29/07/2019
Methoxyflurane en altitude ? Mais oui
WIlkes M et Al. Wilderness Environ Med. 2018 Sep;29(3):388-391.
Methoxyflurane is a volatile, fluorinated anesthetic agent with analgesic properties. Although no longer used as an anesthetic due to concerns regarding renal toxicity in high doses, it has enjoyed a resurgence as an inhaled analgesic in prehospital care and in the emergency department. The agent is nonflammable and leads to rapid, titratable analgesia without intravenous access. The Penthrox inhaler device is light, robust, and straightforward to administer. Consequently, it has been proposed as an ideal analgesic for the remote high altitude setting.

We report its use for procedural analgesia during suprapubic aspiration for acute urinary retention at a remote rescue post at night, in cold winter conditions, at 4470 m altitude in Machermo, Nepal. We found that methoxyflurane provided rapid, effective analgesia for our patient’s visceral and procedural pain. The inhaler was easy to administer, and the patient remained responsive to voice, with satisfactory oxygen saturation and respiratory rate throughout. We also briefly review the administration, dosing, efficacy, and safety of methoxyflurane and its role in remote medical care.
Penthrox: Risque d'hyperthermie maligne ?
An in-vitro model of malignant hyperthermia: differential effects of inhalation anesthetics on caffeine-induced muscle contractures.
Clinical concentrations of anesthetics augment caffeine-induced contracture of frog sartorius muscle; however, anesthetics differ in this characteristic. The potentiation was quantitated using six paired sartorius muscles for each specified concentration of anesthetic and controls. At a concentration of 1 MAC, the greatest potentiation occurred with 2 mM caffeine for all anesthetics studied. Under these conditions the order of magnitude of augmentations was: chloroform (15 times); halothane (11 times); methoxyflurane (10 times); cyclopropane (5 times); enflurane (4 times); isoflurane (3 times); diethyl ether (2 times); Baxter 3224 (2 times); fluroxene (1.4 times); nitrous oxide (1.3 times).
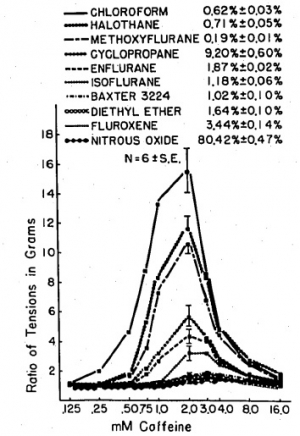
Halothane at .5 MAC augments the 2 mM caffeine-induced contracture almost seven times, and at 2 MAC almost 13 times, whereas 2 MAC isoflurane potentiates the caffeine-induced contracture only four times and 4 MAC diethyl ether only two and a half times. It is postulated that those anesthetics that most potentiate caffeine-induced contracture may be the most potent triggering agents of malignant hyperthermia.
28/07/2019
SAM JT extender:Pourles plaies axillaires
26/07/2019
Maîtriser l'intubation: Un vrai challenge
Procedural Experience With Intubation: Results From a National Emergency Medicine Group.
---------------------------------
Un geste à laquelle les médecins urgentistes US sont peu exposés dans leur pratique quotidienne. Un vrai challenge personnel et pour les formateurs notamment des centres de simulations.
---------------------------------
STUDY OBJECTIVE:
Although intubation is a commonly discussed procedure in emergency medicine, the number of opportunities for emergency physicians to perform it is unknown. We determine the frequency of intubation performed by emergency physicians in a national emergency medicine group.
METHODS:
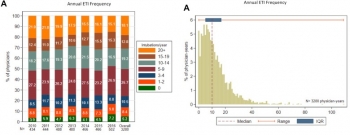
Using data from a national emergency medicine group (135 emergency departments [EDs] in 19 states, 2010 to 2016), we determined intubation incidence per physician, including intubations per year, intubations per 100 clinical hours, and intubations per 1,000 ED patient visits. We report medians and interquartile ranges (IQRs) for estimated intubation rates among emergency physicians working in general EDs (those treating mixed adult and pediatric populations).
