20/04/2013
Coniotomie: Avant tout de bons repères
La réalisation d'une coniotomie en conditions extrêmes n'est pas une chose si aisée que cela. Bien souvent l'opérateur peut être obnubilé par le fait de faire pénétrer un tuyau dans un trou alors que ce qui est important c'est le trou au bon endroit et de taille suffisamment large pour admettre le tuyau. Au final ce qui est FONDAMENTAL c'est donc de prendre ses repères et de vérifier le diamêtre de l'ouverture faite.
C'est ce qu'exprime ce document intéressant et très pratique dont l'un des auteurs est un des inventeurs d'une technqiue de trachéotomie percutanée.
_________________________________________
The first step of the ‘scalpel–finger–tube’ method is to stabilize the larynx with the non-dominant hand, identify the cricothyroid membrane visually and by palpation, and to incise horizontally all the way through skin and cricothyroid membrane into the laryngeal lumen in one motion (Fig. 1).
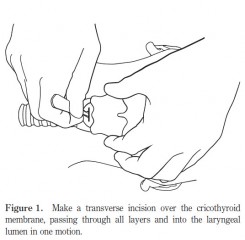
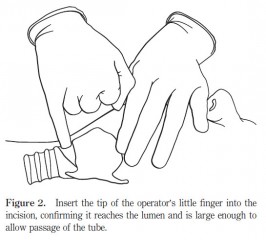
In the emergency situation, neither skin antiseptics nor local anaesthesia are used.Any suitable blade can be used, either on or off the handle. The incision is extended laterally until judgedlarge enough to accommodate the tip of the operator’s gloved little finger, that is, approximately 15 mm. The second step is to remove the scalpel and insert the tip of the operator’s little finger into the incision (Fig. 2), confirming by palpation that the incision has penetratedinto the laryngeal lumen, and that the incision is large enough to accommodate the finger, and therefore, an endotracheal tube.
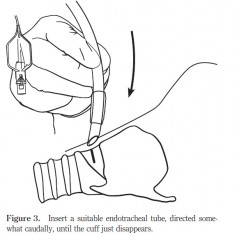
Finally, in the third step, a cuffed oral endotracheal tube is fed through the hole into the trachea, directed somewhat caudally (Fig. 3)
| Tags : airway, coniotomie
08/11/2012
Coniotomie: Pas le kit PCK
Emergency cricothyroidotomy performed by inexperienced clinicians--surgical technique versus indicator-guided puncture technique
Emerg Med J. 2012 Jul 27. [Epub ahead of print]
Abstract
Background To improve the ease and safety of cricothyroidotomy especially in the hand of the inexperienced, new instruments have been developed. In this study, we compared a new indicator-guided puncture technique (PCK) with standard surgical technique (ST) regarding success rate, performance time and complications.
Methods Cricothyroidotomy in 30 human cadavers performed by 30 first year anaesthesia residents. The set chosen for use was randomised: PCK-technique (n=15) and ST (n=15). Success rates, insertion times and complications were compared. Traumatic lesions were anatomically confirmed after dissection.
Results The ST-group had a higher success rate (100% vs 67%; p=0.04). There was no difference in time taken to complete the procedure (PCK 82 s. vs ST 95 s.; p=0.89). There was a higher complication rate in the PCK-group (67% vs 13%; p=0.04). Most frequent complication in the PCK-group was injury to the posterior tracheal wall (n=8), penetration to the oesophageal lumen (n=4) and injury to the thyroid and/or cricoid cartilage (n=5). In the ST-group in only 2 cases minor complications were observed (small vessel injury).
Conclusions In this human cadaver study the PCK technique produced more major complications and more failures than the ST. In the hand of the inexperienced operator the standard surgical approach seems to be a safe procedure, which can successfully be performed within an adequate time. The PCK technique cannot be recommended for inexperienced operators.
