12/12/2025
eFAST et thorax ouvert: Manque de sensibilité +++
Accuracy, reliability, and utility of the extended focused assessment with sonography in trauma examination in the setting of thoracic gunshot wounds
Miharu A et Al. Journal of Trauma and Acute Care Surgery 98(6):p 867-874, June 2025.
------------------------------------------
eFAST en cas de thorax ouvert ? Et bien pas si sûr
------------------------------------------
BACKGROUND
The extended focused assessment with sonography in trauma (eFAST) examination includes additional thoracic views beyond the standard focused assessment with sonography in trauma examination. Its validation has predominantly been conducted in blunt trauma cases. Our aim was to evaluate the eFAST examination in a targeted population with penetrating thoracic trauma.
METHODS
Patients with thoracic gunshot wounds who underwent eFAST between 2017 and 2021 were included from a local trauma registry. Performance metrics for each component of eFAST in each window and pathological condition were analyzed across the entire population, as well as within two cohorts: survived and deceased patients. Chest tube placement rates were compared within true-positive and false-negative (FN) eFAST results for subgroups with pneumothorax or hemothorax.
Miharu A et Al. Journal of Trauma and Acute Care Surgery 98(6):p 867-874, June 2025.
RESULTS
A total of 288 patients were included (male, 91% male; Injury Severity Score ≥15, 48%; and died, 17%). Thirty-nine percent required chest tube, and 18% required urgent thoracic surgical intervention. Although specificity was high (91–100%) for all components, the sensitivity was less than 50% for all thoracic views, except for “no cardiac motion” (100% sensitivity). Sensitivity for pericardial fluid was 47%; for pneumothorax, 22%; for hemothorax, 36%; and for peritoneal fluid, 51% in the total population. Comparing survived versus deceased cohort, the eFAST sensitivity was higher among deaths for all components. The majority of patients (>70%) with a FN eFAST for pneumothorax or hemothorax received chest tube.

CONCLUSION
The eFAST examination showed highly variable performance metrics among patients with penetrating thoracic trauma, with all thoracic components demonstrating high specificity but low overall sensitivity. Urgent interventions were frequently received in patients with FN studies.
14/11/2022
Echographie ciblée: Quelles recommandations ?
International Evidence-Based Recommendations for Focused Cardiac Ultrasound
Via G et Al. J Am Soc Echocardiogr. 2014 Jul;27(7):683.e1-683.e33.
BACKGROUNDS:
Focused cardiac ultrasound (FoCUS) is a simplified, clinician-performed application of echocardiography that is rapidly expanding in use, especially in emergency and critical care medicine. Performed by appropriately trained clinicians, typically not cardiologists, FoCUS ascertains the essential information needed in critical scenarios for time-sensitive clinical decision making. A need exists for quality evidence-based review and clinical recommendations on its use.
METHODS:
The World Interactive Network Focused on Critical UltraSound conducted an international, multispecialty, evidence-based, methodologically rigorous consensus process on FoCUS. Thirty-three experts from 16 countries were involved. A systematic multiple-database, double-track literature search (January 1980 to September 2013) was performed. The Grading of Recommendation, Assessment, Development and Evaluation method was used to determine the quality of available evidence and subsequent development of the recommendations. Evidence-based panel judgment and consensus was collected and analyzed by means of the RAND appropriateness method.
RESULTS:
During four conferences (in New Delhi, Milan, Boston, and Barcelona), 108 statements were elaborated and discussed. Face-to-face debates were held in two rounds using the modified Delphi technique. Disagreement occurred for 10 statements. Weak or conditional recommendations were made for two statements and strong or very strong recommendations for 96. These recommendations delineate the nature, applications, technique, potential benefits, clinical integration, education, and certification principles for FoCUS, both for adults and pediatric patients.
CONCLUSIONS:
This document presents the results of the first International Conference on FoCUS. For the first time, evidence-based clinical recommendations comprehensively address this branch of point-of-care ultrasound, providing a framework for FoCUS to standardize its application in different clinical settings around the world.
27/11/2020
Trauma du larynx: Faites une échographie !
Novel role of focused airway ultrasound in early airway assessment of suspected laryngeal trauma
Adi et al. Ultrasound J (2020) 12:37
Case presentation
We report a case series that illustrate the diagnostic value of focused airway ultrasound in the diagnosis of laryngeal trauma in patients presenting with blunt neck injury.