RESULTS:
We analyzed 53,904 intubations performed by 2,108 emergency physicians in general EDs (53,265 intubations) and pediatric EDs (639 intubations). Intubation incidence varied among general ED emergency physicians (median 10 intubations per year; IQR 5 to 17; minimum 0, maximum 109). Approximately 5% of emergency physicians did not perform any intubations in a given year. During the study, 24.1% of general ED emergency physicians performed fewer than 5 intubations per year (range 21.2% in 2010 to 25.7% in 2016).
Emergency physicians working in general EDs performed a median of 0.7 intubations per 100 clinical hours (IQR 0.3 to 1.1) and 2.7 intubations per 1,000 ED patient visits (IQR 1.2 to 4.6).
CONCLUSION:
These findings provide insights into the frequency with which emergency physicians perform intubations.
25/07/2019
Crico: Plutôt une lame de 20 ?
Scalpel bougie tube versus hook-assisted emergency front of neck airway—a prospective randomised bench top study in porcine larynges
Caulfield K. et Al. https://doi.org/10.1016/j.bja.2019.05.017
Cette lettre a pour objet de comparer l'insertion d'une canule au travers de la membrane crico-thyroidienne d'un larynx de cochon (membrane que l'on sait relativement profonde) soit en utilisant un crochet de Hook soit une bougie. Les deux techniques se valent. Chose intéressante ils observent près de 17% de difficultés d'insertion avec une lame de 10 versus 7% avec une lame de 20. Cette dernière, qui est une version XL de la lame 10, semble donc préférable ?

"...In the Phase 1 study, the maximum sized ET tube to be placed into the CTM was a size 8. Time to insertion of ET tube averaged 30 s using a Size 20 blade and 31 s using a size 10 blade for all ETT sizes. There was a 16% recorded difficulty by candidates with the size 10 blade and only 7.5% recorded difficulty with the size 20 blade. In the Phase 2 study (blinded RCT), all attempted eFONA attempts were ultimately successful. There were no differences in time required, proportion successful in less than 40 s, or perceived difficulty between groups. Neither CTM incision width nor the proportion of attempts requiring re-incision was different between groups. Reassuringly, all eFONA attempts with both techniques were successful. Neither technique outperformed the other in any aspect of performance."
PGR + Plasma pour une meilleure survie long terme
Is prehospital blood transfusion effective and safe in haemorrhagic trauma patients? A systematic review and meta-analysis.
BACKGROUND:
Life-threatening haemorrhage accounts for 40% mortality in trauma patients worldwide. After bleeding control is achieved, circulating volume must be restored. Early in-hospital transfusion of blood components is already proven effective, but the scientific proof for the effectiveness of prehospital blood-component transfusion (PHBT) in trauma patients is still unclear.
OBJECTIVE:
To systematically review the evidence for effectiveness and safety of PHBT to haemorrhagic trauma patients.
METHODS:
CINAHL, Cochrane, EMBASE, and Pubmed were searched in the period from 1988 until August 1, 2018. Meta-analysis was performed for matched trauma patients receiving PHBT with the primary outcomes 24-hour mortality and long-term mortality. Secondary outcome measure was adverse events as a result of PHBT.
RESULTS:
Trauma patients who received PHBT with simultaneous use of packed red blood cells (pRBCs) and plasma showed a statistically significant reduction in long-term mortality (OR = 0.51; 95% CI, 0.36-0.71; P < 0.0001) but no difference in 24-hour mortality (OR = 0.47, 95% CI, 0.17-1.34; P = 0.16). PHBT with individual use of pRBCs showed no difference in long-term mortality (OR = 1.18; 95% CI, 0.93-1.49; P = 0.17) or 24-hour mortality (OR = 0.92; 95% CI, 0.46-1.85; P = 0.82).
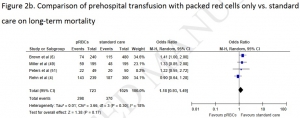
In a total of 1341 patients who received PHBT, 14 adverse events were reported 1.04%, 95% CI 0.57-1.75%.
CONCLUSIONS:
PHBT with simultaneous use of both pRBCs and plasma resulted in a significant reduction in the odds for long-term mortality. However, based on mainly poor quality evidence no hard conclusion can be drawn about a possible survival benefit for haemorrhagic trauma patients receiving PHBT. Overall, PHBT is safe but results of currently ongoing randomised controlled trials have to be awaited to demonstrate a survival benefit.
