08/05/2016
la voie axillaire +++
Chest wall thickness and decompression failure: A systematic review and meta-analysis comparing anatomic locations in needle thoracostomy
Laan DV et Al. Injury, Int. J. Care Injured 47 (2016) 797–804
------------------------------------------
Une publication, une de plus, qui met en avant l'abord axillaire pour la décompression thoracique et qui insiste sur le peu de preuve de l'inocuité des cathéters de 8 cm. On rappelle que la thoracostomie au doigt reste la référence.
------------------------------------------
Introduction:
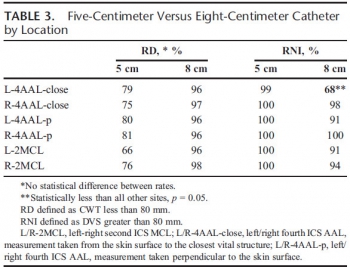
Current Advanced Trauma Life Support guidelines recommend decompression for thoracic tension physiology using a 5-cm angiocatheter at the second intercostal space (ICS) on the midclavicular line (MCL). High failure rates occur. Through systematic review and meta-analysis, we aimed to determine the chest wall thickness (CWT) of the 2nd ICS-MCL, the 4th/5th ICS at the anterior axillary line (AAL), the 4th/5th ICS mid axillary line (MAL) and needle thoracostomy failure rates using the currently recommended 5-cm angiocatheter.
Methods:
A comprehensive search of several databases from their inception to July 24, 2014 was conducted. The search was limited to the English language, and all study populations were included. Studies were appraised by two independent reviewers according to a priori defined PRISMA inclusion and exclusion criteria. Continuous outcomes (CWT) were evaluated using weighted mean difference and binary outcomes (failure with 5-cm needle) were assessed using incidence rate. Outcomes were pooled using the random-effects model.
Results:
The search resulted in 34,652 studies of which 15 were included for CWT analysis, 13 for NT effectiveness. Mean CWT was 42.79 mm (95% CI, 38.78–46.81) at 2nd ICS-MCL, 39.85 mm (95% CI, 28.70–51.00) at MAL, and 34.33 mm (95% CI, 28.20–40.47) at AAL (P = .08). Mean failure rate was 38% (95% CI, 24–54) at 2nd ICS-MCL, 31% (95% CI, 10–64) at MAL, and 13% (95% CI, 8–22) at AAL (P = .01).
Conclusion:
Evidence from observational studies suggests that the 4th/5th ICS-AAL has the lowest predicted failure rate of needle decompression in multiple populations.
| Tags : pneumothorax, exsufflation
25/02/2016
Exsufflation: Cela se complique !
Complications of needle thoracostomy: A comprehensive clinical review
Wernjck B et Al. Int J Crit Illn Inj Sci. 2015 Jul-Sep; 5(3): 160–169
---------------------------------------------
Comme toujours, après une phase d'engouement vient le temps de la réflexion. L'exsufflation à l'aiguille n'est pas d'une indication si fréquente et en plus expose à certaines complications. A lire avant de se lancer dans l'utilisation d'aiguille de tout genre.
---------------------------------------------
Needle thoracostomy (NT) is a valuable adjunct in the management of tension pneumothorax (tPTX), a life-threatening condition encountered mainly in trauma and critical care environments. Most commonly, needle thoracostomies are used in the prehospital setting and during acute trauma resuscitation to temporize the affected individuals prior to the placement of definitive tube thoracostomy (TT). Because it is both an invasive and emergent maneuver, NT can be associated with a number of potential complications, some of which may be life-threatening. Due to relatively common use of this procedure, it is important that healthcare providers are familiar, and ready to deal with, potential complications of NT.
| Tags : pneumothorax
12/08/2015
Drainer un thorax sans drain
Improvised Chest Tube Drain for Decompression of an Acute Tension Pneumothorax
Vinson ED Mil Med. 2004 May;169(5):403-5.
---------------------------------------
Décomprimer un thorax est indispensable en cas de pneumothorax suffocant. Si la décompression à l'aiguille est souvent présentée comme la technique de référence, encore faut il que sa réalisation soit faite par voie latérale avec un cathéter de calibre et longueur suffisant. Néanmoins cette technique est sujette à échec. La thoracostomie au doigt est la méthode la plus efficiente et la moins dangereuse. La justification de la pose d'un drain thoracique est moins claire: durée de transport conséquent, reconstitution du pneumothorax. Encore faut il avoir un drain.Si le cathéter du minitrach percut 2 peut être utilisé, c'est aussi le cas d'une ligne et d'une poche de perfusion qui semblent être une alternative à ne pas méconnaitre.