Conclusion
Early recognition, appropriate triaging, accurate airway evaluation, and prompt management of such injuries are essential. In this case series, we introduce the potential role of focused airway ultrasound in suspected laryngeal trauma, and the correlation of these exam findings with that of computed tomography (CT) scanning, based on the Schaefer classification of laryngeal injury.
02/02/2020
Echographie visuelle et etat de choc
30/11/2019
Echo: Intérêt pas évident pour tous ?
Does point of care ultrasonography improve clinical outcomes in emergency department patients with undifferentiated hypotension? An international randomized controlled trial from the SHoC-ED investigators.
STUDY OBJECTIVE:
Point-of-care ultrasonography protocols are commonly used in the initial management of patients with undifferentiated hypotension in the emergency department (ED). There is little published evidence for any mortality benefit. We compare the effect of a point-of-care ultrasonography protocol versus standard care without point-of-care ultrasonography for survival and clinical outcomes.
METHODS:
This international, multicenter, randomized controlled trial recruited from 6 centers in North America and South Africa and included selected hypotensive patients (systolic blood pressure <100 mm Hg or shock index >1) randomized to early point-of-care ultrasonography plus standard care versus standard care without point-of-care ultrasonography. Diagnoses were recorded at 0 and 60 minutes. The primary outcome measure was survival to 30 days or hospital discharge. Secondary outcome measures included initial treatment and investigations, admissions, and length of stay.
RESULTS:
Follow-up was completed for 270 of 273 patients. The most common diagnosis in more than half the patients was occult sepsis. We found no important differences between groups for the primary outcome of survival (point-of-care ultrasonography group 104 of 136 patients versus standard care 102 of 134 patients; difference 0.35%; 95% binomial confidence interval [CI] -10.2% to 11.0%), survival in North America (point-of-care ultrasonography group 76 of 89 patients versus standard care 72 of 88 patients; difference 3.6%; CI -8.1% to 15.3%), and survival in South Africa (point-of-care ultrasonography group 28 of 47 patients versus standard care 30 of 46 patients; difference 5.6%; CI -15.2% to 26.0%). There were no important differences in rates of computed tomography (CT) scanning, inotrope or intravenous fluid use, and ICU or total length of stay.
CONCLUSION:
To our knowledge, this is the first randomized controlled trial to compare point-of-care ultrasonography to standard care without point-of-care ultrasonography in undifferentiated hypotensive ED patients. We did not find any benefits for survival, length of stay, rates of CT scanning, inotrope use, or fluid administration. The addition of a point-of-care ultrasonography protocol to standard care may not translate into a survival benefit in this group.
27/11/2019
SOF Sono
05/10/2018
Conio: Echo, cela se confirme
Ultrasound Is Superior to Palpation in Identifying the Cricothyroid Membrane in Subjects with Poorly Defined Neck Landmarks: A Randomized Clinical Trial.
BACKGROUND: Success of a cricothyrotomy is dependent on accurate identification of the cricothyroid membrane. The objective of this study was to compare the accuracy of ultrasonography versus external palpation in localizing the cricothyroid membrane.
METHODS:
In total, 223 subjects with abnormal neck anatomy who were scheduled for neck computed-tomography scan at University Health Network hospitals in Toronto, Canada, were randomized into two groups: external palpation and ultrasound. The localization points of the cricothyroid membrane determined by ultrasonography or external palpation were compared to the reference midpoint (computed-tomography point) of the cricothyroid membrane by a radiologist who was blinded to group allocation. Primary outcome was the accuracy in identification of the cricothyroid membrane, which was measured by digital ruler in millimeters from the computed-tomography point to the ultrasound point or external-palpation point. Success was defined as the proportion of accurate attempts within a 5-mm distance from the computed-tomography point to the ultrasound point or external-palpation point.
RESULTS:
The percentage of accurate attempts was 10-fold greater in the ultrasound than external-palpation group (81% vs. 8%; 95% CI, 63.6 to 81.3%; P < 0.0001). The mean (SD) distance measured from the external-palpation to computed-tomography point was five-fold greater than the ultrasound to the computed-tomography point (16.6 ± 7.5 vs. 3.4 ± 3.3 mm; 95% CI, 11.67 to 14.70; P < 0.0001).