07/04/2012
Coniotomie et analyse cognitive de taches
L’analyse cognitive de tâches est une « famille de techniques de recueil de connaissances qui ont démontrées leur efficacité pour extraire les processus cognitifs, décisionnels et de jugements inobservables impliqués lors d’une performance d’expert» (Yates 2007). L’intérêt de ce groupe de techniques est de rendre accessible à la conscience l’ensemble des étapes réalisées de façon automatiques par des experts.
Cette méthode moderne d'enseignement est très certainement d'un apport capital pour l'enseignement du sauvetage au combat. Ainsi il semble qu'elle peut s'appliquer à la coniotomie. C'est du moins ce que laisse supposer l'article suivant.
The effectiveness of a cognitive task analysis informed curriculum to increase self-efficacy and improve performance for an open cricothyrotomy.
Campbell J.. et all J Surg Educ. 2011 Sep-Oct;68(5):403-7
Abstract
OBJECTIVE:
This study explored the effects of a cognitive task analysis (CTA)-informed curriculum to increase surgical skills performance and self-efficacy beliefs for medical students and postgraduate surgical residents learning how to perform an open cricothyrotomy.
METHODS:
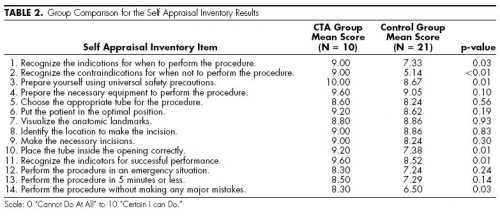
Third-year medical students and postgraduate year 2 and 3 surgery residents were assigned randomly to either the CTA group (n = 12) or the control group (n = 14). The CTA group learned the open cricothyrotomy procedure using the CTA curriculum. The control group received the traditional curriculum.
RESULTS:
The CTA group outperformed the control group significantly based on a 19-point checklist score (CTA mean score: 17.75, standard deviation [SD] = 2.34; control mean score: 15.14, SD = 2.48; p = 0.006). The CTA group also reported significantly higher self-efficacy scores based on a 140-point self-appraisal inventory (CTA mean score: 126.10, SD = 16.90; control: 110.67, SD = 16.8; p = 0.029).
CONCLUSIONS:
The CTA curriculum was effective in increasing the performance and self-efficacy scores for postgraduate surgical residents and medical students performing an open cricothyrotomy.
| Tags : airway, coniotomie
12/11/2011
Cause de décès en afghanistan: Actualités canadiennes
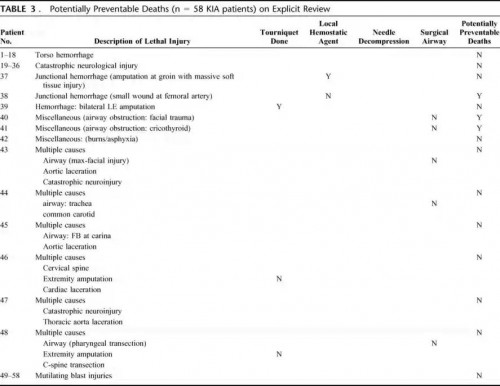
Causes of Death in Canadian Forces Members Deployed to Afghanistan and Implications on Tactical Combat Casualty Care Provision
Pannell D et all. J Trauma. 2011;71: S401–S407
Ce document identifie par ailleurs l'importance de la formation des personels à la gestion des voies aériennes, des mesures de stabilisation du rachis en cas d'IED, du recours aux sondes de foley pour le tamponenment des hémorragies jonctionnelles en cas de non application possible de pansement hémostatique.
-------Morceaux choisis:
We recommend that combat medical technicians should continue to practice surgical airways in live-tissue laboratories. In addition, didactic teaching should continue to review the indications for cricothyrotomy on the battlefield. .........
