07/04/2019
ControlCric: Plutôt à éviter
Necessity to depict difficult neck anatomy for training of cricothyroidotomy: A pilot study evaluating two surgical devices on a new hybrid training model.
BACKGROUND:
Everyone dealing with airway emergencies must be able to accomplish cricothyroidotomy, which cannot be trained in real patients. Training models are necessary.
OBJECTIVE:
To evaluate the suitability of a hybrid training model combining synthetic and porcine parts to depict variable neck anatomy.
DESIGN:
Model-based comparative trial.
SETTING:
Armed Forces Hospital Ulm, Germany, August 2018.
INTERVENTION:
On four anatomical neck variations (long slim/long obese/short slim/short obese) we performed two surgicalrapproaches to cricothyroidotomy (SurgiCric II vs. ControlCric).
PARTICIPANTS:
Forty-eight volunteers divided into two groups based on their personal skill level: beginners group and proficient performers group.
MAIN OUTCOME MEASURES:
Time to completion was recorded for each procedure. Once the operator had indicated completion, the correct anatomical tube placement was confirmed by dissection and structures were inspected for complications. Primary outcomes were successful tracheal placement of an airway tube and time needed to achieve a patent airway. Secondary outcome was assessment of complications.
RESULTS:
Overall, 384 procedures were performed. Median time to completion was 74 s. In total, 284 procedures (74%) resulted in successful ventilation. Time to completion was longer in short obese than in long slim and the risk of unsuccessful procedures was increased in short obese compared with long slim. Even if ControlCric resulted in faster completion of the procedure, its use was less successful and had an increased risk of complications compared with SurgiCric II. Proficient performers group performed faster but had an increased risk of injuring the tracheal wall compared with beginners group.
CONCLUSION:
Participants had difficulties in performing cricothyroidotomy in obese models, but various and difficult anatomical situations must be expected in airway management and therefore must be taught. A new hybrid model combining porcine and synthetic materials offers the necessary conditions for the next step in training of surgical airway procedures.
| Tags : airway
27/03/2019
Management of tracheal intubation in critically ill adults
| Tags : airway
19/03/2019
Trauma et formation: Progrès encore à faire
Surgical interns in 2018: Objective assessment suggests they are better but still lack critical knowledge and skill.
BACKGROUND:
The transition from fourth-year medical student to surgical intern is difficult. A lack of repetitions, experience, and knowledge is problematic. We report our experience using simulation-based technical and nontechnical skills to assess the competency of surgical interns in July and January of their intern year.
DESIGN:
As part of a larger assessment effort, our general surgery interns (2010-2016) have been tested on performing an emergent cricothyrotomy, interpreting 2 arterial blood gases, and reading 3 chest x-rays in fewer than 7 minutes. We retrospectively analyzed general surgery interns' performance on these 3 tests (total score = 20).
RESULTS:
A total of 210 interns completed both July and January (identical) assessments. Overall mean scores improved from July (12.62 ± 3.44) to January (16.5 ± 2.46; P < .05). During the study period general surgery interns' mean baseline scores improved in both July (P < .05) and in January (P < .05). Although most individual general surgery interns did improve their total scores (92% improved, 3% same, 5% worse) between July and January (P < .05), in January 40% could not perform an emergent cricothyrotomy swiftly, and 6% missed a tension pneumothorax on chest x-ray.
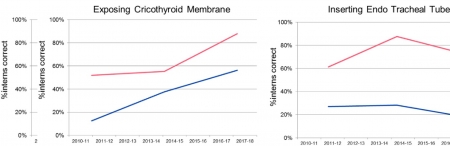
CONCLUSION:
Our data suggest that surgical interns start residency training with low levels of skill and comprehension with emergent cricothyrotomy, arterial blood gas, and chest x-ray. They improve with 6 months of clinical and simulation training. Encouragingly, overall scores for both July and January assessments have improved during the study period. Given that some interns still struggle in January to perform these three tasks, we believe that 2018 interns are better, but still potentially lack critical knowledge and skill.