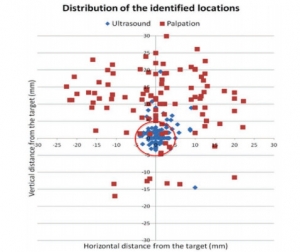
Analysis demonstrated that the risk ratio of inaccurate localization of the cricothyroid membrane was 9.14-fold greater with the external palpation than with the ultrasound (P < 0.0001). There were no adverse events observed.
CONCLUSIONS:
In subjects with poorly defined neck landmarks, ultrasonography is more accurate than external palpation in localizing the cricothyroid membrane.
| Tags : airway, coniotomie
30/09/2018
US: Mieux que la main pour la conio
A multicentre prospective cohort study of the accuracy of conventional landmark technique for cricoid localisation using ultrasound scanning
Cricoid pressure is employed during rapid sequence induction to reduce the risk of pulmonary aspiration. Correct application of cricoid pressure depends on knowledge of neck anatomy and precise identification of surface landmarks. Inaccurate localisation of the cricoid cartilage during rapid sequence induction risks incomplete oesophageal occlusion, with potential for pulmonary aspiration of gastric contents. It may also compromise the laryngeal view for the anaesthetist. Accurate localisation of the cricoid cartilage therefore has relevance for the safe conduct of rapid sequence induction.
We conducted a multicentre, prospective cohort study to determine the accuracy of cricoid cartilage identification in 100 patients. The cranio‐caudal midpoint of the cricoid cartilage was identified by a qualified anaesthetic assistant using the conventional landmark technique and marked. While maintaining the patient in the same position, a second mark was made by identifying the midpoint of the cricoid cartilage using ultrasound scanning.
The mean (SD) distance between the two marks was 2.07 (8.49) mm. In 41% of patients the midpoint was incorrectly identified by a margin greater than 5 mm. This error was uniformly distributed both above and below the midpoint of the cricoid cartilage. The Pearson correlation coefficient of this error with respect to body mass index was 0.062 (p = 0.539) and with age was −0.020 (p = 0.843). There were also no significant differences in error between male and female patients.
Identification of cricoid position using a landmark technique has a high degree of variability and has little correlation with age, sex or body mass index. These findings have significant implications for the safe application of cricoid pressure in the context of rapid sequence induction.
| Tags : airway, coniotomie
22/09/2018
Echo pour l'intubation
Integration of Point-of-care Ultrasound during Rapid Sequence Intubation in Trauma Resuscitation.
Introduction:
Airway and breathing management play critical role in trauma resuscitation. Early identification of esophageal intubation and detection of fatal events is critical. Authors studied the utility of integration of point-of-care ultrasound (POCUS) during different phases of rapid sequence intubation (RSI) in trauma resuscitation.
Methods:
It was prospective, randomized single-centered study conducted at the Emergency Department of a level one trauma center. Patients were divided into ultrasonography (USG) and clinical examination (CE) arm. The objectives were to study the utility of POCUS in endotracheal tube placement and confirmations and identification of potentially fatal conditions as tracheal injury, midline vessels, paratracheal hematoma, vocal cord pathology, pneumothorax, and others during RSI. Patient >1 year of age were included. Time taken for procedure, number of incorrect intubations, and pathologies detected were noted. The data were collected in Microsoft Excel spread sheets and analyzed using Stata (version 11.2, Stata Corp, Texas, U. S. A) software.
Results:
One hundred and six patients were recruited. The mean time for primary survey USG versus CE arm was (20 ± 10.01 vs. 18 ± 11.03) seconds. USG detected four pneumothorax, one tracheal injury, and one paratracheal hematoma. The mean procedure time USG versus CE arm was (37.3 ± 21.92 vs. 58 ± 32.04) seconds. Eight esophageal intubations were identified in USG arm by POCUS and two in CE arm by EtCO2 values.
Conclusion:
Integration of POCUS was useful in all three phases of RSI. It identified paratracheal hematoma, tracheal injury, and pneumothorax. It also identified esophageal intubation and confirmed main stem tracheal intubation in less time compared to five-point auscultation and capnography.
| Tags : airway
21/09/2018
Airway Ultrasound
| Tags : airway
01/02/2017
Echo: Pour le thorax surtout
Traumatic cardiac injury: Experience from a level-1 trauma centre
Mishra B. et Al. Chin J Traumatol. 2016 Dec 1;19(6):333-336.