...... Based on this review, we also feel that future Canadian TCCC courses may be improved by giving battlefield providers a treatment option for dealing with exsanguination from small wounds at junctional areas (groin, axillary, and neck). Currently, TCCC providers only have hemostatic dressings to deal with this difficult problem. However, unfavorable wound geometry can make utilization of these products unfeasible. In addition, TCCC providers have no option for treating carotid artery hemorrhage in the neck. We suggest that combat medical technicians also carry urinary catheters; these can be inserted into wound tracts of small wounds. Insufflation of the balloon may provide temporary hemostasis of junctional bleeding and buy enough time for evacuation to a definitive surgical facility. Another option would be to pack such wounds with ribbon gauze. These options may also be used for posterior packing of lifethreatening epistaxis associated with facial fractures.
On our review, we also noted that three casualties.....
....we recommend that spinal immobilization be considered for all casualties suffering from blunt trauma or IED-related incidents during “Tactical Field Care,” if the tactical situation permits, and if the medical technician deems the situation to be safe enough to proceed with this procedure.
08/09/2011
Alternative à l'intubation: D'abord la coniotomie chirurgicale !
A meta-analysis of prehospital airway control technique part II: alternative airway devices and cricothyrotomy success rate. Hubble MW et all. Prehosp Emerg Care. 2010 Oct-Dec;14(4):515-30.
Ce document est une métaanalyse récente qui le point dans la littérature sur les alternatives à l'intubation. Elle confirme que la coniotomie chirurgicale est la technique de référence. Elle précise que le tube de King est le dispositiflaryngé le plus pertinent mais qu'il manque globalement de recul sur ces dispositifs.
BACKGROUND:
Airway management is a key component of prehospital care for seriously ill and injured patients. Oral endotracheal intubation (OETI) is the definitive airway of choice in most emergency medical services (EMS) systems. However, OETI may not be an approved skill for some clinicians or may prove problematic in certain patients because of anatomic abnormalities, trauma, or inadequate relaxation. In these situations alternative airways are frequently employed. However, the reported success rates for these devices vary widely, and established benchmarks are lacking.
OBJECTIVE:
We sought to determine pooled estimates of the success rates of alternative airway devices (AADs) and needle cricothyrotomy (NCRIC) and surgical cricothyrotomy (SCRIC) placement through a meta-analysis of the literature.We sought to determine pooled estimates of the success rates of alternative airway devices (AADs) and needle cricothyrotomy (NCRIC) and surgical cricothyrotomy (SCRIC) placement through a meta-analysis of the literature.
METHODS:
We performed a systematic literature search for all English-language articles reporting success rates for AADs, SCRIC, and NCRIC. Studies of field procedures performed by prehospital personnel from any nation were included. All titles were reviewed independently by two authors using prespecified inclusion criteria. Pooled estimates of success rates for each airway technique were calculated using a random-effects meta-analysis model.
RESULTS:
Of 2,005 prehospital airway titles identified, 35 unique studies were retained for analysis of AAD success rates, encompassing a total of 10,172 prehospital patients. The success rates for SCRIC and NCRIC were analyzed across an additional 21 studies totaling 512 patients. The pooled estimates (and 95% confidence intervals [CIs]) for intervention success across all clinicians and patients were as follows: esophageal obturator airway-esophageal gastric tube airway (EOA-EGTA) 92.6% (90.1%-94.5%); pharyngeotracheal lumen airway (PTLA) 82.1% (74.0%-88.0%); esophageal-tracheal Combitube (ETC) 85.4% (77.3%-91.0%); laryngeal mask airway (LMA) 87.4% (79.0%-92.8%); King Laryngeal Tube airway (King LT) 96.5% (71.2%-99.7%); NCRIC 65.8% (42.3%-83.59%); and SCRIC 90.5% (84.8%-94.2%).
CONCLUSIONS:
We provide pooled estimates for prehospital AAD, NCRIC, and SCRIC airway interventions. Of the AADs, the King LT demonstrated the highest insertion success rate (96.5%), although this estimate is based on limited data, and data regarding its ventilatory effectiveness are lacking; more data are available for the ETC and LMA. The ETC, LMA, and PTLA all had similar-but lower-success rates (82.1%-87.4%). NCRIC has a low rate of success (65.8%); SCRIC has a much higher success rate (90.5%) and should be considered the preferred percutaneous rescue airway.
