25/10/2016
Coniotomie chirurgicale: Spécialiste ? Non, mais formé spécifiquement OUI
The success of battlefield surgical airway insertion in severely injured military patients: a UK perspective.
BACKGROUND:
The insertion of a surgical airway in the presence of severe airway compromise is an uncommon occurrence in everyday civilian practice. In conflict, the requirement for insertion of a surgical airway is more common. Recent military operations in Afghanistan resulted in large numbers of severely injured patients, and a significant proportion required definitive airway management through the insertion of a surgical airway.
OBJECTIVE:
To examine the procedural success and survival rate to discharge from a military hospital over an 8-year period.
METHODS:
A retrospective database and chart review was conducted, using the UK Joint Theatre Trauma Registry and the Central Health Records Library. Patients who underwent surgical airway insertion by UK medical personnel from 2006 to 2014 were included. Procedural success, demographics, Injury Severity Score, practitioner experience and patient survival data were collected. Descriptive statistics were used for data comparison, and statistical significance was defined as p<0.05.
RESULTS:
86 patients met the inclusion criterion and were included in the final analysis. The mean patient age was 25 years, (SD 5), with a median ISS of 62.5 (IQR 42). 79 (92%) of all surgical airways were successfully inserted. 7 (8%) were either inserted incorrectly or failed to perform adequately. 80 (93%) of these procedures were performed either by combat medical technicians or General Duties Medical Officers (GDMOs) at the point of wounding or Role 1. 6 (7%) were performed by the Medical Emergency Response Team. 21 (24%) patients survived to hospital discharge.
DISCUSSION:
Surgical airways can be successfully performed in the most hostile of environments with high success rates by combat medical technicians and GDMOs. These results compare favourably with US military data published from the same conflict.
| Tags : airway, coniotomie
05/10/2016
Conio: Apprendre 1 h, mieux que rien mais pas assez
Self-directed simulation-based training of emergency cricothyroidotomy: a route to lifesaving skills.
| Tags : airway
04/10/2016
Conio: Et encore pour la technique chirurgicale
Surgicric 2: A comparative bench study with two established emergency cricothyroidotomy techniques in a porcine model.
BACKGROUND:
'Can't Intubate, Can't Oxygenate' is a rare but life threatening event. Anaesthetists must be trained and have appropriate equipment available for this. The ideal equipment is a topic of ongoing debate. To date cricothyroidotomy training for anaesthetists has concentrated on cannula techniques. However cases reported to the NAP4 audit illustrated that they were associated with a high failure rate. A recent editorial by Kristensen and colleagues suggested all anaesthetists must master a surgical technique. The surgical technique for cricothyroidotomy has been endorsed as the primary technique by the recent Difficult Airway Society 2015 guidelines.
METHODS:
We conducted a bench study comparing the updated Surgicric 2 device with a scalpel-bougie-tube surgical technique, and the Melker seldinger technique, using a porcine model. Twenty six senior anaesthetists (ST5+) participated. The primary outcome was insertion time. Secondary outcomes included success rate, ease of use, device preference and tracheal trauma.
RESULTS:
There was a significant difference (P<0.001) in the overall comparisons of the insertion times. The surgical technique had the fastest median time of 62 s. The surgical and Surgicric techniques were significantly faster to perform than the Melker (both P<0.001). The surgical technique had a success rate of 85% at first attempt, and 100% within two attempts, whereas the others had failed attempts. The surgical technique was ranked first by 50% participants and had the lowest grade of posterior tracheal wall trauma, significantly less than the Surgicric 2 (P=0.002).
CONCLUSIONS:
This study supports training in and the use of surgical cricothyroidotomy by anaesthetists.
| Tags : airway
24/09/2016
Crico: Mais que fait-on ?
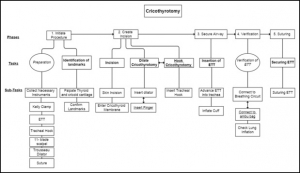
A hierarchical task analysis of cricothyroidotomy procedure for a virtual airway skills trainer simulator
Demirel D. et Al. Am J Surg. 2016 Sep;212(3):475-84
BACKGROUND:
Despite the critical importance of cricothyroidotomy (CCT) for patient in extremis, clinical experience with CCT is infrequent, and current training tools are inadequate. The long-term goal is to develop a virtual airway skills trainer that requires a thorough task analysis to determine the critical procedural steps, learning metrics, and parameters for assessment.
METHODS:
Hierarchical task analysis is performed to describe major tasks and subtasks for CCT. A rubric for performance scoring for each taskwas derived, and possible operative errors were identified.
RESULTS:
Time series analyses for 7 CCT videos were performed with 3 different observers. According to Pearson's correlation tests, 3 of the 7 major tasks had a strong correlation between their task times and performance scores.