--------------------------------------
Disposer d'un appareil d'échographie est d'un grand intérêt. Encore faut-il maîtriser cette technique (1) sous peine de se tromper dans les priorités de prise en charge. Le recours a cette technique reste débattu pour la prise en charge de traumatismes pénétrants. L'échographie thoracique est probablement à valeur ajoutée tant sur l'imagerie pleurale que péricardique. C'est ce que présente ce travail. Ce document rapporte également l'inefficacité en terme de survie de péricardocentèse pourtant prôné par l'ATLS.
--------------------------------------
Traumatic cardiac injury (TCI) is a challenge for trauma surgeons as it provides a short thera- peutic window and the management is often dictated by the underlying mechanism and hemodynamic status. The current study is to evaluate the factors influencing the outcome of TCI.
METHODS:
Prospectively maintained database of TCI cases admitted at a Level-1 trauma center from July 2008 to June 2013 was retrospectively analyzed. Hospital records were reviewed and statistical analysis was performed using the SPSS version 15.
RESULTS:
Out of 21 cases of TCI, 6 (28.6%) had isolated and 15 (71.4%) had associated injuries. Ratio be- tween blunt and penetrating injuries was 2:1 with male preponderance. Mean ISS was 31.95. Thirteen patients (62%) presented with features suggestive of shock. Cardiac tamponade was present in 12 (57%) cases and pericardiocentesis was done in only 6 cases of them. Overall 19 patients underwent surgery. Perioperatively 8 (38.1%) patients developed cardiac arrest and 7 developed cardiac arrhythmia. Overall survival rate was 71.4%. Mortality was related to cardiac arrest (p = 0.014), arrhythmia (p = 0.014), and hemorrhagic shock (p =0.04). The diagnostic accuracy of focused assessment by sonography in trauma (FAST) was 95.24%.
CONCLUSION:
High index of clinical suspicion based on the mechanism of injury, meticulous examination by FAST and early intervention could improve the overall outcome.
02/12/2016
Echo préhospitalière: Expertise à construire svp!
Prehospital ultrasound of the abdomen and thorax changes trauma patient management: A systematic review
O’Dochartaigh D et Al. Injury, Int. J. Care Injured 46 (2015) 2093–2102
--------------------------------------------------
L'échographie tend à prendre une place de plus en plus importante dans notre quotidien. L'existence d'appareils portables, à l'ergonomie et la performance sans cesse améliorée, procède à la généralisation de cet outil d'évaluation dont on comprend bien l'intérêt. Pour autant qu'apporte réellement ce moyen d'exploration et tout particulièrement en préhospitalier ? Et bien les choses ne sont pas si évidentes que cela. Sauf à être mis en oeuvre par des mains expertes et pour des pathologies ciblées et malgré l'engouement général l'intérêt réel reste à prouver. Ce travail n'est pas isolé (1, 2) et devrait nous pousser à une certaine pondération et surtout à des efforts de formation des praticiens ayant recours à cette technique (3).
--------------------------------------------------
Background: Ultrasound examination of trauma patients is increasingly performed in prehospital services. It is unclear if prehospital sonographic assessments change patient management: providing prehospital diagnosis and treatment, determining choice of destination hospital, or treatment at the receiving hospital.
Objective: This review aims to assess and grade the evidence that specifically examines whether prehospital ultrasound (PHUS) of the thorax and/or abdomen changes management of the trauma patient.
Methods: A systematic review was conducted of trauma patients who had an ultrasound of the thorax or abdomen performed in the prehospital setting. PubMed, MEDLINE, Web of Science (CINAHL, EMBASE, Cochrane Central Register of Controlled Trials) and the reference lists of included studies were searched. Methodological quality was checked and risk of bias analysis performed, a level of evidence grade was assigned, and descriptive data analysis performed.