15/03/2019
Encore à la recherche d'un simulateur de crico
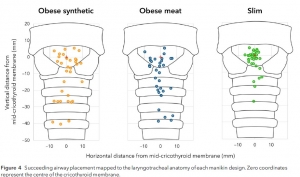
A trial comparing emergency front of neck airway performance in a novel obese-synthetic neck, meat-modified obese neck and conventional slim manikin.
03/03/2019
Crico: Simulation classique = Haute fidélité
A high-fidelity simulator for needle cricothyroidotomy training is not associated with increased proficiency compared with conventional simulators: A randomized controlled study.
BACKGROUND:
A high-fidelity task simulator for cricothyroidotomy was created using data from a 3-dimensional (3D) computed tomography scan using a 3D printer. We hypothesized that this high-fidelity cricothyroidotomy simulator results in increased proficiency for needle cricothyroidotomy compared with conventional simulators.
METHODS:
Cricothyroidotomy-naive residents were recruited and randomly assigned to 2 groups, including simulation training with a conventional simulator (Group C) and with a high-fidelity simulator (Group 3D). After simulation training, participants performed cricothyroidotomy using an ex vivo porcine larynx fitted with an endoscope to record the procedure. The primary outcomes were success rate and procedure time. The secondary outcome was a subjective measure of the similarity of the simulator to the porcine larynx.
RESULTS:
Fifty-two residents participated in the study (Group C: n = 27, Group 3D: n = 25). There was no significant difference in the success rate or procedure time between the 2 groups (success rate: P = .24, procedure time: P = .34). There was no significant difference in the similarity of the simulators to the porcine larynx (P = .81).
CONCLUSION:
We developed a high-fidelity simulator for cricothyroidotomy from 3D computed tomography data using a 3D printer. This anatomically high-fidelity simulator did not have any advantages compared with conventional dry simulators.
| Tags : airway, coniotomie
28/01/2019
Crico: Entraînez vous car cela rapporte de la survie
Prehospital cricothyrotomies in a helicopter emergency medical service: analysis of 19,382 dispatches
BACKGROUND:
Creating a patent airway by cricothyrotomy is the ultimate maneuver to allow oxygenation (and ventilation) of the patient. Given the rarity of airway management catastrophes necessitating cricothyrotomy, sufficiently sized prospective randomized trials are difficult to perform. Our Helicopter Emergency Medical Service (HEMS) documents all cases electronically, allowing a retrospective analysis of a larger database for all cases of prehospital cricothyrotomy.
METHODS:
We analyzed all 19,382 dispatches of our HEMS 'Lifeliner 1', since set-up of a searchable digital database. This HEMS operates 24/7, covering ~ 4.5 million inhabitants of The Netherlands. The potential cases were searched and cross-checked in two independent databases.
RESULTS:
We recorded n = 18 cases of prehospital cricothyrotomy. In all 18 cases, less invasive airway techniques, e.g., supraglottic devices, were attempted before cricothyrotomy. With exception of 2 cases, at least one attempt of orotracheal intubation had been performed before cricothyrotomy. Out of the 18 cases, 4 were performed by puncture-based technique (Melker), the remaining 14 cases by surgical technique. Indications for cricothyrotomy were diverse, dividable into 9 trauma cases and 9 medical cases. The procedure was successful in all but one case (17/18, i.e., 94%; with a 95% confidence interval of 72.7-99.9%). Outcome was such that 6/18 patients arrived at the hospital alive. Long term outcome was poor, with only 2/18 patients discharged from hospital alive.
CONCLUSIONS:
Cricothyrotomy remains, although rare, a regularly occurring requirement in (H)EMS. Our finding of a convincingly high success rate of 94% in trained hands encourages training and a timely performance of cricothyrotomy.