14/12/2010
Abord des voies aériennes:Que font les anglais ?
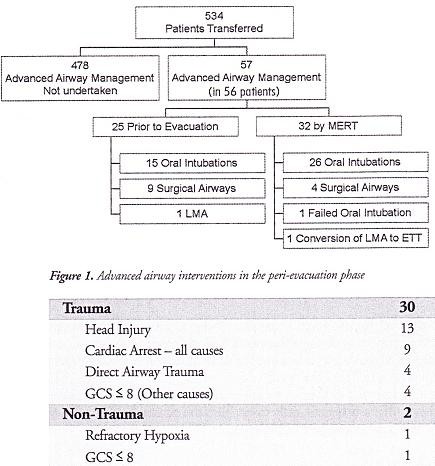
10 % des blessés évacués nécessite une intubation dont 4.7% avant l'embarquement dans le vecteur d'évacuation. Dans ce travail la limite est que nous ne savons pas ce qui relève de blessés au combat , s'il s'agit de blessés militaires, de la répartition des procédures en fonction du contexte. Dans de telles conditions la prise en charge de patients/blessés en arrêt circulatoire est vaine .
J R Army Med Corps. 2010 Sep;156(3):159-61.
Advanced airway management--a medical emergency response team perspective.
Selly Oak Hospital, Birmingham. aghaldane1@doctors.org.uk
Abstract
OBJECTIVES: To determine the number of medical emergency response team (MERT) patients undergoing advanced airway management in the peri-evacuation phase and to determine the indications for airway interventions undertaken in flight.
METHODS: This was a retrospective study. Data was collected from patient report and mission debrief forms completed after each MERT mission during Operation HERRICK 10 (April-October 2009). All patients that received advanced airway interventions before or during evacuation were identified.
RESULTS: MERTs were involved in the primary transfer of 534 patients during the period studied, 56 (10.5%) underwent advanced airway management, of which 31 (5.8% of total) were initiated by the MERT in the peri-evacuation phase. Twenty five cases (4.7%) underwent advanced airway management by other pre-hospital providers prior to MERT arrival. Of the 31 advanced airway interventions undertaken in-flight, cardiac arrest was the primary indication in only nine cases.
CONCLUSIONS: The figure of 56 patients requiring advanced airway management is at the higher end of the range expected from the study of historical military data. This may reflect the doctrine of "intelligent tasking", that is sending this physician-led team to the most seriously injured casualties.
Morceaux choisis
1. Intubation et coniotomie sont la base
2. Les indications diffèrent de la médecine préhospitalière civile
"..
The indications for those advanced airway interventions undertaken by the MERT is in keeping with the historical data: Head injury making the biggest group once those inrubated for post-operative resplratory support ie those transferred post-operatively from an FST location rather than direct from the point of wounding are excluded . The majoriry of the cases were trauma (93,5%) with the remaining non-traula causes (6,5%) (table 1); This figure is again similar io the recent US study [11].
.."