CONCLUSIONS:
The task analysis forms the core of a proposed virtual CCT simulator, and highlights links between performance time and accuracy when teaching individual surgical steps of the procedure.
| Tags : airway
22/09/2016
Crico: Quelques rappels qui font du bien
Evidence Is Important: Safety Considerations for Emergency Catheter Cricothyroidotomy
Marshall SD et Al. Acad Emerg Med. 2016 Sep;23(9):1074-6
Il existe un regain d'intérêt concernant la pratique de l'oxygénation après ponction de la membrane cricoÏdienne. De large débats portent sur la meilleure méthode à utiliser. En pratique il n'est pas inutile de rappeler quelques vérités pratiques. C'est ce que propose ce document dont la lecture est fort utile. Cliquez sur la référence pour accéder au document et ici pour accéder à des vidéos complémentaires
| Tags : coniotomie
07/09/2016
Airway: S'y pencher avec sérieux
Emergency airway management – by whom and how ?
Sollid SJ et Al. Acta Anaesthesiol Scand. 2016 Oct;60(9):1185-7
---------------------------------------
Encore une publication qui insiste sur la formation à la gestion des voies aériennes et au maintien de ses compétences. Ceci n'est pas innée et s'impose tout d'abord non seulement aux praticiens peu confrontés à cette exercice, en première ligne les médecins urgentistes, mais aussi aux médecins anesthésistes compte tenu de l'essor de l'anesthésie loco-régionale et l'emploi de dispositifs supra-glottique. A lire et relire, ainsi que les références.
---------------------------------------
Procedures for advanced airway management are important for maintaining basic life functions in the unconscious patient, and can be lifesaving in critically ill or injured patients. In Acta Anaesthesiologica Scandinavica, a working group from the Scandinavian Society of Anaesthesiology and Intensive Care Medicine (SSAI) presents updated clinical guidelines on pre-hospital airway management.[1] The recommendations from the working group are important statements in the long-lasting quest to ensure that advanced airway management is managed safely pre-hospital at the right level of competence.
Technically, many of the procedures for advanced airway management of the average patient in controlled situations are easy to learn. Yet, a German study found that at least 200 intubation attempts were required to reach a 95% success rate.[2] The challenge, however, lies in assessing and managing the difficult airway cases. Emergency physicians with anaesthesiology background seem to be better at predicting difficult intubations than emergency physicians with other backgrounds, in addition to having significantly lower incidence of intubation problems and more experience in decisions on whether to intubate.[3]
Data from the UK show that the majority of complications in airway management occur in the emergency department and the intensive care unit. One of the reasons is the relatively low exposure to such procedures in these settings.[4] Studies on pre-hospital airway management also indicate that the rate of complications in this setting is high, and also that it is greatly dependent on the competence of the provider.[5] There is sufficient evidence to support that pre-hospital advanced airway management in the hands of trained anaesthesiologists is a safe procedure.[6-8] However, as other authors have pointed out, being a proficient provider of airway management is not equivalent with being an anaesthesiologist.[9] The combination of competencies to assess the situation, practical skills and ability to manage complications are more important than the name of the provider's speciality. In a physician-staffed helicopter emergency medical service in the UK, where doctors are a mix of anaesthesiologists and emergency physicians, the success rates are still high and complications are low.[10] This is probably related to the strict training and highly standardised operating procedures that all doctors must adhere to.
Based on this, advanced airway management seems to be safe if the providers have a large volume of clinical experience (anaesthesiologists) or alternatively, operate under strict clinical guidance and protocol rule (non-anaesthesiologists). Intuitively, a combination of both could probably improve safety further and would be useful in clinical environments, and particularly when airway management occurs as unplanned events with little or no time for individual planning and screening of the patient.
The most recent consensus-based European Guidelines for Postgraduate Training in Anaesthesiology recommend the change from duration of training and number of procedures into competence-based training.[11] These competences include advanced airway management skills. Some of this training can be done in simulation settings, but simulation cannot replace real-life situations.[12, 13] Once learnt, competences must be maintained. That requires regular exposure to the procedure. As the use of laryngeal masks and regional blocks increases at the expense of anaesthesia procedures including endotracheal intubation, the training opportunities for all providers, including anaesthesia personnel is being reduced. That is one of the reasons why the Section and Board of Anaesthesiology of the European Union of Medical Specialists recommended a multispecialty approach to emergency medicine.[14] Like the Scandinavian Society of Anaesthesiology and Intensive Care recommended in 2010,[15] the European Society of Anaesthesiology is increasingly using the term ‘Critical Emergency Medicine’ for the part of the anaesthesiology speciality that all anaesthesiologists should command.