05/12/2018
Crico: Manque d'expérience/Entraînement
Emergency front-of-neck airway by ENT surgeons and residents: A dutch national survey
----------------------------
Ce travail hollandais met en avant le caractère non anecdotique des accès chirurgicaux aux voies aériennes. Pour les chirurgiens ORL hollandais, il s'agit essentiellement de trachéotomies. Le faible recours à la coniotomie s'explique surtout par le manque d'entraînement et d'équipements spécifiques. L'article souligne l'importance des démarches d'acquisition et de maintien des compétences, ce qui ne doit pas nous étonner. Comme pour les chirurgiens ORL le besoin d'un programme structuré de formations à l'accès aux voies aériennes en condition de combat est un impératif.
----------------------------
Objectives:
ENT surgeons and anesthesiologists work closely together in managing challenging airway cases. Sharing knowledge, experiences, and expectations interdisciplinary is essential in order to facilitate decision-making and adequate management in emergency front-of-neck airway cases.
Methods:
A survey was performed, to analyze level of experience, technique of preference, training, knowledge of material and protocols, and self-efficacy scores of Dutch ENT surgeons and residents in performing an urgent or emergency front-of-neck airway.
Results:
Within one year (January 2014-2015), 25.7% of the 257 respondents had performed an urgent or emergency front-of-neck airway. Of all reported emergency front-of-neck airways (N = 30), 80% were managed by tracheotomy. In future emergency front-of-neck airway cases, 74% stated cricothyrotomy would be their technique of preference. The majority would choose an uncuffed large-bore cannula technique. Post-academic hands-on training was attended by 42% of respondents. Self-efficacy scores were highest for surgical tracheotomy, and higher when trained or experienced. In case of an emergency scenario, 8.6% would not perform a front-of-neck airway themselves.


The main reasons for reluctance to start in general were lack of experience and lack of training. Reported items for improvement were mainly the development of a protocol and training.
Conclusion:
The chance of encountering an airway emergency scenario requiring front-of-neck airway is realistic. There is inconsistency between advised technique, technique of preference and technique actually performed by ENT surgeons. This study shows that there is both a need and desire for improvement in training and organization of care. Interdisciplinary guidelines and education is needed and could eventually safe lives.
| Tags : airway
02/12/2018
Crico: Incisez VERTICAL et LARGE
Emergency cricothyroidotomy: an observational study to estimate optimal incision position and length
Background
A vertical incision is recommended for cricothyroidotomy when the anatomy is impalpable, but no evidence-based guideline exists regarding optimum site or length. The Difficult Airway Society guidelines, which are based on expert opinion, recommend an 80–100 mm vertical caudad to cephalad incision in the extended neck position. However, the guidelines do not advise the incision commencement point. We sought to determine the minimum incision length and commencement point above the suprasternal notch required to ensure that the cricothyroid membrane would be accessible within its margins.
Methods
We measured using ultrasound, in 80 subjects (40 males and 40 females) without airway pathology, the distance between the suprasternal notch and the cricothyroid membrane, in the neutral and extended neck positions. We assessed the inclusion of the cricothyroid membrane within theoretical incisions of 0–100 mm in length made at 10 mm intervals above the suprasternal notch.
Results
In 80 subjects (40 males and 40 females), the distance ranged from 27 to 105 mm. Movement of the cricothyroid membrane on transition from the neutral to extended neck position varied from 15 mm caudad to 27 mm cephalad.
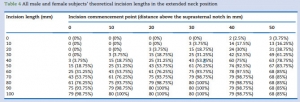
The minimum incision required in the extended position was 70 mm in males and 80 mm in females, commencing 30 mm above the suprasternal notch.
Conclusions
An 80 mm incision commencing 30 mm above the suprasternal notch would include all cricothyroid membrane locations in the extended position in patients without airway pathology, which is in keeping with the Difficult Airway Society guidelines recommended incision length.
| Tags : airway
19/10/2018
Intubation dans le noir: Plutôt Poncho que JVN
OBJECTIVE:
Strict blackout discipline is extremely important for all military units. To be able to effectively determine wound characteristics and perform the necessary interventions at nighttime, vision and light restrictions can be mitigated through the use of tactical night vision goggles (NVGs). The lamp of the classical laryngoscope (CL) can be seen with the naked eye; infrared light, on the other hand, cannot be perceived without the use of NVGs. The aim of the study is to evaluate the safety of endotracheal intubation (ETI) procedures in the darkunder tactically safe conditions with modified laryngoscope (ML) model.