---------------------------------------
A case of a woman presenting with an acute tension pneumothorax during a Navy humanitarian mission in East Timor is presented. The patient was treated at a local rural clinic run by our medical team. Prompt insertion of a chest tube saved the woman’s life; however, there were no chest tube drains available. A field chest tube drain constructed out of an IV bag, a sterile water bottle, and tubing provided an adequate underwater seal and drain. Because of the remote location and limited resources, standard prehospital chest tube management had to be modified. A brief review of simple and tension pneumothoraces and management along with a description of the field chest tube drain is presented
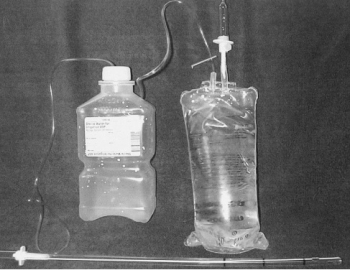
"The equipment needed includes a 24-French chest tube, a 100-mL NS IV bag, a 1,000-mL plastic sterile saline bottle, and two standard primary IV tube sets. The sterile water bottle is prepared by first emptying the contents. Next, two holes should be cut large enough to fit the surgical tubing, one in the cap, and one in the top of the bottle. The IV bag and primary IV tubing should be attached and the tube should be cut between the filter and reservoir. This end is left open for a vent. The other outlet port should be cut open to allow one end of a surgical tube to be inserted. The chest tube is then attached to the plastic spike of the other IV tubing. The other end of the tube is placed into the sterile water bottle through the hole in the cap. The surgical tube from the IV bag outlet port should be attached to the sterile water bottle through the hole in the side. The surgical tubing from the sterile water bag needs to be long enough to reach the top of the IV bag. To operate the system, the IV bag should be inverted to keep the underwater seal to the sterile water bottle. This allows the long tube to stay underwater while the short tube vents air out of the bag. To dispose of any accumulated fluid, the chest tube is first clamped near the patient. The water bottle can then be removed and emptied while the cap remains attached to the chest tube. It is then a simple matter to reattach the bottle and unclamp the chest tube"
| Tags : drainage thorax
06/08/2015
Thoracostomie: ni en antérieur ou postérieur mais par voie latérale
Evaluation of the Risk of Intercostal Artery Laceration During Thoracentesis in Elderly Patients by Using 3D-CT Angiography
Yoneyama H. et Al Inter Med 49: 289-292, 2010
--------------------------------------------
Les artères intercostales ne cheminent pas toujours au rebord inférieur de de la côte supérieure. Il existe de plus des rameaux latéraux plutôt postérieurs. Donc il faut aborder le thorax par voie latérale. Une approche latérale au niveau des 4/5èmes espaces intercostaux sur la lgne axillaire moyennne est sécuritaire.
--------------------------------------------
Objective
Our study was undertaken to determine the location of the tortuous intercostal artery in elderly patients by using 3D-CT angiography in order to prevent laceration during thoracentesis.
Methods
We evaluated the data of 3D-CT angiography of the intercostal artery in consecutive patients who had undergone contrast chest CT scan in our hospital from December 2007 to April 2008. We considered the “percent safe space” (the shortest lower rib-to-intercostal artery distance/the upper rib-to-lower rib distance) to be an index of safety that can be used to prevent laceration of the intercostal artery during thoracentesis. We measured this index at 3 points: the total site (5-10 cm lateral to the spine), the lateral site (9-10 cm lateral to the spine), and the medial site (5-6 cm lateral to the spine).
Results
We evaluated 33 cases (25 males and 8 females; mean age, 74.2 years). The mean percent safe space at the total site was 58.6%. The percent safe space at the total site tended to decrease with advancing age, but the correlation was low (p=0.0378, r=-0.3631). The percent safe space at the lateral site (mean, 79.8%) was significantly higher than that at the medial site (61.2%, p<0.0001).
Conclusion
We showed that the intercostal artery is tortuous and does not always lie along the inferior edge of the rib and that the percent safe space at the lateral site is significantly higher than that at the medial site in elderly patients
| Tags : exsufflation
05/08/2015
Décompression à l'aiguille: Pas fiable
Does needle thoracostomy provide adequate and effective decompression of tension pneumothorax?
Martin M et Al. J Trauma Acute Care Surg. 2012;73: 1412-1417
-----------------------
La décompression thoracique est une des mesures qui vise à réduire le nombre de morts évitables. Il s'agit d'une procédure mise en oeuvre peu fréquemment. L'exsufflation à l'aiguille est la méthode enseignée. Il existe beaucoup de débats concernant le lieu de ponction (plutôt par voie axillaire et non par voie antérieure), la longueur du cathéter (certains proposent 8 cm au risque de ponction parenchymateuse et des gros vaisseaux), le diamètre. Le travail proposé est très intéressant car il exprime toute les réserves qui doivent encadrer ce geste qui ne semble pas aussi efficace que cela car outre les problèmes mécanique il apparaît bien qu'un cathéter de 14G risque d'être insuffisant. On rappelle quand même que la thoracostomie au doigt est toujours possible et que votre doigt a de fortes chances de mesurer 8 cm donc de pouvoir pénétrer dans un thorax après création d'un stomie intercostale à la pince de monro-kelly.
