14/11/2021
Décompression thoracique: 7 cm !
Prehospital Decompression of Pneumothorax: A Systematic Review of Recent Evidence
Robitaille-Fortin M et Al. Prehosp Disaster Med. 2021 Aug;36(4):450-459.
Introduction:
Pneumothorax remains an important cause of preventable trauma death. The aim of this systematic review is to synthesize the recent evidence on the efficacy, patient outcomes, and adverse events of different chest decompression approaches relevant to the out-of-hospital setting.
Methods:
A comprehensive literature search was performed using five databases (from January 1, 2014 through June 15, 2020). To be considered eligible, studies required to report original data on decompression of suspected or proven traumatic pneumothorax and be considered relevant to the prehospital context. They also required to be conducted mostly on an adult population (expected more than ≥80% of the population ≥16 years old) of patients. Needle chest decompression (NCD), finger thoracostomy (FT), and tube thoracostomy were considered. No meta-analysis was performed. Level of evidence was assigned using the Harbour and Miller system.
Results:
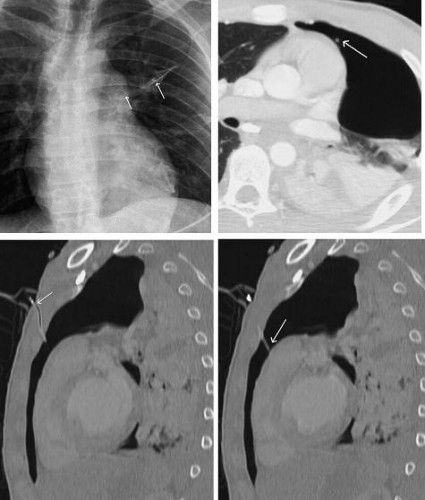
A total of 1,420 citations were obtained by the search strategy, of which 20 studies were included. Overall, the level of evidence was low. Eleven studies reported on the efficacy and patient outcomes following chest decompression. The most studied technique was NCD (n = 7), followed by FT (n = 5). Definitions of a successful chest decompression were heterogeneous. Subjective improvement following NCD ranged between 18% and 86% (n = 6). Successful FT was reported for between 9.7% and 32.0% of interventions following a traumatic cardiac arrest. Adverse events were infrequently reported. Nine studies presented only on anatomical measures with predicted failure and success. The mean anterior chest wall thickness (CWT) was larger than the lateral CWT in all studies except one. The predicted success rate of NCD ranged between 90% and 100% when using needle >7cm (n = 7) both for the lateral and anterior approaches. The reported risk of iatrogenic injuries was higher for the lateral approach, mostly on the left side because of the proximity with the heart.
Conclusions:
Based on observational studies with a low level of evidence, prehospital NCD should be performed using a needle >7cm length with either a lateral or anterior approach. While FT is an interesting diagnostic and therapeutic approach, evidence on the success rates and complications is limited. High-quality studies are required to determine the optimal chest decompression approach applicable in the out-of-hospital setting.
| Tags : décompression
12/01/2014
Exsufflation: 1 / 4 sans pneumothorax !
Inadequate Needle Thoracostomy Rate in the Prehospital Setting for Presumed Pneumothorax. An Ultrasound Study
Blaivas M. J Ultrasound Med 2010; 29:1285–1289
---------------------------------------------------------------------
Nombreux ont attiré l'attention sur le risque d'inefficacité des exsufflations au cathéter à cause de la longueur de ces derniers, plus court que l'épaisseur de la paroi thoracique. Certains prônent l'emploi de cathéter de plus de 8 cm sans véritablement de fondements scientifiques (Lire cette analyse). Entre des mains peu expérimentées cette pratique apparaît dangereuse du fait du fait des erreurs faites sur les niveaux de ponction, ce d'autant que ces cathéters ne sont pas très efficaces dans le temps. L'article proposé incite encore plus à la nécessaire prudence à avoir avant de faire pénétrer une aiguille dans un thorax. En effet ce geste serait pratiqué 1 fois sur 4 en l'absence de pneumothorax.
---------------------------------------------------------------------
Objective. The purpose of this study was to evaluate the frequency of inadequate needle chest tho-racostomy in the prehospital setting in trauma patients suspected of having a pneumothorax (PTX) onthe basis of physical examination.
Methods. This study took place at a level I trauma center. All trauma patients arriving via emergency medical services with a suspected PTX and a needle thoracostomy were evaluated for a PTX with bedside ultrasound. Patients too unstable for ultrasound evaluation before tube thoracostomy were excluded, and convenience sampling was used. All patients were scanned while supine. Examinations began at the midclavicular line and included the second through fifth ribs. If no sliding lung sign (SLS) was noted, a PTX was suspected, and the lung point was sought for definitive confirmation. When an SLS was noted throughout and a PTX was ruled out on ultrasound imaging, the thoracostomy catheter was removed. Descriptive statistics were calculated.
Results. A total of 57 patients were evaluated over a 3-year period. All had at least 1 needle thoracostomy attempted; 1 patient underwent 3 attempts. Fifteen patients (26%) had a normal SLS on ultrasound examination and no PTX after the thoracostomy catheter was removed. None of the 15 patients were later discovered to have a PTX on subsequent computed tomography. Conclusions. In this study, 26% of patients who received needle thoracostomy in the prehospital setting for a suspected PTX appeared not to have had a PTX originally, nor had 1 induced by the needle thoracostomy. It may be prudent to evaluate such patients with bedside ultrasound instead of automatically converting all needle thoracostomies to tube thoracostomies.