24/07/2019
Examiner un bassin: Peu faible en préhospitalier
Clinical Examination of the Pelvic Ring in the Prehospital Phase.
INTRODUCTION:
Instable pelvic fractures are associated with significant hemorrhage and shock. Instability of the pelvic ring should be tested with the manual compression test (MCT) and instable pelvic ring fractures should prompt mechanical stabilization. However, the accuracy of the prehospital MCT in patients, that sustained a high energetic trauma, is still unknown.
SETTING:
Radboudumc Nijmegen, level 1 trauma center, the Netherlands.
METHODS:
This prospective blind observational study included all patients after a high impact blunt trauma treated by an experienced Helicopter Emergency Medical Service (HEMS) physician. Nominal arranged questionnaires were filled in by the HEMS physician prior to the radiological examination of the patient.
RESULTS:
We included 56 patients of which 11 sustained a pelvic ring fracture. 13 patients were treated with pelvic compression devices, of which only five patients had a pelvic ring fracture. Prehospital performed clinical examination by the HEMS physicians had an overall sensitivity of 0.45 (95% CI 0.16-0.75) and a specificity of 0.93 (95% CI 0.29-0.96).
CONCLUSION:
Pelvic ring instability cannot accurately be diagnosed in the prehospital setting, based on the MCT. The use of the pelvic binder should standard in high impact blunt trauma patients, independently of the MCT or trauma mechanism.
| Tags : pelvis
18/07/2019
Easywarm: Une autre couverture chauffante
ISR chez le traumatisé: Etomidate toujours pas convaincant
Pre-hospital emergent intubation in trauma patients: the influence of etomidate on mortality, morbidity and healthcare resource utilization.
-------------------------------------------
Cette publication revient sur le débat qui porte sur l'emploi de l'étomidate pour l'intubation préhospitalière. Son emploi est remis en cause par certains, notamment à cause de ses effets dépresseurs cortico-surrénaliens tout particulièrement en cas de sepsis. Les auteurs, si ils ne rapportent pas d'effets délétères sur la mortalité, mettent en évidence une durée d'hospitalisation et de ventialtion plus longue dans le groupe ETO. Plusieurs informations méritent une lecture critique de ce travail. Le premier est la présence dans le groupe non-ETO de thiopental, responsable de nombreux décès lors de l'attaque de pearl harbour (1). La seconde est l'augmentation significative de défaillance cardio-vasculaire dan le groupe non-ETO. On peut se poser la question de l'impact du thiopental dans ce groupe. Le propofol peut également être à l'origine d'une instabilité hémodynamique et nécessite un vrai apprentissage. La quatrième réflexion porte sur le niveau de qualification, qui n'est pas précisé, des personnels réalisant ces intubations.
Ce document ne permet pa de remettre en question la recommandation d'emploi de la Kétamine pour l'ISR dans le cadre de la mise en condition de survie du blessé de guerre (2).
-------------------------------------------
BACKGROUND:
Due to its favorable hemodynamic characteristics and by providing good intubation conditions etomidate is often used for induction of general anesthesia in trauma patients. It has been linked to temporary adrenal cortical dysfunction. The clinical relevance of this finding after a single-dose is still lacking appropriate evidence.
METHODS:
This retrospective multi-centre study is based on merged data from a German Helicopter Emergency Medical Service (HEMS) database and a large trauma patient registry. All trauma patients who were intubated prior to hospital admission with a documented Injury Severity Score ≥ 9 between 2008 and 2012 were eligible for analysis. The primary endpoint was hospital mortality. Other outcome measures were organ failures, sepsis, length of ventilation, as well as length of stay in hospital and ICU.
RESULTS:
One thousand six hundred ninety seven patients were enrolled into the study. Seven hundred sixty two patients received etomidate and 935 patients received other induction agents. The in-hospital mortality was similar in both groups (18.9% versus 18.2%; p = 0.71). Incidences of organ failures and sepsis were not increased in the etomidate group. However, health care resource utilization parameters were prolonged (after adjusting: + 1.3 days for ICU length of stay, p = 0.062; + 0.8 days for length of ventilation, p = 0.15; + 2,7 days for hospital length of stay, p = 0.034). A multivariable logistic regression analysis did not identify etomidate as an independent predictor of hospital mortality (OR: 1.10, 95% CI: 0.77-1.57; p = 0.60).