-----------------------
BACKGROUND:
Tension pneumothorax (tPTX) is a common and potentially fatal event after thoracic trauma. Needle decompression is the currently accepted first-line intervention but has not been well validated. The purpose of this study was to evaluate the effectiveness of a properly placed and patent needle thoracostomy (NT) compared with standard tube thoracostomy (TT) in a swine model of tPTX.
METHODS:
Six adult swine underwent instrumentation and creation of tPTX using thoracic CO2 insufflation via a balloon trocar. A continued 1 L/min insufflation was maintained to simulate an ongoing air leak. The efficacy and failure rate of NT (14 gauge) compared with TT (34F) was assessed in two separate arms: (1) tPTX with hemodynamic compromise and (2) tPTX until pulseless electrical activity (PEA) obtained. Hemodynamics was assessed at 1 and 5 minutes after each intervention.
RESULTS:
A reliable and highly reproducible tPTX was created in all animals with a mean insufflation volume of 2441 mL. tPTX resulted in the systolic blood pressure declining 54% from baseline (128Y58 mm Hg), cardiac output declining by 77% (7Y1.6 L/min), and equalization of central venous pressure and wedge pressures. In the first arm, there were 19 tPTX events treated with NT placement. All NTs were patent on initial placement, but 5 (26%) demonstrated mechanical failure (due to kinking, obstruction, or dislodgment) within 5 minutes of placement, all associated with hemodynamic decline. Among the 14 NTs that remained patent at 5 minutes, 6 (43%) failed to relieve tension physiology for an overall failure rate of 58%. Decompression with TTwas successful in relieving tPTX in 100%. In the second arm, there were 21 tPTX with PEA events treated initially with either NT (n = 14) or TT (n = 7). The NT failed to restore perfusion in nine events (64%), whereas TT was successful in 100% of events as a primary intervention and restored perfusion as a rescue intervention in eight of the nine NT failures (88%).
CONCLUSION: Thoracic insufflation produced a reliable and easily controlled model of tPTX. NT was associated with high failure rates for relief of tension physiology and for treatment of tPTX-induced PEA and was due to both mechanical failure and inadequate tPTX evacuation. This performance data should be considered in future NT guideline development and equipment design
| Tags : exsufflation, pneumothorax
04/08/2015
Exsufflation: Ø plutôt que longueur
Needle thoracostomy for tension pneumothorax: the Israeli Defense Forces experience
Chen J et Al. Can J Surg 2015;58(3):S118-S124
-----------------------------
Il existe un grand débat sur la nature du cathéter à utiliser pour décomprimer un thorx sous pression. Ce travail est intéressant car, alors qu'il existe une forte pression pour recourir à des cathéters de 8cm, il rapporte une expérience de terrain conséquente où le recours à un angiocath n'a pas été lié à un taux d'échec rédhibitoire puisque 8 fois sur 1 une amélioration clinique est notée. Pour ces auteurs le débat porte plus sur le diamètre du cathéter que sa longueur. Ce document insiste également sur la disparition unilatérale du murmure vésiculaire comme repère du côté à ponctionner.
-----------------------------
Contexte :
La thoracotomie à l’aiguille (TA) pour le pneumothorax sous tension sur les lieux mêmes du traumatisme peut sauver des vies. Des données récentes ont mis en doute l’efficacité des dispositifs de TA classiques. C’est pourquoi le corps médical de l’armée israélienne (CMAI) a récemment proposé un cathéter plus long, plus large et plus résistant pour décomprimer rapidement le pneumothorax. Le présent article résume l’expérience du CMAI en matière de décompression des pneumothorax au moyen de la TA.
Méthodes :
Nous avons passé en revue le registre des traumatismes de l’armée israé- lienne entre janvier 1997 et octobre 2012 pour relever tous les cas où une TA a été tentée.
Résultats :
Durant la période de l’étude 111 patients en tout ont subi une décompression à l’aide d’une TA. La plupart des cas (54 %) résultaient de blessures par balles; les accidents de la route venaient au second rang (16 %). La plupart (79 %) des TA ont été effectuées sur les lieux, tandis que les autres ont été effectuées durant l’évacuation par ambulance ou par hélicoptère (13 % et 4 %, respectivement). L’atténuation des bruits respiratoires du côté affecté était l’une des indications cliniques les plus fréquentes de la TA, enregistrée dans 28 % des cas. L’atténuation des bruits respiratoires était plus fréquente chez les patients qui ont survécu (37 % c. 19 %, p < 0,001). Un drain thoracique a été installé sur le terrain chez 35 patients (32 %), à chaque fois après une TA.
Conclusion :
La TA standard s’accompagne d’un taux d’échec élevé sur le champ de bataille. Une autre mesure de décompression, comme le cathéter Vygon, semble être une solution de rechange envisageable à la TA classique.
| Tags : exsufflation
30/07/2015
Exsuffler: Aiguille de 6,44cm ?