A Nordic working group published a literature review in 2008 on pre-hospital airway management, and proposed an evidence-based guideline.[16] This position paper concludes unanimously that pre-hospital emergency airway management in the appropriate patient groups should be achieved by rapid sequence induction and endotracheal intubation, provided the physician is an anaesthesiologist. Other providers should treat the same patient group in the lateral trauma recovery position and if necessary, provide assisted bag-valve-mask ventilation. Supraglottic airway devices were recommended for non-anaesthesiologists in cardiac arrest with a need for supine positioning of the patient, and as a backup device for anaesthesiologists. These findings have been reaffirmed in the new SSAI clinical practice guideline published in August issue.[1]
A similar paper concerning Scandinavian clinical practice guidelines on general anaesthesia for emergency situations underlines the dangers associated with administering anaesthesia outside the operating theatre. They too advocate that anaesthesia for emergency patients should be given by, or under very close supervision by, experienced anaesthesiologists, and stress that problems with the airway are to be anticipated.[17]
Emergency airway management outside the operating theatres carries a high risk of difficult intubation, in a recent study 10.3%, and these patients have a high risk of complications.[18] This demonstrate the need for particular vigilance in and training for these settings, and provides another argument for using supraglottic approaches for those patients in the hands of non-anaesthesiologists. A recent report from the Johns Hopkins Hospital describes a successful attempt to mitigate difficult airway situations arising within this highly specialised hospital. By the formation of a difficult airway response team, the researchers conquered difficult airway situations which until the intervention ranked among the top five adverse events in Maryland.[19]
In conclusion, emergency airway management carries a high risk of patient injury, even among highly trained and skilled anaesthesiologists. Airway management can be learned, and emergency airway handling can be performed with maintained safety also by non-anaesthesiologists, provided they operate in a highly supervised and algorithm-based environment.[9] In this light, the emerging new emergency medical specialty in the Scandinavian countries is of concern, if these acute or emergency physicians are supposed to perform emergency airway procedures independent of their anaesthesiologist colleagues. Whoever manages the compromised airway in the pre-hospital setting is required to do so with the highest level of quality, attainable through a combination of clinical experience and clinical governance. It is difficult to see how this can be achieved and maintained outside the specialty of anaesthesiology. In the end, this is a matter of patient safety, not competition for airways.
| Tags : airway
01/09/2016
Pensez, efficace et peu couteux
Cognitive skills analysis, kinesiology, and mental imagery in the acquisition of surgical skills
Bathalon S. et Al. J Otolaryngol. 2005 Oct;34(5):328-32.
--------------------------------------------
Un moyen simple pour améliorer sa performance
--------------------------------------------
GOAL:
Isolate and evaluate the impact of mental imagery on the acquisition of an emergency surgical technique.
METHOD:
We studied 44 first-year medical students performing a cricothyrotomy on a mannequin to determine the impact of teaching usingmental imagery (MI) and/or kinesiology (KG) compared to the standard Advandec Trauma Life Support (ATLS) approach. Students were randomly assigned to one of three groups: MI and KG, KG alone or control (ATLS). Two weeks after the one-hour teaching session, they were evaluated with an OSCE testing the performance of the different steps of the technique, the time required and its fluidity.
RESULTS:
Total results (maximum: 25 marks) are as follows: KG + MI = 20.3 +/- 1.5 ; KG = 19.3 +/- 2.9 ; ATLS = 18.2 +/- 2.5. The only statistically significant difference for total results was in the use of MI and KG compared to the control group. Kinesiology alone or with mental imageryimproved the fluidity of the performance.
CONCLUSION:
Many factors influence the acquisition of a surgical technique. This study showed that acquisition and performance of an emergency procedure (cricothyrotomy) was improved when mental imagery and kinesiology were combined to teach it.
31/08/2016
Echo et voies aériennes: Mais oui, à maîtriser
The Role of Airway and Endobronchial Ultrasound in Perioperative Medicine
Vortrua J et Al. Biomed Res Int. 2015; 2015: 754626
-------------------------------
Certainement UN APPORT IMPORTANT à la gestion des voies aériennes et de la ventilation non seulement dans les blocs opératoires mais dans les situations critiques y compris hors de l'hôpital.
-------------------------------
Recent years have witnessed an increased use of ultrasound in evaluation of the airway and the lower parts of the respiratory system. Ultrasound examination is fast and reliable and can be performed at the bedside and does not carry the risk of exposure to ionizing radiation. Apart from use in diagnostics it may also provide safe guidance for invasive and semi-invasive procedures. Ultrasound examination of the oral cavity structures, epiglottis, vocal cords, and subglottic space may help in the prediction of difficult intubation. Preoperative ultrasound may diagnose vocal cord palsy or deviation or stenosis of the trachea. Ultrasonography can also be used for confirmation of endotracheal tube, double-lumen tube, or laryngeal mask placement. This can be achieved by direct examination of the tube inside the trachea or by indirect methods evaluating lung movements. Postoperative airway ultrasound may reveal laryngeal pathology or subglottic oedema. Conventional ultrasound is a reliable real-time navigational tool for emergency cricothyrotomy or percutaneous dilational tracheostomy. Endobronchial ultrasound is a combination of bronchoscopy and ultrasonography and is used for preoperative examination of lung cancer and solitary pulmonary nodules. The method is also useful for real-time navigated biopsies of such pathological structures.
| Tags : airway
Crico avec un stylo ? NON
Bystander cricothyrotomy with ballpoint pen: a fresh cadaveric feasibility study
Kisser U. et Al. Emerg Med J. 2016 Aug;33(8):553-6.