CONCLUSIONS:
This is the largest trial investigating outcome data for trauma patients who had received a single-dose of etomidate for induction of anesthesia. The use of etomidate did not affect mortality. The influence on morbidity and health care resource utilization remains unclear.
| Tags : etomidate, intubation
Miniaturisation: La précision n'est pas au rendez-vous !
-----------------------------------
L'engouement pour la miniaturiation des équipements (PSE, Laryngoscope, Echographe) est grand. Encore faut il que la performance soit au rendez-vous. Ce n'est pas tout à fait le cas avec certains pousse-seringues, notamment en altitude. Ceci est très dommageable dès lors de la mise en oeuvre de perfusion d"amines pressives.
-----------------------------------
BACKGROUND:
Intravenous drug infusions in critically ill patients require accurate syringe infusion pumps (SIPs). This is particularly important during transportation of critically ill patients by helicopter emergency medical services (HEMS), where altitude may influence device performance. Because weight is a real concern in HEMS, new low-weight devices are very appealing. The aim of this study was to compare infusion flow rates delivered by low-weight versus standard SIP devices, in the prehospital emergency medicine setting, at different altitudes.
METHODS:
We conducted a comparative bench study involving five SIP devices (two standard and three low-weight models) at 300, 1700 and 3000 m altitude. The primary endpoint was the flow rate delivered by SIPs for prespecified values. We used two methods to measure flow. The normative method consisted in measuring weight (method A) and the alternate method consisted in measuring instantaneous flow (method B).
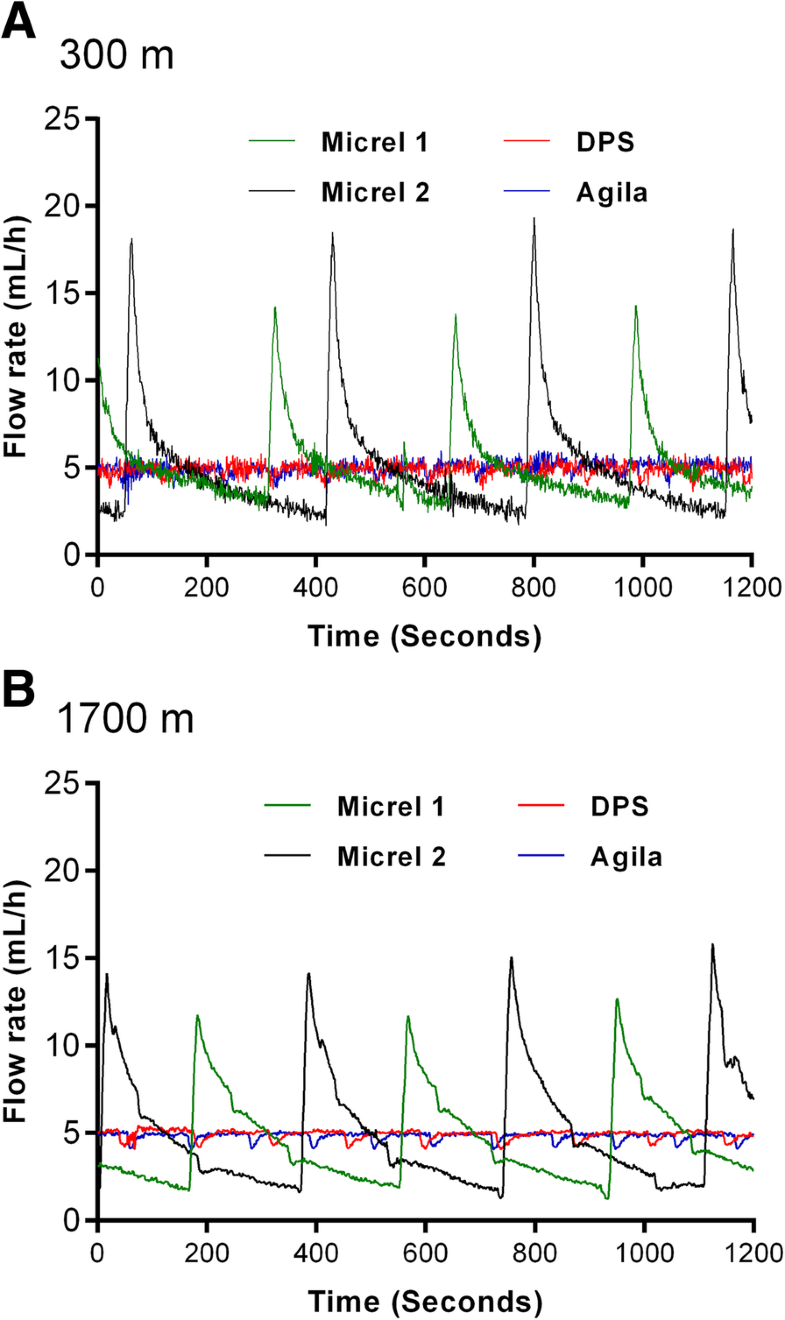
RESULTS:
Using method A, no significant differences were found in median flow rates and interquartile range depending on device and altitude for a prespecified 10-mL/h flow. However, method B showed that low-weight SIPs delivered multiple sequential boluses with substantial variations (1.2-15.8 mL/h) rather than a prespecified continuous 5-mL/h flow. At 1700 m altitude, the interquartile range of delivered flows increased only for low-weight devices (p for interaction< 0.001).
CONCLUSIONS:
