12/04/2016
Plaies crâniennes: Un avenir est possible !
Long-term outcomes of combat casualties sustaining penetrating traumatic brain injury
Weisbrod AB et Al. J Trauma Acute Care Surg. 2012;73: 1525-1530
----------------------
Une prise en charge agressive globale des traumatismes cranio-cérébraux permet le retour à une indépendance fonctionnelle. Leur prise en charge doit donc être parfaite dès la prise en charge et la prévention des acsos un leitmotiv.
----------------------
BACKGROUND:
Previous studies have documented short-term functional outcomes for patients sustaining penetrating brain injuries (PBIs). However, little is known regarding the long-term functional outcome in this patient population. Therefore, we sought to describe the long-term functional outcomes of combat casualties sustaining PBI.
METHODS:
Prospective data were collected from 2,443 patients admitted to a single military institution during an 8-year period from 2003 to 2011. PBI was identified in 137 patients and constitute the study cohort. Patients were stratified by age, Injury Severity Score (ISS) and admission Glasgow Coma Scale (aGCS) score. Glasgow Outcome Scale (GOS) scores were calculated at discharge, 6 months, 1 year and 2 years. Patients with a GOS score of 4 or greater were considered to have attained functional independence (FI).
RESULTS:
The mean (SD) age of the cohort was 25 (7) years, mean (SD) ISS was 28 (9), and mean (SD) aGCS score was 8.8 (4.0). PBI mechanisms included gunshot wounds (31%) and blast injuries (69%). Invasive intracranial monitoring was used in 80% of patients, and 86.9% of the study cohort underwent neurosurgical intervention. Complications included cerebrospinal fluid leak (8.3%), venous thromboembolic events (15.3%), meningitis (24.8%), systemic infection (27.0%), and mortality (5.8%). The cohort was stratified by aGCS score and showed significant improvement in functional status when mean discharge GOS score was compared with mean GOS score at 2 years. For those with aGCS score of 3 to 5 (2.3 [0.9] vs. 2.9 [1.4], p G 0.01), 32% progressed to FI. For those with aGCS score of 6 to 8 (3.1 [0.7] vs. 4.0 [1.2], p G 0.0001), 63% progressed to FI. For those with aGCS score of 9 to 11 (3.3 [0.5] vs. 4.3 [0.8], p G 0.0001), 74% progressed to FI. For those with aGCS score of 12 to 15 (3.9 [0.7] vs. 4.8 [0.4], p G 0.00001), 100% progressed to FI.
CONCLUSION: Combat casualties with PBI demonstrated significant improvement in functional status up to 2 years from discharge, and a large proportion of patients sustaining severe PBI attained FI.
| Tags : crâne
Sauvetage au combat: Connaître et appliquer la procédure
Preventable deaths in trauma patients associated with non adherence to management guidelines
Marson CA et Al. Rev Bras Ter Intensiva. 2010; 22(3):220-228
------------------------------------------------------
Connaître, maîtriser chacune des composantes d'une procédure et les mettre en oeuvre est un facteur de survie des blessés. Le respect de la procédure du sauvetage au combat apparait fondamental. Il est nécessaire de le rappeler.
------------------------------------------------------
Objectives: To evaluate patients treated for traumatic injuries and to identify adherence to guidelines recommendations of treatment and association with death. The recommendations adopted were defined by the committee on trauma of the American College of Surgeons in advanced trauma life support.
Methods: Retrospective cohort study conducted at a teaching hospital. The study population was victims of trauma ≥ 12 years of age with injury severity scores ≥ 16 who were treated between January 1997 and December 2001. Data collection was divided into three phases: pre-hospital, in-hospital, and post-mortem. The data collected were analyzed using EPI INFO.
Results: We analyzed 207 patients, 147 blunt trauma victims (71%) and 60 (29%) penetrating trauma victims. Trauma victims had a 40.1% mortality rate. We identified 221 non adherence events that occurred in 137 patients. We found a mean of 1.61 non adherence per patient, and it occurred less frequently in survivors (1.4) than in non-survivors (1.9; p=0.033). According to the trauma score and injury severity score methodology, 54.2% of deaths were considered potentially preventable. Non adherence occurred 1.77 times more frequently in those considered potentially preventable deaths compared to other non-survivors (95% CI: 1.12–2.77; p=0.012), and 92.9% of the multiple non adherence occurred in the first group (p=0.029).