OBJECTIVE:
In motion pictures and anecdotal reports, ballpoint pens have been used for life-saving cricothyroidotomies. The objective of this study was to examine the widespread belief that ballpoint pens can perforate the skin and cricothyroid ligament and could be used as substitute tracheostomy sets in an emergency setting.
METHODS:
Three different ballpoint pens were examined regarding their inner diameter, their demountability to form a cannula and their airflow properties. Ten medical laypersons were asked to try to puncture the trachea through the skin and the cricothyroid ligament in 10 fresh cadavers just using the ballpoint pens.
RESULTS:
Two of three pens had inner diameters of >3 mm and were both suitable as cannulas in a tracheotomy. All participants could perforate the skin with both ballpoint pens. However, almost no one could penetrate through the cricothyroid ligament or the ventral wall of the trachea, except for one participant. He performed the tracheostomy after three attempts in >5 min with a lot of patience and force.
CONCLUSIONS:
A cricothyroidotomy just with a ballpoint pen is virtually impossible. First, the airflow resistance in commercially available ballpoint pens is too high to produce effective ventilation. Second, the cricothyroid ligament is too strong to be penetrated by ballpoint pens.
| Tags : airway
30/08/2016
Crico et Echo: Pensez TACA
Ultrasonographic identification of the cricothyroid membrane: best evidence, techniques, and clinical impact
Kristensen MS et Al. Br. J. Anaesth. (2016) 117 (suppl 1):i39-i48
Inability to identify the cricothyroid membrane by inspection and palpation contributes substantially to the high failure rate of cricothyrotomy. This narrative review summarizes the current evidence for application of airway ultrasonography for identification of the cricothyroid membrane compared with the clinical techniques. We identified the best-documented techniques for bedside use, their success rates, and the necessary training for airway-ultrasound-naïve clinicians.

After a short but structured training, the cricothyroid membrane can be identified using ultrasound in difficult patients by previously airway-ultrasound naïve anaesthetists with double the success rate of palpation. Based on the literature, we recommend identifying the cricothyroid membrane before induction of anaesthesia in all patients. Although inspection and palpation may suffice in most patients, the remaining patients will need ultrasonographic identification; a service that we should aim at making available in all locations where anaesthesia is undertaken and where patients with difficult airways could be encountered.
| Tags : airway
Crico: Maintenir son savoir, pas gagné !
Out-of-Hospital Surgical Airway Management: Does Scope of Practice Equal Actual Practice?
Furin M. et Al. West J Emerg Med. 2016 May;17(3):372-6
------------------------------
La coniotomie est un geste dont la réalisation est rare. Il existe actuellement un regain d'intérêt pour la maîtrise de cette pratique. Encore faut il avoir la démarche d'entretenir ses pratiques. On part de loin, c'est ce que met en valeur ce travail.
------------------------------
INTRODUCTION:
Pennsylvania, among other states, includes surgical airway management, or cricothyrotomy, within the paramedic scope of practice. However, there is scant literature that evaluates paramedic perception of clinical competency in cricothyrotomy. The goal of this project is to assess clinical exposure, education and self-perceived competency of ground paramedics in cricothyrotomy.
METHODS:
Eighty-six paramedics employed by four ground emergency medical services agencies completed a 22-question written survey that assessed surgical airway attempts, training, skills verification, and perceptions about procedural competency. Descriptive statistics were used to evaluate responses.
RESULTS:
Only 20% (17/86, 95% CI [11-28%]) of paramedics had attempted cricothyrotomy, most (13/17 or 76%, 95% CI [53-90%]) of whom had greater than 10 years experience. Most subjects (63/86 or 73%, 95% CI [64-82%]) did not reply that they are well-trained to perform cricothyrotomy and less than half (34/86 or 40%, 95% CI [30-50%]) felt they could correctly perform cricothyrotomy on their first attempt. Among subjects with five or more years of experience, 39/70 (56%, 95% CI [44-68%]) reported 0-1 hours per year of practical cricothyrotomy training within the last five years.

How much and what type of training have you had in prehospital cricothyrotomy in the past 1 year and the past 5 years?
Half of the subjects who were able to recall (40/80, 50% 95% CI [39-61%]) reported having proficiency verification for cricothyrotomy within the past five years.
CONCLUSION:
Paramedics surveyed indicated that cricothyrotomy is rarely performed, even among those with years of experience. Many paramedics felt that their training in this area is inadequate and did not feel confident to perform the procedure. Further study to determine whether to modify paramedic scope of practice and/or to develop improved educational and testing methods is warranted.
| Tags : airway
29/08/2016
Anatomie cricoïdienne
Topographical anatomy of cricothyroid membrane and its relation with invasive airway access.
