25/07/2019
PGR + Plasma pour une meilleure survie long terme
Is prehospital blood transfusion effective and safe in haemorrhagic trauma patients? A systematic review and meta-analysis.
BACKGROUND:
Life-threatening haemorrhage accounts for 40% mortality in trauma patients worldwide. After bleeding control is achieved, circulating volume must be restored. Early in-hospital transfusion of blood components is already proven effective, but the scientific proof for the effectiveness of prehospital blood-component transfusion (PHBT) in trauma patients is still unclear.
OBJECTIVE:
To systematically review the evidence for effectiveness and safety of PHBT to haemorrhagic trauma patients.
METHODS:
CINAHL, Cochrane, EMBASE, and Pubmed were searched in the period from 1988 until August 1, 2018. Meta-analysis was performed for matched trauma patients receiving PHBT with the primary outcomes 24-hour mortality and long-term mortality. Secondary outcome measure was adverse events as a result of PHBT.
RESULTS:
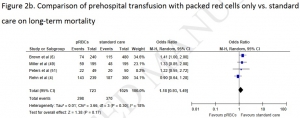
Trauma patients who received PHBT with simultaneous use of packed red blood cells (pRBCs) and plasma showed a statistically significant reduction in long-term mortality (OR = 0.51; 95% CI, 0.36-0.71; P < 0.0001) but no difference in 24-hour mortality (OR = 0.47, 95% CI, 0.17-1.34; P = 0.16). PHBT with individual use of pRBCs showed no difference in long-term mortality (OR = 1.18; 95% CI, 0.93-1.49; P = 0.17) or 24-hour mortality (OR = 0.92; 95% CI, 0.46-1.85; P = 0.82).
In a total of 1341 patients who received PHBT, 14 adverse events were reported 1.04%, 95% CI 0.57-1.75%.
CONCLUSIONS:
PHBT with simultaneous use of both pRBCs and plasma resulted in a significant reduction in the odds for long-term mortality. However, based on mainly poor quality evidence no hard conclusion can be drawn about a possible survival benefit for haemorrhagic trauma patients receiving PHBT. Overall, PHBT is safe but results of currently ongoing randomised controlled trials have to be awaited to demonstrate a survival benefit.

Les commentaires sont fermés.