Sufficient catheter length for pneumothorax needle decompression: a meta-analysis
Clemency BM et Al. Prehosp Disaster Med. 2015 Jun;30(3):249-53
Abstract
Introduction Needle thoracostomy is the prehospital treatment for tension pneumothorax. Sufficient catheter length is necessary for procedural success. The authors of this study determined minimum catheter length needed for procedural success on a percentile basis.
METHODS:
A meta-analysis of existing studies was conducted. A Medline search was performed using the search terms: needle decompression, needle thoracentesis, chest decompression, pneumothorax decompression, needle thoracostomy, and tension pneumothorax. Studies were included if they published a sample size, mean chest wall thickness, and a standard deviation or confidence interval. A PubMed search was performed in a similar fashion. Sample size, mean chest wall thickness, and standard deviation were found or calculated for each study. Data were combined to create a pooled dataset. Normal distribution of data was assumed. Procedural success was defined as catheter length being equal to or greater than the chest wall thickness.
RESULTS:
The Medline and PubMed searches yielded 773 unique studies; all study abstracts were reviewed for possible inclusion. Eighteen papers were identified for full manuscript review. Thirteen studies met all inclusion criteria and were included in the analysis. Pooled sample statistics were: n=2,558; mean=4.19 cm; and SD=1.37 cm. Minimum catheter length needed for success at the 95th percentile for chest wall size was found to be 6.44 cm. Discussion A catheter of at least 6.44 cm in length would be required to ensure that 95% of the patients in this pooled sample would have penetration of the pleural space at the site of needle decompression, and therefore, a successful procedure. These findings represent Level III evidence.
| Tags : exsufflation
09/06/2015
Faut il drainer avant de décoller: Non ?
Air Transport of Patients with Pneumothorax: Is Tube Thoracostomy Required Before Flight ?
Braude D et Al. Air Med J. 2014 Jul-Aug;33(4):152-6
Objective: It is conventionally thought that patients with pneumothorax (PTX) require tube thoracostomy (TT) before air medical transport (AMT), especially in unpressurized rotor-wing (RW) aircraft, to prevent deterioration from expansion of the PTX or development of tension PTX. We hypothesize that patients with PTX transported without TT tolerate RW AMT without serious deterioration, as defined by hypotension, hypoxemia, respiratory distress, intubation, bag valve mask ventilation, needle thoracostomy (NT), or cardiac arrest during transport.
Methods: We conducted a retrospective review of a case-series of trauma patients transported to a single Level 1 trauma center via RW with confirmed PTX and no TT. Using standardized abstraction forms, we reviewed charts for signs of deterioration. Those patients identified as having clinical deterioration were independently reviewed for the likelihood that the clinical deterioration was a direct consequence of PTX.
Results: During the study period, 66 patients with confirmed PTX underwent RW AMT with an average altitude gain of 1890 feet, an average barometric pressure 586-600 mmHg, and average flight duration of 28 minutes. All patients received oxygen therapy; 14/66 patients (21%) were supported with positive pressure ventilation. Eleven of 66 patients (17%) had NT placed before flight and 4/66 (6%) had NT placed during flight. Four of 66 patients (6% CI0.3-11.7) may have deteriorated during AMT as a result of PTX; all were successfully managed with NT.
Conclusions: In this series, 6% of patients with PTX deteriorated as result of AMT without TT, yet all patients were managed successfully with NT. Routine placement of TT in patients with PTX before RW AMT may not be necessary. Further prospective evaluation is warranted.
| Tags : pneumothorax, drainage thorax
03/06/2015
Par le côté et avec du long ?
Evaluation of 8.0-cm needle at the fourth anterior axillary line for needle chest decompression of tension pneumothorax
Chang SJ et Al. J Trauma Acute Care Surg. 2014;76: 1029-1034
----------------------------------------------------------------------------
La décompression d'un thorax sous pression doit maintenant se faire par voie latérale, la voie antérieure étant associée à un taux d'échec important notamment avec l'emploi de cathéters veineux classiques dont la longueur est rarement supérieure à 5 cm. Le recours à des cathéters de 8 cm est ainsi prôné dans la littérature anglo-saxone sur des seuls arguments anatomiques. Le risque de ponction de structures intrathoraciques est réel et doit rendre mesuré quand au recours à de tels dispositifs. On rappelle que la thoracostomie au doigt doit être considérée comme la référence.
| Tags : exsufflation, pneumothorax
24/04/2015
Pneumothorax: Passez par le côté
Failed needle decompression of bilateral spontaneous tension pneumothorax
Bac PT et Al. Acta Anaesthesiol Scand. 2015 Apr 21. doi: 10.1111/aas.12538. [Epub ahead of print]
-------------------------------------------------
Cet article a le mérite de rappeler que la détresse respiratoire est ua prmeier plan enc as de pneumothorax suffocant chez le patient non ventilé, que la voie latérale doit être privilégié et surtout que la thoracostomie simple est parfaitement efficace.