| Tags : airway, intubation
06/12/2010
Protection des voies aériennes en urgence: Une synthèse à lire
Protection des voies aériennes en médecine d’urgence
Journal Européen des Urgences (2010) 23, 44—56
X. Combes, P. Jabre, F. Soupizet
Le résumé
Le contrôle des voies aériennes des patients présentant une détresse vitale est très souvent nécessaire en médecine d’urgence. L’intubation orotrachéale est la technique de référence pour le contrôle des voies aériennes. En dehors du cadre de la réanimation de l’arrêt cardiaque, l’intubation trachéale doit être reéalisée sur un patient sédaté et curarisé selon la technique d’intubation en séquence rapide. L’intubation en urgence est une intubation à risques. L’inhalation pulmonaire et les épisodes de désaturation artérielle profonde sont les deux complications les plus fréquemment associées à ce geste. En médecine d’urgence, l’intubation difficile, rarement prévisible, est plus fréquente qu’au bloc opératoire. La prise en charge de
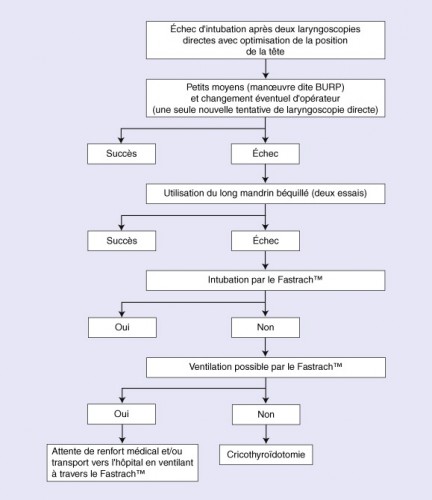
l’intubation difficile survenant dans le cadre de la médecine d’urgence repose sur l’utilisation de techniques alternatives efficaces. Ces techniques doivent être utilisées selon un algorithme précis. Les mandrins longs béquillés et le masque laryngé d’intubation de type Fastrach TM permettent de résoudre la majorité des cas d’intubation difficile. En cas d’échec de ces deux techniques, une cricothyroïdotomie permettant un abord trachéal direct doit être réalisée chez les patients impossibles à ventiler.
Morceaux choisis
1. On considère qu’un médecin exerçant en SMUR intube annuellement de 15 à 20 patients. Ces chiffres sont à mettre en parallèle avec les données disponibles pour l’activité anesthésique nationale où environ trois millions de patients sont intubés tous les ans au bloc opératoire par des médecins anesthésistes qui intubent chacun en moyenne plus de 300 patients par an.
Un minimum de 40 intubations pour apprendre l'intubation est nécessaire et 20 par an sont nécessaires pour entretenir cette compétence. Cela signifie que la maîtrise de l'abord des VAS est l'objectif principal de la formation continue du médecin d'unité de telle sorte qu'il soit toujours en capacité de faire face à une obstruction des VAS en condition de combat.
2. Les dispositifs laryngés sont probablement plus faciles à insérer pour des opérateurs non médecins que la sonde d’intubation. Les deux problèmes majeurs rencontrés lors de l’utilisation de ce type de matériel sont le risque d’inhalation pulmonaire et le risque de perforation œsophagienne. En effet, ces dispositifs n’assurent pas une protection complète des voies aériennes en cas de vomissement et le risque d’inhalation est alors réel. Plusieurs cas de déchirure du tiers supérieur de l’œsophage ont été rapportés lors de l’utilisation du Combitube®, liés à la surpression régnant dans le ballonnet œsophagien de ce dispositif.
3. En médecine préhospitalière, les circonstances font que très souvent les patients qui nécessitent une intubation en urgence sont pris en charge alors qu’ils sont allongés sur le sol. L’intubation d’un patient au sol présente quelques difficultés particulières. L’opérateur est en effet dans une position le plus souvent pénible pour réaliser son geste et l’intubation est rendue plus difficile. Une technique de positionnement de l’opérateur visant à limiter les difficultés d’intubation a été décrite récemment. Elle consiste à positionner la personne qui va intuber en décubitus latéral. Dans cette position, l’axe visuel de l’opérateur est abaissé et la visualisation glottique, indispensable pour réaliser l’intubation, est rendue beaucoup plus aisée.
4. Parmi les dispositifs laryngés utilisables en préhospitalier, il faut choisir le FASTRACH car son emploi est documenté et qu'il permet l'intubation orotrachéale.
5. La cricothyroïdotomie représente la technique ultime de contrôle des voies aériennes proposée dans le cas où l’intubation et la ventilation du patient restent impossibles malgré l’utilisation des autres techniques alternatives que sont les mandrins et les dispositifs supraglottiques. ......Cette technique est de réalisation très rapide et permet une ventilation efficace dans plus de 95 % des cas.
6. Un algorithme
| Tags : intubation, airway, coniotomie
19/11/2010
Masque laryngé: Êtes vous sûr ?