Results: 992 unique citations were identified, which included eight studies that met inclusion criteria with a total of 925 patients. There are no reports of randomised controlled trials. Heterogeneity exists between the included studies which ranged from a case series to retrospective and prospective nonrandomised observational studies. Three studies achieved a 2+ Scottish Intercollegiate Guidelines Networks grade for quality of evidence and the remainder demonstrated a high risk of bias. The three best studies each provided examples of prehospital ultrasound positively changing patient management.
Conclusion: There is moderate evidence that supports prehospital physician use of ultrasound for trauma patients. For some patients, management was changed based on the results of the PHUS. The benefit of ultrasound use in non-physician services is unclear.
31/08/2016
Echo et voies aériennes: Mais oui, à maîtriser
The Role of Airway and Endobronchial Ultrasound in Perioperative Medicine
Vortrua J et Al. Biomed Res Int. 2015; 2015: 754626
-------------------------------
Certainement UN APPORT IMPORTANT à la gestion des voies aériennes et de la ventilation non seulement dans les blocs opératoires mais dans les situations critiques y compris hors de l'hôpital.
-------------------------------
Recent years have witnessed an increased use of ultrasound in evaluation of the airway and the lower parts of the respiratory system. Ultrasound examination is fast and reliable and can be performed at the bedside and does not carry the risk of exposure to ionizing radiation. Apart from use in diagnostics it may also provide safe guidance for invasive and semi-invasive procedures. Ultrasound examination of the oral cavity structures, epiglottis, vocal cords, and subglottic space may help in the prediction of difficult intubation. Preoperative ultrasound may diagnose vocal cord palsy or deviation or stenosis of the trachea. Ultrasonography can also be used for confirmation of endotracheal tube, double-lumen tube, or laryngeal mask placement. This can be achieved by direct examination of the tube inside the trachea or by indirect methods evaluating lung movements. Postoperative airway ultrasound may reveal laryngeal pathology or subglottic oedema. Conventional ultrasound is a reliable real-time navigational tool for emergency cricothyrotomy or percutaneous dilational tracheostomy. Endobronchial ultrasound is a combination of bronchoscopy and ultrasonography and is used for preoperative examination of lung cancer and solitary pulmonary nodules. The method is also useful for real-time navigated biopsies of such pathological structures.
| Tags : airway
30/08/2016
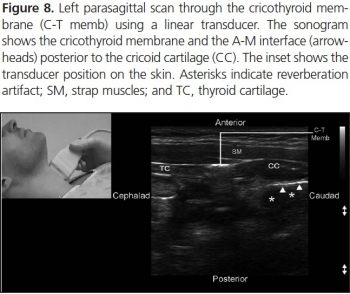
Crico et Echo: Pensez TACA
Ultrasonographic identification of the cricothyroid membrane: best evidence, techniques, and clinical impact
Kristensen MS et Al. Br. J. Anaesth. (2016) 117 (suppl 1):i39-i48
Inability to identify the cricothyroid membrane by inspection and palpation contributes substantially to the high failure rate of cricothyrotomy. This narrative review summarizes the current evidence for application of airway ultrasonography for identification of the cricothyroid membrane compared with the clinical techniques. We identified the best-documented techniques for bedside use, their success rates, and the necessary training for airway-ultrasound-naïve clinicians.

After a short but structured training, the cricothyroid membrane can be identified using ultrasound in difficult patients by previously airway-ultrasound naïve anaesthetists with double the success rate of palpation. Based on the literature, we recommend identifying the cricothyroid membrane before induction of anaesthesia in all patients. Although inspection and palpation may suffice in most patients, the remaining patients will need ultrasonographic identification; a service that we should aim at making available in all locations where anaesthesia is undertaken and where patients with difficult airways could be encountered.
| Tags : airway
05/08/2016
Echo pour abord vasculaire: Intérêt modéré ?
Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization
Cochrane Database Syst Rev. 2015 Jan 9;1:CD011447. doi: 10.1002/14651858.CD011447.
-------------------------------------
La mise en place d'un abord veineux central est une éventualité peu fréquente en médecine tactique. La maîtrise de l'abord vasculaire périphérique et l'apport de la perfusion intraosseuse suffisent le plus souvent à répondre aux besoins. Néanmoins ce besoin ne peut être écarté. Alors que la majorité des sociétés savantes recommandent le recours à la pose échoguidée, il semblerait qu'une analyse critique de l'intérêt d'une telle pratique ne soit pas encore complètement en faveur de telles recommandations (???). Même si de très grandes avancées technologiques ont lieu et permettent de disposer d'appareil et de sondes adhoc utilisables hors de l'hôpital, dans nos conditions d'exercice et donc in fine de notre aptitude à cette pratique sans échographe.