-------------------------------------------------
This case report presents a young male admitted with primary bilateral spontaneous tension pneumothorax and severe respiratory distress. This is an extremely rare condition. The patient was on the verge of hypoxic cardiac arrest and the attempted needle thoracocentesis was unsuccessful. Needle thoracocentesis in the midclavicular line of the second intercostal space is widely used and recommended as first-line treatment of tension pneumothorax. Reviewing the literature, the procedure is not based on solid evidence. It has high failure rates and potentially serious complications. Alternatives to this approach are perhaps more appropriate. Correctly done, needle thoracocentesis has its place in the presence of a diagnosed or suspected tension pneumothorax when no other options are available. If needle thoracocentesis is chosen, then insertion in the mid-anterior axillary line of the 3rd–5th intercostal space is an appropriate alternative site. Otherwise, lateral thoracostomy, with or without chest tube insertion, is a safe procedure with a high success rate. It should be considered as the first-line treatment of tension pneumothorax, particularly in the unstable patient
| Tags : pneumothorax, exsufflation
10/03/2015
Pansements 3 côtés: C'est efficace
Vented Chest Seals for Prevention of Tension Pneumothorax in a Communicating Pneumothorax
Kotora JG et Al. J Emerg Med. 2013 Nov;45(5):686-94.
--------------------------------------------------------------------------------------------------------------------
La prise en charge d'une plaie thoracique soufflante (1) est une éventualité peu fréquente qui expose d'une part au risque de détresse respiratoire aiguë et d'autre part au risque d'instabilité hémodynamique en rapport avec le caractère compressif d'un épanchement intra-thoracique gazeux ou liquidien (2) L'exsufflation et/ou la pose d'un pansement 3 côtés sont alors requis. Ce dernier peut être réalisé simplement ou par l'emploi de dispositifs commerciaux prêts à l'emploi. Le travail présenté exprime l'efficacité des pansements "3 côtés" de dernières générations aussi bien en matière d'adhérence cutanée que d'efficacité d'évacuation de l'air et secrétions intra-thoraciques. Ils jouent donc ainsi parfaitement le rôle pour lesquels ils ont été conçus (3).
--------------------------------------------------------------------------------------------------------------------
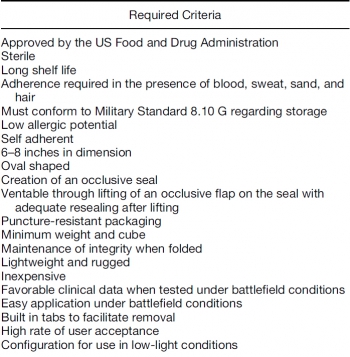
BACKGROUND:
Tension pneumothorax accounts for 3%–4% of combat casualties and 10% of civilian chest trauma. Air entering a wound via a communicating pneumothorax rather than by the trachea can result in respiratory arrest and death. In such cases, the Committee on Tactical Combat Casualty Care advocates the use of unvented chest seals to prevent respiratory compromise.
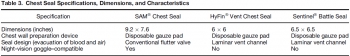
OBJECTIVE: A comparison of three commercially available vented chest seals was undertaken to evaluate the efficacy of tension pneumothorax prevention after seal application.
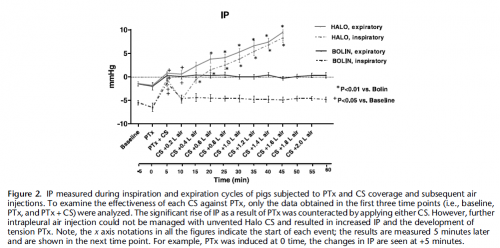
METHODS:
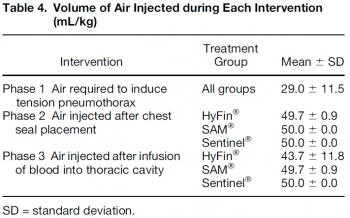
A surgical thoracostomy was created and sealed by placing a shortened 10-mL syringe barrel (with plunger in place) into the wound. Tension pneumothorax was achieved via air introduction through a Cordis to a maximum volume of 50 mL/kg. A 20% drop in mean arterial pressure or a 20% increase in heart rate confirmed hemodynamic compromise. After evacuation, one of three vented chest seals (HyFin ®, n = 8; Sentinel ®, n = 8, SAM ®, n = 8) was applied. Air was injected to a maximum of 50 mL/kg twice, followed by a 10% autologous blood infusion, and finally, a third 50 mL/kg air bolus. Survivors completed all three interventions, and a 15-min recovery period.
RESULTS:
The introduction of 29.0 (±11.5) mL/kg of air resulted in tension physiology. All three seals effectively evacuated air and blood. Hemodynamic compromise failed to develop with a chest seal in place.