---------------------------------------------------------------------
Recourir à l'échographie pleurale et réaliser ce geste par voie latérale avec un cathéter de 5 cm apparaissent être sécuritaire.
| Tags : exsufflation, decompression
29/01/2011
Syndrome compartimental du globe oculaire
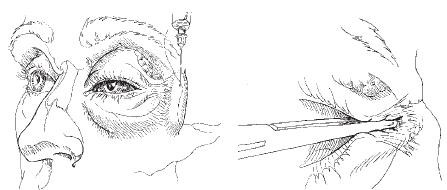
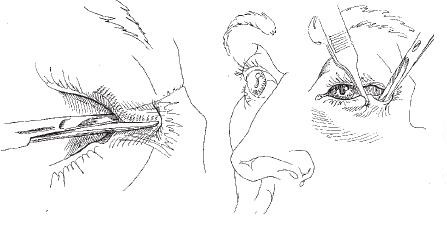
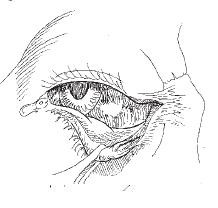
Les syndromes compartimentaux peuvent tuer. On pense bien sûr au syndrome des loges, au syndrome compartimental abdominal. On peut en rapprocher la tamponnade cardiaque, le pneumothorax compressif et les hypertensions intracrâniennes. Il est moins naturel de penser au syndrome compartimental orbitaire. Pourtant un geste simple permet de réduire ce risque lors de trauma de la face, c'est la cantholyse externe.
Voici en quelques schémas comment la réaliser.
En réalisant ce geste simple, vous soulagez la pression intraorbitaire et améliorer la perfusion rétinienne.
| Tags : compartiment, décompression
23/12/2010
Exsufflation: 5 cm suffisent !
Can J Surg. 2010 June; 53(3): 184–188
Ball CG et all.
"
Résumé
Needle thoracostomy decompression was attempted in 1.5% (142/9689) of patients. Among patients with blunt injuries, the incidence was 1.4% (101/7073). Patients transported by helicopter (74%) received a 4.5-cm sheath. The remainder (26% ground transport) received a 3.2-cm catheter. A minority in each group (helicopter 15%, ground 28%) underwent immediate chest tube insertion (before thoracic ultrasound) because of ongoing hemodynamic instability. Failure to decompress the pleural space by NT was observed via ultrasound and/or CT in 65% (17/26) of attempts with a 3.2-cm catheter, compared with only 4% (3/75) of attempts with a 4.5-cm catheter (p < 0.001).
"
Morceau choisi
Although some authors13,16 have called for 7- to 8-cm needles to ensure that all OPTXs are decompressed, it appears that even catheters as short as 4.5 cm can puncture the heart at standard insertion locations in 2.5% of trauma patients.24 Other complications include chest wall hematoma, hemothorax, empyema and dislodgement in up to 8% of patients.18,25 In an attempt to avoid these issues, as well as access the pleural space more reliably, support for axillary NT is increasing.3,18,22,25,39 This lateral location takes advantage of a thinner chest wall (mean 2.6 cm)16 and is the military’s first choice if under fire because it allows medics to keep a soldier’s body armor in place while achieving decompression.40 Although we observed no direct complications in our study, we support the use of a catheter at of least 4.5 cm in length.
Commentaires
Le pneumothorax suffocant est la seconde cause de mort évitable au combat. Sa pris en charge repose sur la décompression de l'air retneu dans la cage thoracique. Outre la thoracostomie au doigt, geste de référence simple et sans danger, il peut être effectué une décompression à l'aiguille. Certains militent pour l'emploi d'un cathéter de grande taille de 8 cm du fait de l'épaisseur de la paroi thoracique, en particulier chez les militaires . Cependant le risque de plaie cardiaque et des gros vaisseaux est relativement important et peut atteindre 2.5% des blessés (1, 2, 3), ce d'autant plus que les ponctions sont habituellement réalisées de manière beaucoup trop médianes.
En condition de combat, une conduite raisonnable est de pratiquer cette exsufflation par voie LATERALE (4) et par ailleurs d'utiliser des cathéters de 5 cm qui apparaissent SUFFISANTS (5)
| Tags : décompression
10/10/2010
Exsufflation à l'aiguille: Pas n'importe comment !
L'exsufflation à l'aiguille en condition de combat diffère de la pratique habituelle. Le combattant est porteur d'effet de protection, l'épaisseur de la paroi thoracique de sujet musclé est importante, le stress lié au combat rend moins serein la réalisation du geste. Aussi est i important de privilégier les abords latéraux, du moins toujours pour les abords antérieurs un point de ponction situé en dehors d'une ligne passant par le mamelon et d'une ligne passant par la fourchette sternale. Ceci diffère des repères habituels dont l'emploi peut être source de de ponctions trop médianes génératrices de complications.
Les dangers d'une exsufflation à l'aiguille mal conduite
| Tags : décompression