Develi S. et Al. Clin Anat. 2016 Aug 2. doi: 10.1002/ca.22750
-----------------------------
On enseigne que l'abord cricothyroïdien est sécuritaire, notamment concernnant le risuqe de ponctions vasculaires. Cela est vrai surtout pour sa partie inférieure et tout partiuclièrement son quadran inférieur droit.
-----------------------------
Cricothyroidotomy is a surgical procedure involving penetration through the skin and cricothyroid membrane to maintain airway patency during life-threatening emergency conditions. Complications such as bleeding and laryngeal stenosis can result from it. Our aim in this study was to identify the anatomical structures located on the membrane and to ascertain whether there is a safe area on the membrane for this procedure. Thirty larynx specimens fixed with 10% formaldehyde in the Department of Anatomy were dissected. The cricothyroid artery, the cricothyroid vein, the common artery and vein formed by the cricothyroid vessels, the pyramidal lobe of the thyroid gland and lymph nodes were observed on the membrane. The cricothyroid membrane was divided into four quadrants and the most common locations of these anatomical structures on the membrane were recorded.
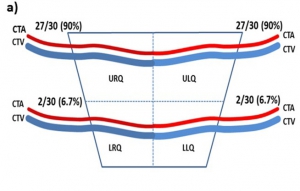
The cricothyroid artery and vein were located on the upper half of the membrane, the common vein was found in the midline, coursing to the thyroid gland, and the lobus pyramidalis and lymph nodes were located on the left side of the midline. Overall, the anatomical structures were mostly located on the upper half and lower left quadrant of the cricothyroid membrane. Thus, the lower right quadrant seems safer for invasive procedures such as needle cricothyroidotomy or other cannulation techniques. Needle puncture or cannulation through the lower right quadrant of the cricothyroid membrane will injure fewer anatomical structures so there should be fewer complications due to degradation of the vascular supply to this region
Echographie: Un outil pour la gestion des VAS
Role of upper airway ultrasound in airway management
Osman A. et Al. Osman and Sum Journal of Intensive Care (2016) 4:52
Upper airway ultrasound is a valuable, non-invasive, simple, and portable point of care ultrasound (POCUS) for evaluation of airway management even in anatomy distorted by pathology or trauma. Ultrasound enables us to identify important sonoanatomy of the upper airway such as thyroid cartilage, epiglottis, cricoid cartilage, cricothyroid membrane, tracheal cartilages, and esophagus. Understanding this applied sonoanatomy facilitates clinician to use ultrasound in assessment of airway anatomy for difficult intubation, ETT and LMA placement and depth, assessment of airway size, ultrasound-guided invasive procedures such as percutaneous needle cricothyroidotomy and tracheostomy, prediction of postextubation stridor and left double-lumen bronchial tube size, and detecting upper airway pathologies. Widespread POCUS awareness, better technological advancements, portability, and availability of ultrasound in most critical areas facilitate upper airway ultrasound to become the potential first-line non-invasive airway assessment tool in the future.
| Tags : intubation
23/07/2016
Moins d'expérience ? Alors la conio chirurgicale
Emergency Cricothyrotomy Performed by Surgical Airway–naive Medical Personnel
Heymans F. et Al. Anesthesiology 2016; 125:295-303
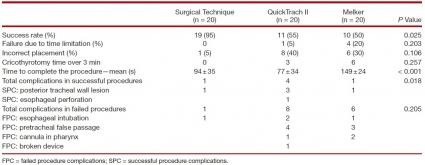
BACKGROUND:
When conventional approaches to obtain effective ventilation and return of effective spontaneous breathing fail, surgical airway is the last rescue option. Most physicians have a limited lifetime experience with cricothyrotomy, and it is unclear what method should be taught for this lifesaving procedure. The aim of this study is to compare the performance of medical personnel, naive to surgical airway techniques, in establishing an emergency surgical airway in cadavers using three commonly used cricothyrotomy techniques.
METHODS:
Twenty medical students, without previous knowledge of surgical airway techniques, were randomly selected from their class. After training, they performed cricothyrotomy by three techniques (surgical, Melker, and QuickTrach II) in a random order on 60 cadavers with comparable biometrics. The time to complete the procedure, rate of success, and number of complications were recorded. A success was defined as the correct placement of the cannula within the trachea in 3 min.
RESULTS:
The success rates were 95, 55, and 50% for surgical cricothyrotomy, QuickTrach, and Melker, respectively (P = 0.025). The majority of failures were due to cannula misplacement (15 of 20). In successful procedures, the mean procedure time was 94 ± 35 s in the surgical group, 77 ± 34 in the QuickTrach II group, and 149 ± 24 in the Melker group (P < 0.001). Few significant complications were found in successful procedures. No cadaver biometric parameters were correlated with success of the procedure.