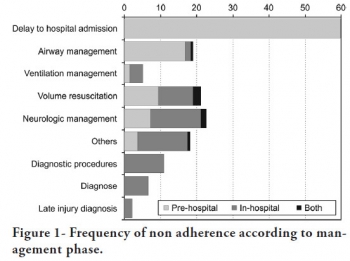
Conclusions: Non adherence occurred more frequently in patients with potentially preventable deaths. Non adherence to guidelines recommendations can be considered a contributing factor to death in trauma victims and can lead to an increase in the number of potentially preventable deaths.
| Tags : procedure evdg
11/04/2016
PROPPR Study: 1-1-2 aussi bien !
Damage-control resuscitation and emergency laparotomy: Findings from the PROPPR study
Undurraga VJ et AL. J Trauma Acute Care Surg. 2016 Apr;80(4):568-75
BACKGROUND:
The Pragmatic Randomized Optimal Platelet and Plasma Ratios (PROPPR) trial has demonstrated that damage-controlresuscitation, a massive transfusion strategy targeting a balanced delivery of plasma-platelet-red blood cell in a ratio of 1:1:1, results in improved survival at 3 hours and a reduction in deaths caused by exsanguination in the first 24 hours compared with a 1:1:2 ratio. In light of these findings, we hypothesized that patients receiving 1:1:1 ratio would have improved survival after emergency laparotomy.
METHODS:
Severely injured patients predicted to receive a massive transfusion admitted to 12 Level I North American trauma centers were randomized to 1:1:1 versus 1:1:2 as described in the PROPPR trial. From these patients, the subset that underwent an emergency laparotomy, defined previously in the literature as laparotomy within 90 minutes of arrival, were identified. We compared rates and timing of emergency laparotomyas well as postsurgical survival at 24 hours and 30 days.
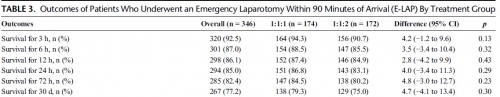
RESULTS:
Of the 680 enrolled patients, 613 underwent a surgical procedure, 397 underwent a laparotomy, and 346 underwent an emergency laparotomy. The percentages of patients undergoing emergency laparotomy were 51.5% (174 of 338) and 50.3% (172 of 342) for 1:1:1 and 1:1:2, respectively (p = 0.20). Median time to laparotomy was 28 minutes in both treatment groups. Among patients undergoing an emergency laparotomy, the proportions of patients surviving to 24 hours and 30 days were similar between treatment arms; 24-hour survival was 86.8% (151 of 174) for 1:1:1 and 83.1% (143 of 172) for 1:1:2 (p = 0.29), and 30-day survival was 79.3% (138 of 174) for 1:1:1 and 75.0% (129 of 172) for 1:1:2 (p = 0.30).
CONCLUSION:
We found no evidence that resuscitation strategy affects whether a patient requires an emergency laparotomy, time to laparotomy, or subsequent survival.
| Tags : coagulopathie, transfusion
07/04/2016
Brûlés: Moins grave qu'imaginé mais toujours spécifique
One year of burns at a Role 3 Medical Treatment Facility in Afghanistan
Jeevaratnam JA et Al. J R Army Med Corps. 2014 Mar;160(1):22-6
-------------------------------
L'expérience UK afghane confirme dans ce type de conflits la particularité des brûlures de guerre: Finalement peu fréquentes souvent isolées (72%), relativement peu étendues portant sur la face, associée à des brûlures respiratoires/inhalation de fumées (13%) et associés à d'autres lésions traumatiques (27%) qui peuvent être au premier plan. 6% sont intubés. Il n'en demeure pas moins que la chaîne de prise en charge se doit d'être spécifique avec le respect de délai de prise en charge en particulier du fait des techniques d'excision-greffe nécessaire et des besoins transfusionnels souvent importants.
-------------------------------
OBJECTIVES:
Historically, burns have formed a significant proportion of the casualties of war. The management of burns in recent conflict has been found to be a resource-heavy undertaking, though its impact on both personnel and resources in current conflicts is unclear. A case analysis has been carried out in order to quantify the logistical impact of the management of burns on Role 3 Medical Treatment Facility (MTF) infrastructure and to examine if and how the cause and management of burns have evolved in early 21st century conflict.
METHODS:
All casualties treated for burns at a Role 3 MTF over one calendar year were identified and scanned copies of their notes obtained from the UK Joint Theatre Trauma Registry and retrospectively analysed.