METHODS:
We developed an ML model by changing the standard lamp on a CL with an infrared light-emitting diode lamp to obtain a tool which can be used to perform ETI under night conditions in combination with NVGs. We first evaluated the safety of ETI procedures in prehospital conditions under darkness by using both the CL and the ML for the study, and then researched the procedures and methods by which ETI procedure could be performed in the dark under tactically safe conditions. In addition, to better ensure light discipline in the field of combat, we also researched the benefits, from a light discipline standpoint, of using the poncho liner (PL) and of taking advantage of the oropharyngeal region during ETIs performed by opening the laryngoscope blades directly in the mouth and using a cover. During the ETI procedures performed on the field, two experienced combatant staff simulated the enemy by determining whether the light from the two different types of laryngoscope could be seen at 100-m intervals up to 1,500 m.
RESULTS:
In all scenarios, performing observations with an NVG was more advantageous for the enemy than with the naked eye. The best measure that can be taken against this threat by the paramedic is to ensure tactical safety by having an ML and by opening the ML inside the mouth with the aid of a PL. The findings of the study are likely to shed light on the tactical safety of ETI performed with NVGs under darkness.
CONCLUSION:
Considering this finding, we still strongly recommend that it would be relatively safer to open the ML blade inside the mouth and to perform the procedures under a PL. In chaotic environments where it might become necessary to provide civilian health services for humanitarian aid purposes (Red Crescent, Red Cross, etc.) without NVGs, we believe that it would be relatively safer to open the CL blade inside the mouth and to perform the procedures under a PL.
05/10/2018
Conio: Echo, cela se confirme
Ultrasound Is Superior to Palpation in Identifying the Cricothyroid Membrane in Subjects with Poorly Defined Neck Landmarks: A Randomized Clinical Trial.
BACKGROUND: Success of a cricothyrotomy is dependent on accurate identification of the cricothyroid membrane. The objective of this study was to compare the accuracy of ultrasonography versus external palpation in localizing the cricothyroid membrane.
METHODS:
In total, 223 subjects with abnormal neck anatomy who were scheduled for neck computed-tomography scan at University Health Network hospitals in Toronto, Canada, were randomized into two groups: external palpation and ultrasound. The localization points of the cricothyroid membrane determined by ultrasonography or external palpation were compared to the reference midpoint (computed-tomography point) of the cricothyroid membrane by a radiologist who was blinded to group allocation. Primary outcome was the accuracy in identification of the cricothyroid membrane, which was measured by digital ruler in millimeters from the computed-tomography point to the ultrasound point or external-palpation point. Success was defined as the proportion of accurate attempts within a 5-mm distance from the computed-tomography point to the ultrasound point or external-palpation point.
RESULTS:
The percentage of accurate attempts was 10-fold greater in the ultrasound than external-palpation group (81% vs. 8%; 95% CI, 63.6 to 81.3%; P < 0.0001). The mean (SD) distance measured from the external-palpation to computed-tomography point was five-fold greater than the ultrasound to the computed-tomography point (16.6 ± 7.5 vs. 3.4 ± 3.3 mm; 95% CI, 11.67 to 14.70; P < 0.0001).
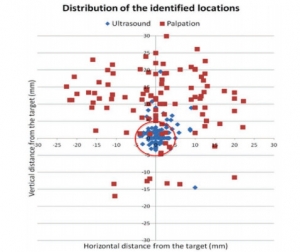
Analysis demonstrated that the risk ratio of inaccurate localization of the cricothyroid membrane was 9.14-fold greater with the external palpation than with the ultrasound (P < 0.0001). There were no adverse events observed.
CONCLUSIONS:
In subjects with poorly defined neck landmarks, ultrasonography is more accurate than external palpation in localizing the cricothyroid membrane.
| Tags : airway, coniotomie
21/09/2018
Coniotomie: Control-Cric pas optimal
A Randomized Comparative Assessment of Three Surgical Cricothyrotomy Devices on Airway Mannequins.