Despite satisfactory normative tests, low-weight SIPs deliver discontinuous flow with potential clinical implications for critically ill patients receiving vasoactive drugs. This study also highlights a thus far unknown negative impact of altitude on SIP function. We believe that normative requirements for SIP approval should be revised accordingly.
17/07/2019
Drainage thoracique chez l'enfant: La règle des 4
Rule of 4's: Safe and effective pleural decompression and chest drain insertion in severely injured children.
The intersecting scenarios of multi-trauma, thoracic injury and traumatic cardiac arrest present some of the most demanding moments in paediatric trauma. For these reasons, decision support through teamwork, checklists, technology and guidelines are central to ensuring quality paediatric trauma care. The 'Rule of 4's' is a simple aide-memoire, which guides clinicians of all grades, expertise and distractedness in a reliable approach to injured children who require safe and effective emergency pleural decompression and timely insertion of a chest drain.

The Rule of 4's enables these important therapeutic goals to be met through: (i) four steps in a 'good plan'; (ii) fourth (or fifth) intercostal space as the basis for siting a 'good hole'; (iii) 4× uncuffed endotracheal tube size (4× [age/4 + 4]) to guide selection of a 'good tube'; and (iv) 4 cm mark for a 'good stop' to ensure the drain is in far enough but not too far.
| Tags : drainage thorax
The pre-hospital management of life-threatening chest injuries: A consensus statement from the Faculty of Pre-Hospital Care
| Tags : thorax
16/07/2019
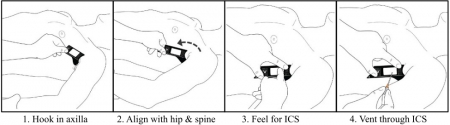
Exsuflation: Plus stable par voie axillaire
Relative device stability of anterior versus axillary needle decompression for tension pneumothorax during casualty movement: Preliminary analysis of a human cadaver model.
-------------------------------
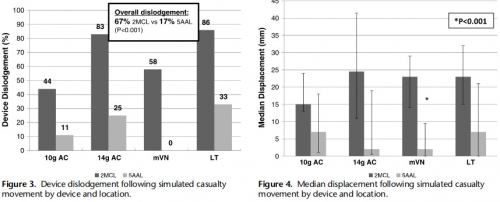
L'étude porte sur la stabilité des cathéters d'exsufflation posés par voie antérieure versus par voie axillaire. Cette dernière voie est associée à un bien moindre risque de délogement pendant un transport que la voie antérieure. Ceci milite pour faire de la voie axillaire la voie de référence, et ce malgré la constatation de lésions parenchymateuses minimes.