La place des dispositifs laryngés pour le contrôle des voies aériennes en condition de combat est très limitée. Ces dispositifs ne font pas partie des mesures recommandées par le TCCC et le BATLS, car ils ne ne répondent pas aux critères essentiels qui sont d'assurer l'ouverture des voies aériennes en cas de plaie maxillo-faciale, ils ne protègent pas des risques d'inhalation, ils ne dispensent pas de la réalisation d'une sédation, ils sont susceptibles de mobilisation, enfin ils ne représente pas la première ligne de traitement pour la prise en charge d'une détresse respiratoire en condition de combat.
L'article suivant expose un certain nombre de désagrément lié à l'emploi de l'un de ces dispositifs.
Indian Journal of Anaesthesia 2009; 53 (4):414-424
Troubleshooting ProSeal LMA
Bimla Sharma, Jayashree Sood , Chand Sahai , V P Kumra
Summary
Supraglottic devices have changed the face of the airway management. These devices have contributed in a bigway in airway management especially, in the difficult airway scenario significantly decreasing the pharyngolaryngeal morbidity. There is a plethora of these devices, which has been well matched by their wider acceptance in clinical practice. ProSeal laryngeal mask airway (PLMA) is one such frequently used device employed for spontaneous as well as controlled ventilation. However, the use of PLMA at times may be associated with certain problems. Some of the problems related with its use are unique while others are akin to the classic laryngeal mask airway (cLMA). However, expertise is needed for its safe and judicious use, correct placement, recognition and management of its various malpositions and complications. The present article describes the tests employed for proper confirmation of placement to assess the ventilatory and the drain tube functions of the mask, diagnosis of various malpositions and the management of these aspects. All these areas have been highlighted under the heading of troubleshooting PLMA. Many problems can be solved by proper patient and procedure selection, maintaining adequate depth of anaesthesia, diagnosis and management of malpositions. Proper fixation of the device and monitoring cuff pressure intraoperatively may bring down the incidence of airway morbidity.
26/10/2010
Coniotomie: Connaître l'anatomie aide
Une publication récente résume de manière simple ce qu'il faut savoir, et tout cela en anglais bien sûr.
| Tags : airway, coniotomie
16/10/2010
Alternative à l'intubation; La coniotomie chirurgicale
Il existe un grand débat concernant les alternatives à l'intubation préhospitalière. Si les dispositifs laryngés apparaissent une alternative du fait de taux d'insertion satisfaisant en particulier le tube KING LT, il n'en demeure toujours pas moins qu'il ne représente toujours pas une solution réelle en conditions de combat du fait de la nécessité de réaliser une anesthésie générale, de l'absence de protection contre le risque d'inhalation, et de limitations importantes en terme de ventilation (pression et déplacement de tube pendant le transport). Ces dispositifs sont par ailleurs relativement volumineux. La recommandation en condition de combat est de privilégier la coniotomie chirurgicale sous AL.
-------------------------------------------------------------------
Prehosp Emerg Care. 2010 Oct-Dec;14(4):515-30.
A meta-analysis of prehospital airway control techniques part II: alternative airway devices and cricothyrotomy success rates.
Hubble MW, Wilfong DA, Brown LH, Hertelendy A, Benner RW.
Emergency Medical Care Program, 122 Moore Building, Western Carolina University, Cullowhee, NC 28723, USA. mhubble@email.wcu.edu
Abstract
BACKGROUND: Airway management is a key component of prehospital care for seriously ill and injured patients. Oral endotracheal intubation (OETI) is the definitive airway of choice in most emergency medical services (EMS) systems. However, OETI may not be an approved skill for some clinicians or may prove problematic in certain patients because of anatomic abnormalities, trauma, or inadequate relaxation. In these situations alternative airways are frequently employed. However, the reported success rates for these devices vary widely, and established benchmarks are lacking.
OBJECTIVE: We sought to determine pooled estimates of the success rates of alternative airway devices (AADs) and needle cricothyrotomy (NCRIC) and surgical cricothyrotomy (SCRIC) placement through a meta-analysis of the literature.