Dorsam J et Al. Prehosp Emerg Care. 2018 Sep 1:1-30
-------------
La réalisation d'une coniotomie peut se faire par voie percutanée avec mandrin souple ou chirurgical, aidée ou pas d'une bougie. L'armée américaine recommande dans sa dernière révision du TCCC le recours à un dispositif appelé control-kit. Les données sur lesquelles reposent une telle proposition sont minces. Ce travail n'est clairement pas en sa faveur, du moins sur le modèle de moulage utilisé pour l'étude. La référence reste donc la technique chirurgicale.
-------------
BACKGROUND:
Airway obstruction is the second leading cause of preventable battlefield death, at least in part because surgical cricothyrotomy (SC) failure rates remain unacceptably high. Ideally, SC should be a rapid, simple, easily-learned, and reliably-performed procedure. Currently, Tactical Combat Casualty Care (TCCC) has approved three SC devices: The Tactical CricKit® (TCK), Control-Cric™(CC), and Bougie-assisted Technique (BAT). However, no previous studies have compared these devices in application time, application success, user ratings, and user preference.
METHODS:
United States Navy Corpsmen (N = 25) were provided 15 minutes of standardized instruction, followed by hands-on practice with each device on airway mannequins. Participants then performed SC with each of the three devices in a randomly assigned sequence. In this within-subjects design, application time, application success, participant ratings, and participant preference data were analyzed using repeated-measures ANOVA, regression, and non-parametric statistics at p < 0.05.
RESULTS:
Application time for CC (M = 184 sec, 95% CI 144-225 sec) was significantly slower than for BAT (M = 135 sec, 95% CI 113-158 sec, p < 0.03) and TCK (M = 117 sec, 95% CI 93-142 sec, p < 0.005). Success was significantly greater for BAT (76%) than for TCK (40%, p < 0.02) and trended greater than CC (48%, p = 0.07).
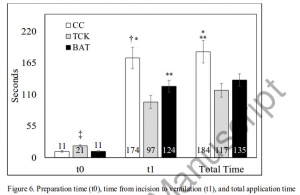
CC was rated significantly lower than TCK and BAT in ease of application, effectiveness, and reliability (each p < 0.01). User preference was significantly (p < 0.01) higher for TCK (58%) and BAT (42%) than for CC (0%). Improved CC blade design was the most common user suggestion.
CONCLUSION:
While this study was limited by the use of mannequins in a laboratory environment, present results indicate that none of these devices was ideal for performing SC. Based on slow application times, low success rates, and user feedback, the Control-Cric™ cannot be recommended until improvements are made to the blade design.
| Tags : airway
Airway Ultrasound
| Tags : airway
15/09/2018
Coniotomie: Ne pas endommager le mandrin
Front-of-neck access and bougie trapping

| Tags : airway, coniotomie
01/08/2018
Cricothyrotomie: Chirurgicale et tous les ans ++
A bench study comparing between scalpel-bougie technique and cannula-to-Melker technique in emergency cricothyroidotomy in a porcine model
Chang SS et Al. Korean Journal of Anesthesiology 2018;71(4):289-295.
Background: The ideal emergency cricothyroidotomy technique remains a topic of ongoing debate. This study aimed to compare the cannula-to-Melker technique with the scalpel-bougie technique and determine whether yearly training in cricothyroidotomy techniques is sufficient for skill retention.
Methods: We conducted an observational crossover bench study to compare the cannula-to-Melker with the scalpel-bougie technique in a porcine tracheal model. Twenty-eight anesthetists participated. The primary outcome was time taken for device insertion. Secondary outcomes were first-pass success rate, incidence of tracheal trauma, and technique preference. We also compared the data on outcome measures with the data obtained in a similar workshop a year ago.