| Surgical Technique | QuickTrach II | Melker | ||
| Success rate (%)) ) | 19 (95 | 11 (55) | 10 (50 | 0.025 |
| Failure due to time limitation (%) | 0 | 1 (5) | 4 (20) | 0.203 |
| Incorrect placement (%) | 1 (5) | 8 (40) ) | 6 (30) | 0.106 |
| Cricothyrotomy time over 3 min | 0 | 3 | 6 | 0.257 |
| Time to complete the procedure—mean (s) | 94±35 | 149±24 | < 0.001 | |
| Total complications in successful procedures | 1 | 4 | 1 | 0.018 |
| SPC: posterior tracheal wall lesion | 1 | 3 | 1 | |
| SPC: esophageal perforation 1 | 10 (50 | |||
| Total complications in failed procedures | 1 | 8 | 6 | 0.205 |
| FPC: esophageal intubation | 1 | 2 | 1 | |
| FPC: pretracheal false passage | 4 | 3 | ||
| FPC: cannula in pharynx 1 2 | 1 | 2 | ||
| FPC: broken device 1 | 1 | |||
| FPC = failed procedure complications; SPC = successful procedure complications. |
"....In conclusion, our results indicate that medical personnel naive to surgical airway techniques establish a surgical airway more efficiently using surgical cricothyroidotomy. Since the vast majority of clinicians perform emergency airway infrequently, our observation might apply to the majority of them. Whether surgical cricothyrotomy remains superior in advance-trained medical personnel requires further study......"
CONCLUSION:
Surgical airway-naive medical personnel establish emergency cricothyrotomy more efficiently and safely with the surgical procedure than with the other two commonly used techniques.
| Tags : airway
08/07/2016
Coniotomie: Plaidoyer UK pour la chirurgie
The success of battlefield surgical airway insertion in severely injured military patients: a UK perspective
Tyle T et Al. J R Army Med Corps. 2016 Jun 6. pii: jramc-2016-000637. doi: 10.1136/jramc-2016-000637
-----------------------------------------------
Un geste peu fréquent: 86 blessés sur une période de 8 ans et pourtant un geste essentiel à maîtriser. Faire simple est mieux. Pour cela pas besoin d'être chirurgien, urgentiste ou anesthésiste-réanimateur.
-----------------------------------------------
BACKGROUND:
The insertion of a surgical airway in the presence of severe airway compromise is an uncommon occurrence in everyday civilian practice. In conflict, the requirement for insertion of a surgical airway is more common. Recent military operations in Afghanistan resulted in large numbers of severely injured patients, and a significant proportion required definitive airway management through the insertion of a surgical airway.
OBJECTIVE:
To examine the procedural success and survival rate to discharge from a military hospital over an 8-year period.
METHODS:
A retrospective database and chart review was conducted, using the UK Joint Theatre Trauma Registry and the Central Health Records Library. Patients who underwent surgical airway insertion by UK medical personnel from 2006 to 2014 were included. Procedural success, demographics, Injury Severity Score, practitioner experience and patient survival data were collected. Descriptive statistics were used for data comparison, and statistical significance was defined as p<0.05.
RESULTS:
86 patients met the inclusion criterion and were included in the final analysis. The mean patient age was 25 years, (SD 5), with a median ISS of 62.5 (IQR 42). 79 (92%) of all surgical airways were successfully inserted. 7 (8%) were either inserted incorrectly or failed to perform adequately. 80 (93%) of these procedures were performed either by combat medical technicians or General Duties Medical Officers (GDMOs) at the point of wounding or Role 1. 6 (7%) were performed by the Medical Emergency Response Team. 21 (24%) patients survived to hospital discharge.
DISCUSSION:
Surgical airways can be successfully performed in the most hostile of environments with high success rates by combat medical technicians and GDMOs. These results compare favourably with US military data published from the same conflict.
| Tags : airway, coniotomie
28/06/2016
Crico: Incisez et palpez sous la peau !
Deficiencies in locating the cricothyroid membrane by palpation: We can’t and the surgeons can’t, so what now for the emergency surgical airway ?
Law JA et Al. Can J Anesth (2016) 63:791–796
"......Certaines questions concernant la localisation de la membrane cricothyroïdienne demeurent sans réponse. Nous savons désormais que la palpation externe manque de précision, indépendamment de la spécialité du médecin évaluateur. En d’autres termes, les techniques qui s’appuient sur un accès direct à la trachée via la membrane cricothyroïdienne palpée depuis l’extérieur (par ex., les techniques percutanées de Seldinger ou réalisées à l’aide d’un trocart, un accès basé sur un scalpel à l’aide d’une coupure horizontale unique) courent toutes le risque d’un mauvais positionnement. L’alternative, lorsqu’on a recours à ces techniques de cricothyrotomie (en fait, à toutes ces techniques), est de commencer par une incision verticale médiane de 3-4 cm à travers la peau et les tissus sous-cutanés situés sur l’emplacement estimé de la membrane cricothyroïdienne.5,6 La membrane cricothyroïdienne est ensuite palpée à nouveau dans la lésion, et son emplacement devrait être bien plus facile à déterminer lorsqu’il y a considérablement moins de tissu mou entre le doigt qui palpe et la membrane cricothyroïdienne. La cricothyrotomie peut ensuite se faire à l’aide de la technique choisie et en étant absolument certain de son bon positionnement......"
| Tags : airway, coniotomie
27/06/2016
Crico: Utilisez le manche du bistouri !