-------------------------------------
BACKGROUND:
Central venous catheters can help with diagnosis and treatment of the critically ill. The catheter may be placed in a large vein in the neck (internal jugular vein), upper chest (subclavian vein) or groin (femoral vein). Whilst this is beneficial overall, inserting the catheter risks arterial puncture and other complications and should be performed in as few attempts as possible.In the past, anatomical 'landmarks' on the body surface were used to find the correct place to insert these catheters, but ultrasound imaging is now available. A Doppler mode is sometimes used to supplement plain 'two-dimensional' ultrasound.
OBJECTIVES:
The primary objective of this review was to evaluate the effectiveness and safety of two-dimensional ultrasound (US)- or Dopplerultrasound (USD)-guided puncture techniques for subclavian vein, axillary vein and femoral vein puncture during central venous catheter insertion in adults and children. We assessed whether there was a difference in complication rates between traditional landmark-guided and any ultrasound-guided central vein puncture.When possible, we also assessed the following secondary objectives: whether a possible difference could be verified with use of the US technique versus the USD technique; whether there was a difference between using ultrasound throughout the puncture ('direct') and using it only to identify and mark the vein before starting the puncture procedure ('indirect'); and whether these possible differences might be evident in different groups of patients or with different levels of experience among those inserting the catheters.
SEARCH METHODS:
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 1), MEDLINE (1966 to 15 January 2013), EMBASE (1966 to 15 January 2013), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1982 to 15 January 2013), reference lists of articles, 'grey literature' and dissertations. An additional handsearch focused on intensive care and anaesthesia journals and abstracts and proceedings of scientific meetings. We attempted to identify unpublished or ongoing studies by contacting companies and experts in the field, and we searched trial registers. We reran the search in August 2014. We will deal with any studies of interest when we update the review.
SELECTION CRITERIA:
Randomized and quasi-randomized controlled trials comparing two-dimensional ultrasound or Doppler ultrasound versusan anatomical 'landmark' technique during insertion of subclavian or femoral venous catheters in both adults and children.
DATA COLLECTION AND ANALYSIS:
Three review authors independently extracted data on methodological quality, participants, interventions and outcomes of interest using a standardized form. We performed a priori subgroup analyses.
MAIN RESULTS:
Altogether 13 studies enrolling 2341 participants (and involving 2360 procedures) fulfilled the inclusion criteria. The quality of evidence was very low (subclavian vein N = 3) or low (subclavian vein N = 4, femoral vein N = 2) for most outcomes, moderate for one outcome (femoral vein) and high at best for two outcomes (subclavian vein N = 1, femoral vein N = 1). Most of the trials had unclear risk of bias across the six domains, and heterogeneity among the studies was significant. For the subclavian vein (nine studies, 2030 participants, 2049 procedures), two-dimensional ultrasound reduced the risk of inadvertent arterial puncture (three trials, 498 participants, risk ratio (RR) 0.21, 95% confidence interval (CI) 0.06 to 0.82; P value 0.02, I² = 0%) and haematoma formation (three trials, 498 participants, RR 0.26, 95% CI 0.09 to 0.76; P value 0.01, I² = 0%). No evidence was found of a difference in total or other complications (together, US, USD), overall (together, US, USD), number of attempts until success (US) or first-time (US) success rates or time taken to insert the catheter (US). For the femoral vein, fewer data were available for analysis (four studies, 311 participants, 311 procedures). No evidence was found of a difference in inadvertent arterial puncture or other complications. However, success on the first attempt was more likely with ultrasound (three trials, 224 participants, RR 1.73, 95% CI 1.34 to 2.22; P value < 0.0001, I² = 31%), and a small increase in the overall success rate was noted (RR 1.11, 95% CI 1.00 to 1.23; P value 0.06, I² = 50%). No data on mortality or participant-reported outcomes were provided.
