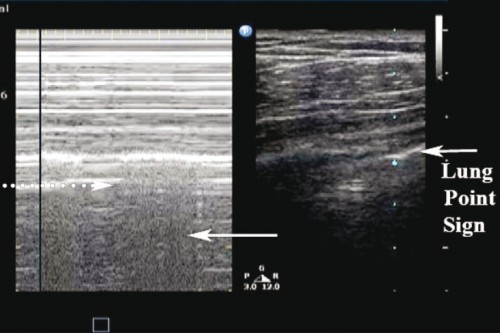
Le point poumon
Le pouls pulmonaire

Pour aller plus loin:
| Tags : pneumothorax, échographie
05/05/2013
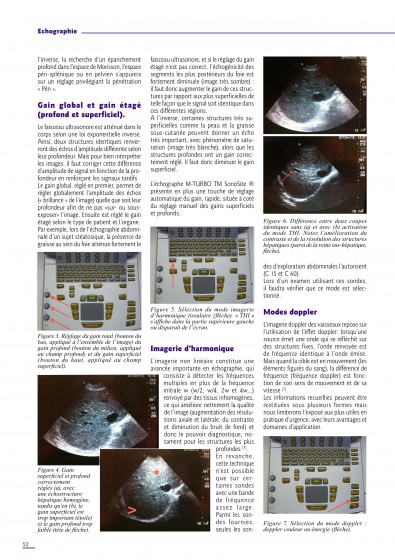
Echographe: Bien régler pour bien voir
| Tags : échographie
06/04/2013
Échographie abdomino-pelvienne d’urgence
Échographie abdominopelvienne d’urgence.
Principales indications
Petrovic T. et Al. Urgences 2010
L’échographie clinique s’est développée en médecine d’urgence depuis plusieurs années pour devenir incontournable. De nombreuses études ont montré son efficacité et son intérêt en médecine d’urgence tant extrahospitalière qu’intrahospitalière. Un transfert progressif de compétences s’est opéré entre les radiologues d’une part, les spécialistes ayant intégré les ultrasons dans leur pratique courante (cardiologues, gynéco-obstétriciens, etc.) d’autre part et les médecins urgentistes. De fait, la question principale d’aujourd’hui n’est plus « pourquoi faire ? », mais « comment faire ? ». Après avoir choisi le bon appareil et la bonne sonde, une des réponses à cette question consiste à choisir des indications et des incidences précises et focalisées répondant à des besoins cliniques et non pas seulement diagnostiques. Répondre, par exemple, aux questions posées par une douleur abdominale implique un raisonnement médical intégrant de nombreuses variables parmi lesquelles certaines peuvent être explorées par l’échographie d’urgence. Il n’est donc pas question, tout du moins dans un premier temps, de rechercher des lésions fines au chevet du malade, mais plutôt de repérer des anomalies directes ou indirectes s’intégrant dans un syndrome plus général.Du fait de la richesse potentielle des informations fournies par une échographieabdominale, une attitude pragmatique est donc la plus adaptée.
| Tags : échographie
06/04/2012
Echographie Pulmonaire
Glissement pleural
https://www.youtube.com/watch?v=HD7JzLg33nE
Pneumothorax
https://www.youtube.com/watch?v=7bK_C9NyrAc
Epanchement