METHODS: We performed a systematic literature search for all English-language articles reporting success rates for AADs, SCRIC, and NCRIC. Studies of field procedures performed by prehospital personnel from any nation were included. All titles were reviewed independently by two authors using prespecified inclusion criteria. Pooled estimates of success rates for each airway technique were calculated using a random-effects meta-analysis model.
RESULTS: Of 2,005 prehospital airway titles identified, 35 unique studies were retained for analysis of AAD success rates, encompassing a total of 10,172 prehospital patients. The success rates for SCRIC and NCRIC were analyzed across an additional 21 studies totaling 512 patients. The pooled estimates (and 95% confidence intervals [CIs]) for intervention success across all clinicians and patients were as follows: esophageal obturator airway-esophageal gastric tube airway (EOA-EGTA) 92.6% (90.1%-94.5%); pharyngeotracheal lumen airway (PTLA) 82.1% (74.0%-88.0%); esophageal-tracheal Combitube (ETC) 85.4% (77.3%-91.0%); laryngeal mask airway (LMA) 87.4% (79.0%-92.8%); King Laryngeal Tube airway (King LT) 96.5% (71.2%-99.7%); NCRIC 65.8% (42.3%-83.59%); and SCRIC 90.5% (84.8%-94.2%).
CONCLUSIONS: We provide pooled estimates for prehospital AAD, NCRIC, and SCRIC airway interventions. Of the AADs, the King LT demonstrated the highest insertion success rate (96.5%), although this estimate is based on limited data, and data regarding its ventilatory effectiveness are lacking; more data are available for the ETC and LMA. The ETC, LMA, and PTLA all had similar-but lower-success rates (82.1%-87.4%). NCRIC has a low rate of success (65.8%); SCRIC has a much higher success rate (90.5%) and should be considered the preferred percutaneous rescue airway.
-------------------------------------------------------------------
| Tags : airway
11/10/2010
Coniotomie: Avec un guide !
La coniotmie ou cricothyrotomie est unetechnique essentielle à maîtriser pour une prise en charge optimale des blessés de la face présentant une obstruction des voies aériennes ( le A du SAFE ABC MARCHE). ICI vous est présenté une technique qu'il faut connaître.
| Tags : airway, coniotomie
07/10/2010
Coniotomie: Chirurgie vs percutané ?
Volume 8, Issue 4, October-December 2004, Pages 424-426
Michelle Fischer Keane MD ,
,  , Kathryn H. Brinsfield MD, K. Sophia Dyer MD, Simon Roy MD and Daniel White EMT-P
, Kathryn H. Brinsfield MD, K. Sophia Dyer MD, Simon Roy MD and Daniel White EMT-P
Abstract
Objective
To compare the speeds and success rates of placement for percutaneous cricothyrotomy versus surgical or open cricothyrotomy.
Methods
Twenty-two paramedics (mean 9.7 years of experience), with training in both methods, were timed using a pig trachea in a crossover model. An emergency physician performed timing and documentation of success; timing commenced after the equipment was ready and the membrane was identified. Paramedics were randomly assigned by a coin toss to start in either group. All were actively employed by a municipal third-service emergency medical services (EMS) agency. Paramedics who did not complete one of the methods correctly were excluded from speed analysis. Data were analyzed using descriptive statistics, a t-test of paired samples, and confidence intervals for matched samples.
Results
Placement of a surgical cricothyrotomy was significantly faster (mean 28 seconds, range 10–78 seconds) than the percutaneous method (mean 123 seconds, range 58–257 seconds) (p < 0.001). Mean difference between the 20 matched percutaneous versus surgical pairs was 93.75 seconds (95% CI 72.3, 115.2). The surgical route had a 100% success rate at obtaining airway control, whereas the percutaneous method had a 90.9% success rate (p = 0.1).
Conclusion
In an animal model, surgical cricothyrotomy appeared to be a preferable method for establishing a definitive airway over the percutaneous method. Further research is required to define the optimal approach in the prehospital setting for the invasive airway.
07/12/2008
Au sujet de la coniotomie
| Tags : respiration