Results: The scalpel-bougie technique was significantly faster than the cannula-to-Melker technique for cricothyroidotomy (median time of 45.2 s vs. 101.3 s; P = 0.001). Both techniques had 100% success rate within two attempts; there were no significant differences in the first-pass success rates and incidence of tracheal wall trauma (P > 0.999 and P = 0.727, respectively) between them. The relative risks of inflicting tracheal wall trauma after a failed cricothyroidotomy attempt were 6.9 (95% CI 1.5–31.1), 2.3 (95% CI 0.3–20.7) and 3.0 (95% CI 0.3–25.9) for the scalpel-bougie, cannula-cricothyroidotomy, and Melker-Seldinger airway, respectively. The insertion time and incidence of tracheal wall trauma were lower when the present data were compared with data from a similar workshop conducted the previous year.
Conclusions: This study supports the use of a scalpel-bougie technique for cricothyroidotomy by anesthetists and advocates a yearly training program for skill retention
20/04/2018
Coniotomie: Au moins 15 ml
Surgical cricothyrotomy: the tracheal-tube dilemma.
Editor—In a recent issue of the British Journal of Anaesthesia, Higgs and colleagues1 published guidelines for the management of tracheal intubation in critically ill adults. I appreciate the authors' successful efforts for implementation of comprehensive guidelines to improve airway management and patient safety in the intensive-care-unit environment. In accordance with current evidence and expert opinion, the authors recommend an open surgical approach (surgical cricothyrotomy) for emergency front-of-neck access in adult patients. They highlight the benefits of this technique: it is fast, reliable, has a high success rate, and provides definitive access to the airway. After incision of the cricothyroid membrane, insertion of a tracheal tube via a bougie stylet is advocated. The use of tracheal tubes with an inner diameter (ID) of 5.0 or 6.0 mm is advised, presumably because of the dimensions of the cricothyroid membrane.
Insertion of ‘standard’ tracheal tubes with an ID of 5.0 or 6.0 mm generates a dilemma of potentially limiting the benefits of the surgical technique. The cuff diameter of a tracheal tube of ID 6.0 mm with a high-volume low-pressure cuff is 18–19 mm, or about 13 mm in a tracheal tube of ID 5.0 mm. The upper limits of normal for coronal and sagittal diameters of the trachea in men of 20–79 yr average 25–27 mm, and in women 21–23 mm. The disparity between the diameters of the inflated cuff and the trachea potentially generates a leak.
Insufflation of oxygen via a standard tracheal tube should provide sufficient oxygenation. But, further gains of a surgical approach with tracheal-tube insertion, such as confirmation of success by waveform capnography, protection against aspiration, and application of PEEP, are possibly impeded because of insufficient cuff seal. Thus, are standard tracheal tubes superior for this challenging scenario?
Given its advantages, surgical cricothyrotomy is the recommended technique in the ‘cannot intubate, cannot oxygenate’ scenario. To overcome the problem of leakage caused by the mismatch of small tracheal-tube cuff and tracheal diameters, we equip all cricothyrotomy kits for adults with micro-laryngeal tubes (MLTs) ID 5.0 and 6.0 mm (Rüsch® micro-laryngeal endotracheal tube; Teleflex Medical GmbH, Belp, Switzerland). Designed for laryngeal or tracheal surgery and patients with tracheal stenosis, these tubes offer smaller inner (5.0 or 6.0 mm) and outer (7.3 and 8.7 mm) diameters to provide better visualisation and access to the surgical site. But, the cuff diameter averages 31 mm, about the cuff diameter of a standard ID 8.0 mm tube. It is possible to place an ID 5.0 or 6.0 mm tube through the incision in the cricoid membrane, whilst simultaneously achieving a sufficient seal in adults, enabling positive pressure ventilation, sufficient expiration, capnography, etc. We have used this successfully in mannequin tests and in emergencies. I recommend routine use of MLTs instead of standard tracheal tubes for surgical cricothyrotomy procedures in adults, and encourage the authors to take these considerations into account for future updates of their excellent guidelines.
Réponse
Response to 'Surgical cricothyroidotomy-the tracheal tube dilemma'.