CONCLUSIONS:
HyFin ®, SAM ®, and Sentinel ® vented chest seals are equally effective in evacuating blood and air in a communicating pneumothorax model. All three prevented tension pneumothorax formation after penetrating thoracic trauma
| Tags : pneumothorax, exsufflation
23/02/2015
Pneumo suffocant: Oui
Clic sur l'image pour accéder au document
Pneumothorax compressif, sous tension, tamponnade gazeuse. Autant de termes utilisés pour cette situation clinique à laquelle est souvent associé l'existence d'une hypotension artérielle, en fait surtout présente chez les patients ventilés. La détresse respiratoire est souvent au premier plan che le blessé non ventilé et le terme de pneumothorax suffocant adapté. Le document proposé est un peu ancien mais apporte une vision relativement didactique de la problématique séméiologique et physiopathologique.
| Tags : pneumothorax
28/12/2014
Un trocard de coelio ?
Standard laparoscopic trocars for the treatment of tension pneumothorax: A superior alternative to needle decompression
Quinton H. et Al. J Trauma Acute Care Surg. 2014;77: 170-175.
-------------------------------------------------------
Le recours à un cathéter d'au moins 8 cm est prôné par certains du fait de l'épaisseur de la paroi thoracique. L'inconvénient de cette longueur est le risque non négligeable de ponction parenchymateuse surtout lors de l'emploi de la voie antérieure.
La voie latérale exposerait maoins à ce risque. Une alternative bien moins dangereuse et toute aussi efficace est la thoracostomie au doigt. Et pourquoi pas un trocard de coelio ?
-------------------------------------------------------
BACKGROUND: Needle thoracostomy (NT) is a commonly taught intervention for tension pneumothorax (tPTX) but has a high failure rate. We hypothesize that standard 5-mm laparoscopic trocars may be a safe and more effective alternative.
METHODS: Thirty episodes of tPTX and 27 episodes of tension-induced pulseless electrical activity (PEA) were induced in five adult swine using thoracic CO2 insufflation via balloon trocar. Tension was defined as a 50% decrease in cardiac output. Chest decompression was performed with 5-mm laparoscopic trocars for the treatment of both tPTX with hemodynamic compromise and tension-induced PEA. The lungs and heart were inspected and graded at necropsy for trocar-related injury. Results were also compared with success rates with NT in the same model.
RESULTS: The placement of a 5-mm trocar rapidly and immediately relieved tension physiology in 100% of the cases. Mean arterial pressure, cardiac output, central venous pressure, and pulmonary capillary wedge pressure all returned to baseline within 1 minute of trocar placement. Adequate perfusion was restored in 100% of tension-induced PEA cases within 30 seconds of trocar placement. There was no evidence of trocar-related heart or lung damage in any of the experimental animals at necropsy (mean injury scores, 0 for both). Fivemillimeter trocars significantly outperformed standard NT for both tPTX and tension-induced PEA arrest.
CONCLUSION: tPTX and tension-induced PEA can be safely and effectively treated with chest decompression using 5-mm laparoscopic trocars. This technique may serve as a more rapid and reliable alternative to needle decompression.
| Tags : pneumothorax
17/11/2014
Pneumothorax et vol en altitude : Possible ?
Cleared for takeoff: The effects of hypobaric conditions on traumatic pneumothoraces
Majercik S. et All. J Trauma Acute Care Surg. 2014;77: 729-733
| Tags : pneumothorax
13/11/2014
Drain thoracique: Confirmation, pas si simple
An audit of the complications of intercostal chest drain insertion in a high volume trauma service in South Africa.
Kong V. et All. Ann R Coll Surg Engl. 2014 Nov;96(8):609-13
Intercostal chest drain (ICD) insertion is a commonly performed procedure in trauma and may be associated with significant morbidity.
METHODS:
This was a retrospective review of ICD complications in a major trauma service in South Africa over a four-year period from January 2010 to December 2013.
RESULTS:
clic sur l'image pour accéder au document SAMU 69
A total of 1,050 ICDs were inserted in 1,006 patients, of which 91% were male. The median patient age was 24 years (interquartile range [IQR]: 20-29 years). There were 962 patients with unilateral ICDs and 44 with bilateral ICDs. Seventy-five per cent (758/1,006) sustained penetrating trauma and the remaining 25% (248/1006) sustained blunt trauma. Indications for ICD insertion were: haemopneumothorax (n=338), haemothorax (n=314), simple pneumothorax (n=265), tension pneumothorax (n=79) and open pneumothorax (n=54). Overall, 203 ICDs (19%) were associated with complications: 18% (36/203) were kinked, 18% (36/203) were inserted subcutaneously, 13% (27/203) were too shallow and in 7% (14/203) there was inadequate fixation resulting in dislodgement. Four patients (2%) sustained visceral injuries and two sustained vascular injuries. Forty-one per cent (83/203) were inserted outside the 'triangle of safety' but without visceral or vascular injuries. One patient had the ICD inserted on the wrong side. Junior doctors inserted 798 ICDs (76%) while senior doctors inserted 252 (24%). Junior doctors had a significantly higher complication rate (24%) compared with senior doctors (5%) (p<0.001). There was no mortality as a direct result of ICD insertion. </sec> Conclusions ICD insertion is associated with a high rate of complications. These complications are significantly higher when junior doctors perform the procedure. A multifaceted quality improvement programme is needed to improve the situation.
| Tags : drainage thorax
12/01/2014
Exsufflation: 1 / 4 sans pneumothorax !