-------------------------------
BACKGROUND:
Tension pneumothorax (tPTX) remains a significant cause of potentially preventable death in military and civilian settings. The current prehospital standard of care for tPTX is immediate decompression with a 14-gauge 8-cm angiocatheter; however, failure rates may be as high as 17% to 60%. Alternative devices, such as 10-gauge angiocatheter, modified Veress needle, and laparoscopic trocar, have shown to be potentially more effective in animal models; however, little is known about the relative insertional safety or mechanical stability during casualty movement.
METHODS:
Seven soft-embalmed cadavers were intubated and mechanically ventilated. Chest wall thickness was measured at the second intercostal space at the midclavicular line (2MCL) and the fifth intercostal space along the anterior axillary line (5AAL). CO2 insufflation created a PTX, and needle decompression was then performed with a randomized device. Insertional depth was measured between hub and skin before and after simulated casualty transport. Thoracoscopy was used to evaluate for intrapleural placement and/or injury during insertion and after movement. Cadaver demographics, device displacement, device dislodgment, and injuries were recorded. Three decompressions were performed at each site (2MCL/5AAL), totaling 12 events per cadaver.
RESULTS:
Eighty-four decompressions were performed. Average cadaver age was 59 years, and body mass index was 24 kg/m. The CWT varied between cadavers because of subcutaneous emphysema, but the average was 39 mm at the 2MCL and 31 mm at the 5AAL. Following movement, the 2MCL site was more likely to become dislodged than the 5AAL (67% vs. 17%, p = 0.001).
Median displacement also differed between 2MCL and 5AAL (23 vs. 2 mm, p = 0.001). No significant differences were noted in dislodgement or displacement between devices. Five minor lung injuries were noted at the 5AAL position.
CONCLUSION:
Preliminary results from this human cadaver study suggest the 5AAL position is a more stable and reliable location for thoracic decompression of tPTX during combat casualty transport.
| Tags : exsufflation
Always Ready; Responding to an Emergency at Sea
Always Ready; Responding to an Emergency at Sea
I’m surrounded by the lush jungle of Okinawa on a muggy day,
The warm glow of the sun on my face brings me to life.
The alarm screeches overhead jarring me out of my reverie.
“Attention in the medical bay. This is not a drill.”
An airplane is in the water. Casualties inbound,
The medical bay of the aircraft carrier is abuzz with anticipation.
Drill after drill--for this.
Years of study and experience come down to this one moment.
Medical school;
Field trauma training;
Internship;
Aviation medicine;
Are you ready? Is your team ready? Could you have done more?
We are prepared. We are ready!
Eyes are on you, “Sir, what do we do?”
What do we know? What happened? Who’s involved? Where are they?
Details are scarce.
Take a breath…think…remember your training.
---ABCDE.
Airway, breathing, circulation, disability, environment;
The mantra marches to the forefront of my thoughts like an eager Marine.
Assign roles, prepare the equipment,
New information, the two pilots are my friends.
Only one is recovered. Push the sorrow to the rear. Three minutes out.
We are ready.
The whirling rotors are deafening as we unload the patient,
We move by instinct thanks to constant drilling,
Next thing I know we are in Trauma One.
He has one question, “The crew, are they safe?”
Airway is clear, he is breathing and ventilating. Brain is perfused.
Primary survey; distal femur and posterior hip are shattered,
Our team of nurses, corpsmen, and doctors take to their assigned roles,
We splint the femur and bind the hip.
Medical management with morphine, normal saline, and antibiotics.
A job well done; he is going to be okay.
We medevac him via helicopter to Roll 3 ashore,
His parting words. “Any updates on the crew?”
I tell him answers will come, but I know in my heart the truth.
He is in the water…Our brother is dead.
How do you prepare for that?
14/07/2019
Penthrox: Séduisant mais
Low-dose methoxyflurane analgesia in adolescent patients with moderate-to-severe trauma pain: a subgroup analysis of the STOP! study.
Introduction:
The undertreatment of acute pain presents a significant challenge in the Emergency Department. This post hoc subgroup analysis of a previously reported randomized controlled UK study reports the efficacy and safety of low-dose methoxyflurane analgesia in treating adolescent patients with moderate-to-severe trauma pain.