Tracheal tube Cuff diameters inflated using different volumes of air, (mm)-including diameter stated on packaging
| Tube inner diameter (mm) | Stated cuff diameter (mm) | 12 ml inflated (mm) | 15 ml inflated (mm) | 20 ml inflated (mm) |
|---|---|---|---|---|
| 5.0 | 18 | 25 | 26 | 27 |
| 5.5 | 21 | 25 | 27 | 30 |
| 6.0 | 22 | 26 | 28 | 30 |
18/03/2018
Control Cric: Pas mieux que la conio chirurgicale
A randomized cross-over study comparing surgical cricothyrotomy techniques by combat medics using a synthetic cadaver model
Cricothyrotomy is a complex procedure with a high rate of complications including failure to cannulate and injury to adjacent anatomy. The Control-Cric™ System and QuickTrach II™ represent two novel devices designed to optimize success and minimize complications with this procedure. This study compares these two devices against a standard open surgical technique.
METHODS:
We conducted a randomized crossover study of United States Army combat medics using a synthetic cadaver model. Participants performed a surgical cricothyrotomy using the standard open surgical technique, Control-Cric™ System, and QuickTrach II™ device in a random order. The primary outcome was time to successful cannulation. The secondary outcome was first-attempt success. We also surveyed participants after performing the procedures as to their preferences.
RESULTS:
Of 70 enrolled subjects, 65 completed all study procedures. Of those that successfully cannulated, the mean times to cannulation were comparable for all three methods: standard 51.0s (95% CI 45.2-56.8), QuickTrach II™ 39.8s (95% CI 31.4-48.2) and the Cric-Control™ 53.6 (95% CI 45.7-61.4). Cannulation failure rates were not significantly different: standard 6.2%, QuickTrach II™ 13.9%, Cric-Control™ 18.5% (p=0.106). First pass success rates were also similar (93.4%, 91.1%, 88.7%, respectively, p=0.670). Of respondents completing the post-study survey, a majority (52.3%) preferred the QuickTrach II™ device.
CONCLUSIONS:
We identified no significant differences between the three cricothyrotomy techniques with regards to time to successful cannulation or first-pass success.
| Tags : airway
12/03/2018
Voies aériennes: L'expérience US OIF/OEF
BACKGROUND:
Airway management is of critical importance in combat trauma patients. Airway compromise is the second leading cause of potentially survivable death on the battlefield and accounts for approximately 1 in 10 preventable deaths. Reports from the Iraq and Afghanistan wars indicate 4-7% incidence of airway interventions on casualties transported to combat hospitals. The goal of this study was to describe airway management in the prehospital combat setting and document airway devices used on the battlefield.
METHODS:
This study is a retrospective review of casualties that required a prehospital life-saving airway intervention during combat operations in Afghanistan. We obtained data from the Prehospital Trauma Registry (PHTR) that was linked to the Department of Defense Trauma Registry (DoDTR) for outcome data for the time period between January 2013 and September 2014.
RESULTS:
705 total trauma patients were included, 16.9% required a prehospital airway management procedure. There were 132 total airway procedures performed, including 83 (63.4%) endotracheal intubations and 26 (19.8%) nasopharyngeal airway placements. Combat medics were involved in 48 (36.4%) of airway cases and medical officers in 73 (55.3%). Most (94.2%) patients underwent airway procedures due to battle injuries caused by explosion or gunshot wounds.
Casualties requiring airway management were more severely injured and less likely to survive as indicated by injury severity score, responsiveness level, Glascow coma score, and outcome.
CONCLUSIONS:
Percentages of airway interventions more than tripled from previous reports from the wars in Afghanistan and Iraq. These changes are significant and further study is needed to determine the causes. Casualties requiring airway interventions sustained more severe injuries and experienced lower survival than patients who did not undergo an airway procedure, findings suggested in previous reports.
11/02/2018
Airway: Prévention des complications
| Tags : airway
12/05/2017
Membrane Cricoïdienne: Histoire de hauteur
The height of the cricothyroid membrane on computed tomography scans in trauma patients
Nutbeam T. et Al. Anaesthesia. 2017 May 2. doi: 10.1111/anae.13905.