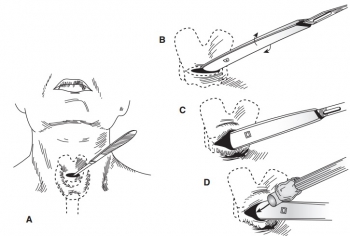
Surgical Procedures in Trauma Management. New York, NY: Thieme Inc; 1986:303
| Tags : airway, coniotomie
15/06/2016
Coniotomie: Chirurgicale SVP !
Emergency Cricothyrotomy Performed by Surgical Airway–naive Medical Personnel
Heymans F. et Al. Anesthesiology 2016; 125:00-00
----------------------------------------
L'obstruction des voies aériennes est une cause rare mais évitable de décès au combat. savoir ouvrir un cou est donc un geste qui doit être maîtrisé par le médecin ou l'infirmier présent. Se pose cependant la question de la méthode: chirurgicale ou dispositif spécifique ? Ce travail apporte clairement une réponse. Des personnels de santé novice obtiennent de meilleurs résultats avec la technique chirurgicale. Même si la technique utilisée n'est pas celle promue par la procédure du sauvetage au combat (emploi d'un crochet de hook au lieu d'une pince de Monro-Kelly), ce travail conforte le choix qui est fait d'avoir recours à la technique chirurgicale.
----------------------------------------
Background: When conventional approaches to obtain effective ventilation and return of effective spontaneous breathing fail, surgical airway is the last rescue option. Most physicians have a limited lifetime experience with cricothyrotomy, and it is unclear what method should be taught for this lifesaving procedure. The aim of this study is to compare the performance of medical personnel, naive to surgical airway techniques, in establishing an emergency surgical airway in cadavers using three commonly used cricothyrotomy techniques.
Methods: Twenty medical students, without previous knowledge of surgical airway techniques, were randomly selected from their class. After training, they performed cricothyrotomy by three techniques (surgical, Merkel, and QuickTrach II) in a random order on 60 cadavers with comparable biometrics. The time to complete the procedure, rate of success, and number of complications were recorded. A success was defined as the correct placement of the cannula within the trachea in 3min.
"After intact skin palpation of relevant structures (step 1), a vertical midline skin incision (step 2) is emphasized because it can be extended up or down if not correctly placed and because fewer vessels are located at the midline. Although
rarely emphasized, we recommend finger palpation through the subcutaneous tissue (step 3) and even in the trachea as a guide, as a dissector, and as a dilator; finger palpation is oblivious to bleeding and a better guide to the ligament, being the “surgeon’s eye” during cricothyrotomy. A horizontal incision of the lower aspect of the cricotracheal ligament (step 4) allows for tension release and better opening. A hook permits to maintain the skin and the tracheal opening. Caudal traction (step 5) is recommended because the cricoid cartilage is more resistant and in order to prevent laryngeal injuries. We did not use a dilator, forceps, or a retractor during this experiment. Finally, a cuffed cannula is inserted (step 6)"
Results: The success rates were 95, 55, and 50% for surgical cricothyrotomy, QuickTrach, and Merkel, respectively (P = 0.025).
The majority of failures were due to cannula misplacement (15 of 20). In successful procedures, the mean procedure time was 94± 35 s in the surgical group, 77 ± 34 in the QuickTrach II group, and 149 ±24 in the Melker group (P < 0.001). Few significant complications were found in successful procedures. No cadaver biometric parameters were correlated with success of the procedure.
Conclusion: Surgical airway–naive medical personnel establish emergency cricothyrotomy more efficiently and safely with the surgical procedure than with the other two commonly used techniques
| Tags : airway
12/05/2016
Crico: Incisez large
The inaccuracy of using landmark techniques for cricothyroid membrane identification: a comparison of three techniques
Bair AE et Al. Acad Emerg Med 2015 Aug; 22:908
---------------------------------------------------------
Le recours à la coniotomie est rare mais il s'agit d'un geste technique à connaître pour la prise en charge des obstructions des voies aériennes. Le repérage de la membrane crio-thyroïdienne peut être difficile. Ce travail rappelle que l'identification manuelle de cette dernière est fiable dans moins de 60 % des cas. L'échographie améliorerait la fiabilité de cette localisation (Campbell M et Al. 1) mais ceci n'est pas, et c'est surprenant, retrouvé par tous (Yldiz G et Al. 2). En ce qui nous concerne, la disponibilité d'un appareil d'échographie sur le terrain est peu probable . En cas de difficulté de repérage pensez à réaliser une incision large pour repérer au doigt directement cette membrane (regardez cette vidéo)
---------------------------------------------------------
OBJECTIVES:
Successful cricothyrotomy is predicated on accurate identification of the cricothyroid membrane (CTM) by palpation of superficial anatomy. However, recent research has indicated that accuracy of the identification of the CTM can be as low as 30%, even in the hands of skilled providers. To date, there are very little data to suggest how to best identify this critical landmark. The objective was to compare three different methods of identifying the CTM.