Patients and methods:
Three hundred patients (96 in the adolescent subgroup) aged ≥12 years requiring analgesia for acute trauma pain (pain score of 4-7 on the Numerical Rating Scale) at triage were randomized 1:1 to methoxyflurane (up to 6 mL) or placebo (normal saline), both administered using a Penthrox® inhaler. The patient could request rescue medication (paracetamol/opioids) at any time. The primary endpoint was the change from baseline in visual analog scale (VAS) pain intensity.
Results:
Mean VAS pain score for the adolescent subgroup at baseline was ~ 61 mm. Adjusted mean change in VAS pain intensity from baseline to 5, 10, 15, and 20 minutes was -24.5, -28.1, -31.6, and -31.7 mm for methoxyflurane and -14.6, -18.8, -19.2, and -23.7 mm for placebo, with a statistically significant treatment effect in favor of methoxyflurane overall across all four time points (-9.9 mm; 95% CI: -17.4, -2.4 mm; P=0.0104). Median time to first pain relief was significantly shorter with methoxyflurane (1 minute) than placebo (3 minutes, P<0.0001). Pain relief was reported within 1-10 inhalations in 95.7% of methoxyflurane-treated patients and 64.6% of placebo-treated patients. Rescue medication was requested by two (4.3%) methoxyflurane-treated patients and three (6.3%) placebo-treated patients. Over 95% of patients, physicians, and nurses rated methoxyflurane treatment as "Excellent", "Very Good" or "Good" compared with between 64% and 68% for placebo. The incidence of adverse events was higher with methoxyflurane (51%) than placebo (42%), mostly comprising mild/transient dizziness and headache.
Conclusion:
This subgroup analysis shows that low-dose inhaled methoxyflurane is a rapid-acting and effective analgesic in adolescent patients presenting with moderate-to-severe trauma pain.
Penthrox: Avis de la HAS
 Le méthoxyflurane a été utilisé dès 1960 en Europe et aux États-Unis comme gaz anesthésiant halogéné à des doses plus élevées et avec des inhalateurs différents de ceux de PENTHROX. Il a été retiré du marché en 1974 compte tenu d’une faible utilisation en anesthésie. De plus, à fortes doses, le méthoxyflurane a été associé à une néphrotoxicité grave liée à la dose et à l’utilisation pendant de longues périodes au cours d’une anesthésie générale. Sous la dénomination PENTHROX liquide pour inhalation par vapeur en flacon de 3 ml, il est utilisé en Australie depuis 1993 et en Nouvelle Zélande depuis 2002 par les services d’urgence en tant qu’analgésique non opioïde, d’urgence. PENTHROX pourrait être une alternative aux antalgiques comme le MEOPA actuellement utilisés dans ces situations de traumatologie.
Le méthoxyflurane a été utilisé dès 1960 en Europe et aux États-Unis comme gaz anesthésiant halogéné à des doses plus élevées et avec des inhalateurs différents de ceux de PENTHROX. Il a été retiré du marché en 1974 compte tenu d’une faible utilisation en anesthésie. De plus, à fortes doses, le méthoxyflurane a été associé à une néphrotoxicité grave liée à la dose et à l’utilisation pendant de longues périodes au cours d’une anesthésie générale. Sous la dénomination PENTHROX liquide pour inhalation par vapeur en flacon de 3 ml, il est utilisé en Australie depuis 1993 et en Nouvelle Zélande depuis 2002 par les services d’urgence en tant qu’analgésique non opioïde, d’urgence. PENTHROX pourrait être une alternative aux antalgiques comme le MEOPA actuellement utilisés dans ces situations de traumatologie.
La spécialité PENTHROX dispose d’une AMM obtenue par procédure décentralisée dans 3 autres pays de l’union européenne en plus de la France : Belgique, Irlande, Royaume-Uni. Elle dispose d’une AMM en Australie depuis 1993 et en nouvelle Zélande depuis 2002 ; elle est commercialisée depuis ces dates dans ces 2 pays.