RESULTS:
88 of the 1461 (6.0%) trauma patients presenting to the Role 3 MTF over the year were treated for burns of whom 52.3% were combat troops and 45.4% civilians. Half of the burns were caused by non-conflict related mechanisms; the two commonest mechanisms were flame burns in 38/88 mostly non-conflict related cases and blast in 30/88 cases most of which were conflict related.

CONCLUSIONS:
The management of burns at war is a complex process. It is further confounded by the management of civilians with non-conflict related burns, which places a predictable strain on Role 3 MTF resources: theatre time, nursing time, dressing resources and bed space. This must be planned for in current and future deployed operations.
06/04/2016
Mèdecine de guerre: Histoire US
Treatment of War Wounds. A Historical Review
Clin Orthop Relat Res (2009) 467:2168–2191
The treatment of war wounds is an ancient art, constantly refined to reflect improvements in weapons technology, transportation, antiseptic practices, and surgical techniques. Throughout most of the history of warfare, more soldiers died from disease than combat wounds, and misconceptions
regarding the best timing and mode of treatment for injuries often resulted in more harm than good. Since the 19th century, mortality from war wounds steadily decreased as surgeons on all sides of conflicts developed systems for rapidly moving the wounded from the battlefield to frontline hospitals where surgical care is delivered. We review the most important trends in US and Western military trauma management over two centuries, including the shift from primary to delayed closure in wound management, refinement of amputation techniques, advances in evacuation philosophy and technology, the development of antiseptic practices, and the use of antibiotics.We also discuss how the lessons of history are reflected in contemporary US practices in Iraq and Afghanistan
05/04/2016
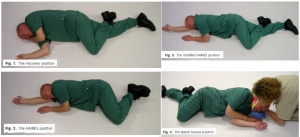
Immobiliser le rachis: Comme il faut !
Safety of the lateral trauma position in cervical spine injuries: a cadaver model study
Hyldmo PK et Al. Acta Anaesthesiol Scand. 2016 Mar 7. doi: 10.1111/aas.12714.
__________________________
Bien immobiliser un rachis avec la bonne position. Lire aussi 1, 2, 3
__________________________
| Tags : rachis
Victimes d'explosion: Pas de collier cervical
Cervical spine injuries in civilian victims of explosions: Should cervical collars be used?
Klein Y et Al. J Trauma Acute Care Surg. 2016 Mar 18. [Epub ahead of print]
---------------------------------------------------
En contexte de terrorisme civil, la pose d'un collier cervical apparaît plutôt inutile et source de perte de temps.
---------------------------------------------------
BACKGROUND:
Semi-rigid cervical collars (SRCC) are routinely applied to victims of explosions as part of the pre-hospital trauma protocols. Previous studies have shown that the use of SRCC in penetrating injuries is not justified due to the scarcity of unstable cervical spine injuries and the risk of obscuring other neck injuries. Explosion can inflict injuries by fragments penetration, blast injury, blunt force and burns. The study purpose was to determine the occurrence of cervical spine instability without irreversible neurological deficit and other potentially life threatening non-skeletal neck injuries among victims of explosions. The potential benefits and risks of SRCC application in explosion related injuries (ERI) was Evaluated.
METHODS:
a retrospective cohort study of all explosions civilian victims admitted to Israeli hospitals during the years 1998-2010. Data collection was based on the Israeli national trauma registry and the hospital records, and included demographic, clinical and radiological details of all patients with documented cervical spine injuries.
RESULTS:
the cohort included 2,267 patients. All of them were secondary to terrorist attacks. SRCC was applied to all the patients at the scene. Nineteen patients (0.83%) had cervical spine fractures. Nine patients (0.088%) had unstable cervical spine injury. All but one had irreversible neurological deficit on admission. 151 patients (6.6%) had potentially life threatening penetrating non-skeletal neck injuries.
CONCLUSIONS:
Unstable cervical spine injuries secondary to explosion are extremely rare. The majority of unstable cervical spine fractures were secondary to penetrating injuries, with irreversible neurological deficits on admission. The application of SRCC did not seem to be of any benefit in these patients and might pose a risk of obscuring other neck injuries. We recommend that SRCC will not be used in the pre-hospital management of victims of explosions.
LEVEL OF EVIDENCE:
Retrospective observational study, level III.
| Tags : immobilisation