AUTHORS' CONCLUSIONS:
On the basis of available data, we conclude that two-dimensional ultrasound offers small gains in safety and quality when compared with an anatomical landmark technique for subclavian (arterial puncture, haematoma formation) or femoral vein (success on the first attempt) cannulation for central vein catheterization. Data on insertion by inexperienced or experienced users, or on patients at high risk for complications, are lacking. The results for Doppler ultrasound techniques versus anatomical landmark techniques are uncertain.
03/08/2016
Echographie clinique en médecine d'urgence
Premier niveau de compétence pour l'échographie clinique en médecine d’urgence
Recommandations de la Société française de médecine d’urgence par consensus formalisé.
Société française de médecine d’urgence 2016
clic sur l'image pour accéder au document
| Tags : échographie
05/06/2016
Echographie pour l'intubation: Plutôt oui.
Tracheal ultrasonography and ultrasonographic lung sliding for confirming endotracheal tube placement: Speed and Reliability
BACKGROUND:
In this study we aimed to evaluate the success of ultrasonography (USG) for confirming the tube placement and timeliness by tracheal USG and ultrasonographic lung sliding in resuscitation and rapid sequence intubation.
MATERIALS AND METHODS:
This study was a prospective, single-center, observational study conducted in the emergency department of a tertiary care hospital. Patients were prospectively enrolled in the study. Patients who went under emergency intubation because of respiratory failure, cardiac arrest or severe trauma included in the study. Patients with severe neck trauma, neck tumors, history of neck operation or tracheotomy and under 18years old were excluded from the study.
RESULTS:
A total of 115 patients included in the study. The mean age was 67.2±17.1 with age 16-95years old. Among 115 patients 30 were cardiac arrest patients other 85 patients were non-cardiac arrest patients intubated with rapid sequence intubation. The overall accuracy of the ultrasonography was 97.18% (95% CI, 90.19-99.66%), and the value of kappa was 0.869 (95% CI, 0.77-0.96), indicating a high degree of agreement between the ultrasonography and capnography. The ulrasonography took significantly less time than capnography in total.
DISCUSSION:
Ultrasonography achieved high sensitivity and specificity for confirming tube placement and results faster than end-tidal carbon dioxide. Ultrasonography is a good alternative for confirming the endotracheal tube placement. Future studies should examine the use of ultrasonography as a method for real-time assessment of endotracheal tube placement by emergency physicians with only basic ultrasonographic training.
| Tags : airway, échographie
30/10/2015
Echographie: De l'expérience SVP
Does physician experience influence the interpretability of focused echocardiography images performed by a pocket device?
Bobbia X et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2015) 23:52
---------------------------------------------------------------
Il existe un très grand engouement concernant l'emploi d'échographe dit de poche. Cet article appelle a être plus circonspect. Sil il s'agit bien de faire rentrer l'échographie dans la pratique quotidienne, encore faut il que cela soit assorti d'une qualification réelle.
---------------------------------------------------------------
Introduction: The use of focused cardiac ultrasound (FoCUS) in a prehospital setting is recommended. Pocket ultrasound devices (PUDs) appear to be well suited to prehospital FoCUS. The main aim of our study was to evaluate the interpretability of echocardiography performed in a prehospital setting using a PUD based on the experience of the emergency physician (EP).
Methods: This was a monocentric prospective observational study. We defined experienced emergency physicians (EEPs) and novice emergency physicians (NEPs) as echocardiographers if they had performed 50 echocardiographies since their initial university training (theoretical training and at least 25 echocardiographies performed with a mentor). Each patient undergoing prehospital echocardiography with a PUD was included. Four diagnostic items based on FoCUS were analyzed: pericardial effusions (PE), right ventricular dilation (RVD), qualitative left ventricular function assessment (LVEF), and inferior vena cava compliance (IVCC). Two independent experts blindly evaluated the interpretability of each item by examining recorded video loops. If their opinions were divided, then a third expert concluded.
Results: Fourteen EPs participated: eight (57 %) EEPs and six (43 %) NEPs. Eighty-five patients were included: 34 (40 %) had an echocardiography by an NEP and 51 (60 %) by an EEP. The mean number of interpretable items by echocardiography was three [1; 4]; one [0; 2.25] in the NEP group, four [3; 4] in EEP (p < .01). The patient position was also associated with interpretable items: supine three [2; 4], “45°” three [1; 4], sitting two [1; 4] (p = .02). In multivariate analysis, only EP experience was associated with the number of interpretable items (p = .02). Interpretability by NEPs and EEPs was: 56 % vs. 96 % for LVF, 29 % vs. 98 % for PE, 26 % vs. 92 % for RVD, and 21 % vs. 67 % for IVCC (p < .01 for all).