PENTHROX est une alternative aux antalgiques disponibles dans la prise en charge en urgence de la douleur modérée à sévère. Faute de données, il n’est pas possible de le situer par rapport aux alternatives antalgiques disponibles. Il présente un avantage pratique (pas de voie veineuse, auto-administration). Son principal inconvénient est la nécessité d’obtenir la coopération du patient, ce qui le contre-indique chez l’adulte inconscient ou au contraire agité. De plus, l’administration par voie inhalée limite son utilisation chez le patient présentant une insuffisance respiratoire chronique ou aiguë.
Les effets indésirables les plus fréquents rapportés avec PENTHROX ont été essentiellement les effets sur le système nerveux central tels que les vertiges, la somnolence et les céphalées. De rares cas d’hépatotoxicité ont été rapportés lors de l’utilisation du méthoxyflurane à dose antalgique.
Compte tenu des données cliniques disponibles versus placebo, PENTHROX apporte une réponse partielle au besoin thérapeutique dans le soulagement de la douleur en situation d’urgence. Il subsiste des incertitudes sur son efficacité dans les douleurs les plus sévères (EN>7). De plus, en l’absence de comparaison directe de qualité méthodologique satisfaisante, il n’est pas possible de le situer par rapport aux alternatives antalgiques disponibles. De ce fait, son impact sur la morbidité et sur la qualité de vie n’est à ce jour pas démontré. Par ailleurs, malgré sa praticité d’utilisation potentielle, son impact positif sur l’organisation des soins n’a pas été démontré.
Le service médical rendu est modéré. Compte tenu de :
– l’efficacité de PENTHROX démontrée versus placebo chez des patients ayant majoritairement une douleur d’intensité modérée,
– l’absence d’étude de qualité méthodologique suffisante l’ayant comparé aux autres antalgiques actuellement disponibles,
PENTHROX n’apporte pas d’amélioration du service médical rendu (ASMR V) par rapport aux autres antalgiques disponibles dans le soulagement d’urgence des douleurs modérées à sévères associées à un traumatisme chez des patients adultes conscients.
13/07/2019
Exsuffler au bon endroit: Avec un gabarit ?
ThoraSite: A device to improve accuracy of lateral decompression needle and chest tube placement.
BACKGROUND:
Multiple reports have detailed an unacceptably high error rate in the siting of decompression needles and tubes and describe associated iatrogenic injuries. The objective of the current study was to measure the accuracy of the novel ThoraSite template for identifying an acceptable intercostal space (ICS) for lateral needle or tube thoracostomy.
METHODS:
Two trained operators used the ThoraSite to place radiopaque needles in the left and right lateral chests of 12 cadavers. An independent radiologist reviewed fluoroscopy images to determine the primary outcome: the ICS in which each needle was placed. Secondary outcomes were ICS's palpable through ThoraSite's Safe Zone; needle placement relative to the anterior axillary line (AAL) and midaxillary line (MAL); and percent correct placement (defined as the third, fourth, or fifth ICS from 1 cm anterior to the AAL to 1 cm posterior to the MAL).
RESULTS:
The six female and six male cadavers spanned 4 ft and 11 inches (150 cm) to 6 ft and 7 inches (201 cm), 80 lb (36 kg) to 350 lb (159 kg), and 16 kg/m to 42 kg/m body mass index. All 24 needles were placed in either the third (4 [17%] of 24 needles), fourth (10 [42%] of 24 needles), or fifth ICS (10 [42%] of 24 needles). In 10 (42%) of 24 assessments, two ICSs were palpable in ThoraSite's Safe Zone. All palpable ICSs were either the third (8 [24%] of 34), fourth (15 [44%] of 34); or fifth ICS (11 [32%] of 34).
Twenty-three (96%) of 24 needles were inserted from 1 cm anterior to the AAL to 1 cm posterior to the MAL. Twenty-three (96%) of 24 needle placements were correct.
CONCLUSION:
ThoraSite use was associated with needle placement in the third, fourth, or fifth ICS in an area roughly spanning the AAL to MAL in anatomically diverse cadavers. By facilitating appropriate needle/tube placement, ThoraSite use may decrease iatrogenic injuries. Future study involving representative users may be useful to further evaluate ThoraSite accuracy.