Inadequate Needle Thoracostomy Rate in the Prehospital Setting for Presumed Pneumothorax. An Ultrasound Study
Blaivas M. J Ultrasound Med 2010; 29:1285–1289
---------------------------------------------------------------------
Nombreux ont attiré l'attention sur le risque d'inefficacité des exsufflations au cathéter à cause de la longueur de ces derniers, plus court que l'épaisseur de la paroi thoracique. Certains prônent l'emploi de cathéter de plus de 8 cm sans véritablement de fondements scientifiques (Lire cette analyse). Entre des mains peu expérimentées cette pratique apparaît dangereuse du fait du fait des erreurs faites sur les niveaux de ponction, ce d'autant que ces cathéters ne sont pas très efficaces dans le temps. L'article proposé incite encore plus à la nécessaire prudence à avoir avant de faire pénétrer une aiguille dans un thorax. En effet ce geste serait pratiqué 1 fois sur 4 en l'absence de pneumothorax.
---------------------------------------------------------------------
Objective. The purpose of this study was to evaluate the frequency of inadequate needle chest tho-racostomy in the prehospital setting in trauma patients suspected of having a pneumothorax (PTX) onthe basis of physical examination.
Methods. This study took place at a level I trauma center. All trauma patients arriving via emergency medical services with a suspected PTX and a needle thoracostomy were evaluated for a PTX with bedside ultrasound. Patients too unstable for ultrasound evaluation before tube thoracostomy were excluded, and convenience sampling was used. All patients were scanned while supine. Examinations began at the midclavicular line and included the second through fifth ribs. If no sliding lung sign (SLS) was noted, a PTX was suspected, and the lung point was sought for definitive confirmation. When an SLS was noted throughout and a PTX was ruled out on ultrasound imaging, the thoracostomy catheter was removed. Descriptive statistics were calculated.
Results. A total of 57 patients were evaluated over a 3-year period. All had at least 1 needle thoracostomy attempted; 1 patient underwent 3 attempts. Fifteen patients (26%) had a normal SLS on ultrasound examination and no PTX after the thoracostomy catheter was removed. None of the 15 patients were later discovered to have a PTX on subsequent computed tomography. Conclusions. In this study, 26% of patients who received needle thoracostomy in the prehospital setting for a suspected PTX appeared not to have had a PTX originally, nor had 1 induced by the needle thoracostomy. It may be prudent to evaluate such patients with bedside ultrasound instead of automatically converting all needle thoracostomies to tube thoracostomies.
---------------------------------------------------------------------
Recourir à l'échographie pleurale et réaliser ce geste par voie latérale avec un cathéter de 5 cm apparaissent être sécuritaire.
| Tags : exsufflation, decompression
20/12/2013
Drainage et thoracocentèse
Chest Drainage
McDermott S. et Al. Semin Intervent Radiol 2012;29:247–255
Infectious, traumatic, or neoplastic processes in the chest often result in fluid collections within the pleural, parenchymal, or mediastinal spaces. The same fundamental principles that guide drainages of the abdomen can be applied to the chest. This review discusses various pathologic conditions of the thorax that can result in the abnormal accumulation of fluid or air, and their management using image-guided methods.
10/12/2013
Thoracostomie au doigt: Le mieux !
Simple thoracostomy in prehospital trauma management is safe and effective: a 2-year experience by helicopter emergency medical crews
Massaruttia D et Al. Eur J Emerg Med. 2006 Oct;13(5):276-80
-----------------------------------------------------------------------
La réalisation d'une exsufflation à l'aiguille bien que classique reste discutable du fait de nombreux problèmes techniques et du caractère très relatif de son efficacité. La thoracostomie au doigt doit être considérée comme la technique de référence.
-----------------------------------------------------------------------
OBJECTIVE:
To evaluate the effectiveness and potential complications of simple thoracostomy, as first described by Deakin, as a method for prehospital treatment of traumatic pneumothorax.
METHODS:
Prospective observational study of all severe trauma patients rescued by our Regional Helicopter Emergency Medical Service and treated with on-scene simple thoracostomy, over a period of 25 months, from June 1, 2002 to June 30, 2004.