---------------------------------
Un travail très intéressant qui met en avant le fait que la hauteur de la membrane cricoïdienne est moindre que ce que l'on pensait, qu'elle est en fait peu dépendante des conditions d'extension du cou et qu'une canule de 6 mm n'est pas celle qui sera insérée le plus facilement.
---------------------------------
Emergency cricothyrotomy is a common feature in all difficult airway algorithms. It is the final step following a ‘can’t intubate, can’t oxygenate’ scenario. It is rarely performed and has a significant failure rate. There is variation in the reported size of the cricothyroid membrane, especially across population groups. Procedural failure may result from attempting to pass a device with too large an external diameter through the cricothyroid membrane. We aimed to determine the maximum height of the cricothyroid membrane in a UK trauma population. Electronic callipers were used to measure the maximum height of the cricothyroid membrane on 482 reformatted trauma computed tomography scans, 377 (78.2%) of which were in male patients. The mean (SD) height of the cricothyroid membrane, as independently measured by two radiologists, was 7.89 (2.21) mm and 7.88 (2.22) mm in male patients, and 6.00 (1.76) mm and 5.92 (1.71) mm in female patients. The presence of concurrent tracheal intubation or cervical spine immobilisation was found not to have a significant effect on cricothyroid membrane height.
| Device | External diameter; mm | Proportion of study population in whom the mean cricothyroid membrane height > external diameter of device |
|---|---|---|
| 6.0 mm internal diameter tracheal tube | 8.0 | 36.2% |
| 5.0 mm internal diameter tracheal tube | 6.7 | 60.5% |
| 4.0 mm internal diameter tracheal tube | 5.6 | 77.6% |
| 3.0 mm internal diameter tracheal tube | 4.2 | 93.2% |
| Shiley tracheostomy 7.5 mm internal diameter | 10.8 | 7.7% |
| Melker cricothyrotomy set | 8.2 | 34.6% |
| TracheoQuick cricothyrotomy set | 5.0 | 86.5% |
The cricothyroid membrane height in the study population was much smaller than that previously reported.Practitioners encountering patients who may require an emergency surgical airway should be aware of these data. Rescue airway equipment with variety of external diameters should be immediately available.
| Tags : airway
22/01/2017
Crico avec un opinel ? Possible
Bystander cricothyroidotomy with household devices - A fresh cadaveric feasibility study.
In various motion pictures, medical TV shows and internet chatrooms, non-medical devices were presented as tools for life-saving cricothyroidotomies. However, there is uncertainty about whether it is possible for a bystander to perform a cricothyroidotomy and maintain gas exchange using improvised household items. This study examines the ability of bystanders to carry out an emergency cricothyroidotomy in fresh human cadavers using only a pocket knife and a ballpoint pen.
MATERIALS AND METHODS:
Two commonly available pens and five different pocket knives were used. Ten participants with no or only basic anatomical knowledge had to choose one of the pens and one of the knives and were asked to perform a cricothyroidotomy as quickly as possible after a short introduction. Primary successful outcome was a correct placement of the pen barrel and was determined by the thoracic lifting in a mouth-to-pen resuscitation.
RESULTS:
Eight (80%) participants performed a successful approach to the upper airway with a thoracic lifting at the end. Five participants performed a cricothyroidotomy and three performed an unintentional tracheotomy. Injuries to muscles and cartilage were common, but no major vascular damage was seen in the post-procedural autopsy. However, mean time in the successful group was 243s.
CONCLUSION:
In this cadaveric model, bystanders with variable medical knowledge were able to establish an emergency cricothyroidotomy in 80% of the cases only using a pocketknife and a ballpoint pen. No major complications (particularly injuries of arterial blood vessels or the oesophagus) occurred. Although a pocket knife and ballpoint pen cricothyroidotomy seem a very extreme procedure for a bystander, the results of our study suggest that it is a feasible option in an extreme scenario. For a better outcome, the anatomical landmarks of the neck and the incision techniques should be taught in emergency courses.
| Tags : airway