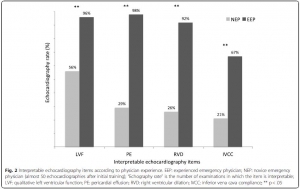
Conclusion: FoCUS with PUD in prehospital conditions was possible for EEPs, It is difficult and the diagnostic yield is poor for NEPs.
| Tags : échographie
25/07/2015
Echo des voies aériennes
Focused ultrasound for airway management
http://viewer.zmags.com/publication/698570e2#/698570e2/1Tutoriel Philips
SANS HĖSITER: IL FAUT S'Y METTRE +++
Clic sur l'image pour accéder au document
Deux exemples
1. Visualisation de l'épiglotte:
- Vue transverse

- Vue parasagittale

2. Repérage du cartilage cricoïdienne en coupe sagittale ou parasagittale

3. Réalisation d'une coniotomie
| Tags : airway, échographie
20/07/2015
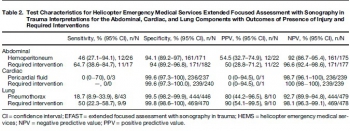
Echo en hélico: Avec formation solide !
Prospective evaluation of prehospital trauma ultrasound during aeromedical transport.
Press GM et Al. J Emerg Med. 2014 Dec;47(6):638-45
------------------------------------------------
L'apport de l'échographie est incontournable pour la prise en charge des traumatisés. Son emploi en prehospitalier est proposé. Pour autant la mise en oeuvre de ce moyen d'exploration n'est pas si simple et demande une grande expertise. Le travail présenté porte sur la mise en oeuvre de ce type d'exploration par technicinens paramédicaux expérimentés et ayant suivi une formation sur une période de deux mois. malgré cela leur performance reste modeste. Un examen négatif de permet pas de conclure. Ceci plaide pour un peu de modération concernant l'engouement actuel. Comme pour tout il faut investir sur la formation pour être performant.
------------------------------------------------
BACKGROUND:
Ultrasound is widely considered the initial diagnostic imaging modality for trauma. Preliminary studies have explored the use of trauma ultrasound in the prehospital setting, but the accuracy and potential utility is not well understood.
OBJECTIVE:
We sought to determine the accuracy of trauma ultrasound performed by helicopter emergency medical service (HEMS) providers.
METHODS:
Trauma ultrasound was performed in flight on adult patients during a 7-month period. Accuracy of the abdominal, cardiac, and lung components was determined by comparison to the presence of injury, primarily determined by computed tomography, and to required interventions.
RESULTS:
HEMS providers performed ultrasound on 293 patients during a 7-month period, completing 211 full extended Focused Assessment with Sonography for Trauma (EFAST) studies. HEMS providers interpreted 11% of studies as indeterminate. Sensitivity and specificity for hemoperitoneum was 46% (95% confidence interval [CI] 27.1%-94.1%) and 94.1% (95% CI 89.2%-97%), and for laparotomy 64.7% (95% CI 38.6%-84.7%) and 94% (95% CI 89.2%-96.8%), respectively. Sensitivity and specificity for pneumothorax were 18.7% (95% CI 8.9%-33.9%) and 99.5% (95% CI 98.2%-99.9%), and for thoracostomy were 50% (95% CI 22.3%-58.7%) and 99.8% (98.6%-100%), respectively. The positive likelihood ratio for laparotomy was 10.7 (95% CI 5.5-21) and for thoracostomy 235 (95% CI 31-1758), and the negative likelihood ratios were 0.4 (95% CI 0.2-0.7) and 0.5 (95% CI 0.3-0.8), respectively. Of 240 cardiac studies, there was one false-positive and three false-negative interpretations (none requiring intervention).
CONCLUSIONS:
HEMS providers performed EFAST with moderate accuracy. Specificity was high and positive interpretations raised the probability of injury requiring intervention. Negative interpretations were predictive, but sensitivity was not sufficient for ruling out injury.
| Tags : échographie