METHODS:
A convenience sample of patients and physician volunteers who met inclusion criteria was consented. The patients were assessed by physician volunteers who were randomized to one of three methods for identifying the CTM (general palpation of landmarks vs. an approximation based on four finger widths vs. an estimation based on overlying skin creases of the neck). Volunteers would then mark the skin with an invisible but florescent pen. A single expert evaluator used ultrasound to identify the superior and inferior borders of the CTM. The variably colored florescent marks were then visualized with ultraviolet light and the accuracy of the various methods was recorded as the primary outcome. Additionally, the time it took to perform each technique was measured. Descriptive statistics and report 95% confidence intervals (CIs) are reported.
RESULTS:
Fifty adult patients were enrolled, 52% were female, and mean body mass index was 28 kg/m(2) (95% CI = 26 to 29 kg/m(2) ). The general palpation method was successful 62% of the time (95% CI = 48% to 76%) and took an average of 14 seconds to perform (range = 5 to 45 seconds). In contrast, the four-finger technique was successful 46% of the time (95% CI = 32% to 60%) and took an average of 12 seconds to perform (range = 6 to 40 seconds). Finally, the neck crease method was successful 50% of the time (95% CI = 36% to 64%) and took an average of 11 seconds to perform (range = 5 to 15 seconds).
CONCLUSIONS:
All three methods performed poorly overall. All three techniques might potentially be even less accurate in instances where the superficial anatomy is not palpable due to body habitus. These findings should alert clinicians to the significant risk of a misplaced cricothyrotomy and highlight the critical need for future research.
23/01/2016
Maîtriser l'airway +++, entre autres
Augmentation of point of injury care: Reducing battlefield
mortality—The IDF experience
Benov A. et Al. Injury. 2015 Nov 18. pii: S0020-1383(15)00697-X. doi: 10.1016/j.injury.2015.10.078.
------------------------------
Une publication particulièrement intéressante car elle émane de collègues militaires qui interviennent dans un contexte très particulier de prise en charge de blessés tels qu'on peut les rencontrer en opérations extérieures mai dans un contexte de réseau de traumatologie civile puisque que les hôpitaux de recueil de ces blessés sont les hôpitaux civils. Les données présentées ne portent que sur la prise en charge de combattants.
Un des points analysé est la performance des équipes dans certains gestes considérés comme essentiel, notamment la gestion des voies aériennes. Comme dans l'armée française l'intubation orotrachéale et la criciothyrotomie représentent les deux procédures mises en oeuvre par des médecins. Manifestement, il existe une grande maîtrise de la coniotomie alors que celle de l'Intubation est moins évidente: 41% de succès et une moyenne de 2 tentatives. Ceci reste problématique lorsque la prise en charge des blessés se fait loin d'un trauma center et qu'il faut envisager la gestion de ces voies aériennes et l'initiation d'une ventilation pendant plusieurs heures (jours ?). Pour ces raisons et même si la probabilité d'être confronté à une telle situation est faible, ce travail rapporte les 2/3 des blessés ne sont pas urgent et que 5% seulement des nécessitent un geste sur les voies aériennes, il s'agit d'un point fondamental en matière de réduction de morts indues.
------------------------------
STUDY OBJECTIVE:
In 2012, the Israel Defense Forces Medical Corps (IDF-MC) set a goal of reducing mortality and eliminating preventable death on the battlefield. A force buildup plan entitled "My Brother's Keeper" was launched addressing: trauma medicine, training, change of Clinical Practice Guidelines (CPGs), injury prevention, data collection, global collaboration and more. The aim of this article is to examine how military medical carehas evolved due "My Brother's Keeper" between Second Lebanon War (SLW, 2006) to Operation Protective Edge (OPE, 2014).
METHODS:
Records of all casualties during OPE and SLW were extracted and analyzed from the I.D.F Trauma Registry. Noncombat injuries and civilian injuries from missile attacks were excluded from this analysis.
RESULTS:
The plans main impacts were; incorporation of a physician or paramedic as an integral part of each fighting company, implementation of new CPGs, introduction of new approaches for extremity haemorrhage control and Remote Damage Control Resuscitation at point of injury (POI) using single donor reconstituted freeze dried plasma (25 casualties) and transexamic acid (98 casualties). During OPE, 704 soldiers sustained injuries compared with 833 casualties during SLW. Fatalities were 65 and 119, respectively, cumulating to Case Fatality Rate of 9.2% and 14.3%, respectively.
CONCLUSIONS:
Significant changes in the way the IDF-MC provides combat casualty care have been made in recent years. It is the transformation from concept to doctrine and integration into a structured and Goal-Oriented Casualty Care System, especially POI care that led to the unprecedented survival rates in IDF as shown in this conflict.
| Tags : airway