RESULTS:
Fifty-five consecutive severely injured patients with suspected pneumothorax and an average Revised Trauma Score of 9.6+/-2.7 underwent field simple thoracostomy. Oxygen saturation significantly improved after the procedure (from 86.4+/-10.2% to 98.5%+/-4.7%, P<0.05). No difference exists in the severity of thoracic lesions between patients with systolic arterial pressure and oxygen saturation below and above or equal to 90. A pneumothorax or a haemopneumothorax was found in 91.5% of the cases and a haemothorax in 5.1%. No cases of major bleeding, lung laceration or pleural infection were recorded. No cases of recurrent tension pneumothorax were observed. Forty (72.7%) patients survived to hospital discharge.
CONCLUSIONS:
Prehospital treatment of traumatic pneumothorax by simple thoracostomy without chest tube insertion is a safe and effective technique.
| Tags : pneumothorax
01/09/2013
Pneumothorax: Pansement NON OCCLUSIF
Vented versus unvented chest seals for treatment of pneumothorax and prevention of tension pneumothorax in a swine model
Kheirabadi BS et all. J Trauma Acute Care Surg. 2013;75: 150-156
La procédure du sauvetage au combat indique qu'un thorax ouvert ne doit JAMAIS être fermé et qu'un pansement 3 côtés doit être mis en place pour éviter toute surpression intrathoracique. Ceci diffère du TCCC américain qui recommande l'occlusion de la plaie et la surveillance du blessé à la recherche d'un pneumothorax suffocant. Mais les choses évoluent à la lumière de la remise en question de pratiques pas toujours bien documentées. Le TCCC va proposer le recours non pas à l'emploi d'un pansement 3 côtés consommateur de temps mais à l'utilisation de pansements adhésifs prêts à l'emploi.
L'article présenté montre très clairement l'intérêt de la mise en place de pansement permettant l'évacuation de l'air intrathoracique.
Au delà de l'intérêt des dispositifs prêts à l'emploi avec valve de surpression, il y a le problème du choix du modèle. La procédure du sauvetage au combat propose la valve d'asherman, qui doit être considérée comme obsolète car bien qu'efficace, sa capacité d'adhésion à la peau est perfectible. Il semble que les modèles concurrents (Hyfin Vent Chest Seal, SAM chest seal et Sentinel chest seal) proposés par l'industrie aient la même efficacité
| Tags : exsufflation, pneumothorax, matériel
02/07/2013
Pneumothorax: Dès 10 mmHg
Physiology and cardiovascular effect of severe tension pneumothorax in a porcine model
Nelson D et all. J Surg Res. 2013 Jun 5. pii: S0022-4804(13)00505-2
BACKGROUND:
Pneumothoraces are relatively common among trauma patients and can rapidly progress to tension physiology and death if not identified and treated. We sought to develop a reliable and reproducible large animal model of tension pneumothorax and to examine the cardiovascular effects during progression from simple pneumothorax to tension pneumothorax.
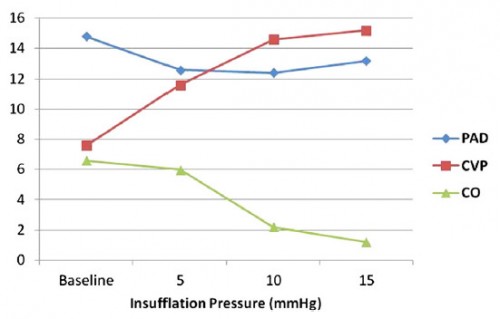
MATERIALS AND METHODS:
Ten swine were intubated, sedated, and placed on mechanical ventilation. After a midline celiotomy, a 10-mm balloon-tipped laparoscopic trocar was placed through the diaphragm, and a 28F chest tube was placed in the standard position and clamped. Thoracic insufflation was performed in 5-mm increments, and continuous cardiovascular measurements were obtained.
RESULTS:
Mean insufflation pressures of 10 mm Hg were associated with a 67% decrease in cardiac output (6.6 L/min versus 2.2 l/min; P = 0.04). An additional increase in the insufflation pressure (mean 15 mm Hg) was associated with an 82% decrease in cardiac output from baseline (6.8 versus 1.2 L/min; P < 0.01). Increasing insufflation pressures were associated with a corresponding increase in central venous pressure (from 7.6 mm Hg to 15.2 mm Hg; P < 0.01) and a simultaneous decrease in the pulmonary artery diastolic pressure (from 15 mm Hg to 12 mm Hg; P = 0.06), with the central venous pressure and pulmonary artery diastolic pressure approaching equalization immediately before the development of major hemodynamic decline. Pulseless electrical activity arrest was induced at an average of 20 mm Hg. Tension physiology was immediately reversible with adequate decompression, allowing for multiple repeated trials.
CONCLUSIONS:
A reliable and highly reproducible model was created for severe tension pneumothorax in a large animal. Major cardiovascular instability proceeding to pulseless electrical activity arrest with stepwise insufflation was noted. This model could be highly useful for studying new diagnostic and treatment modalities for tension pneumothorax.
| Tags : pneumothorax