L'immobilisation du rachis sous le feu direct n'est pas recommandé par la procédure du sauvetage au combat. Cela ne veut pas dire qu'il ne faut jamais stabiliser un rachis. Les fractures du rachis sont relativement fréquentes chez le blessé par VBIED. Ce contexte est rarement celui d'une exposition des sauveteurs au feu direct de l'ennemi. Il est donc particulièrement important de bien faire, dans les programme de formation des personnels, entre la prise en charge d'un blessé dans le cadre de combat d'infanterie et de la prise en charge de blessés par balle ou éclats provenant de munition et celui de VBIED où en plus des projectiles interviennent les notions de projection éventuelles et d'exposition au blast.
C'est ce qu'exprime le document présenté, fruit de l'expérience canadienne qui rappelle la fréquence des lésions du rachis dans ce contexte et malheureusement l'insuffisance du recours à la stabilisation du rachis.
----------------------------
Spinal Injuries After Improvised Explosive Device Incidents: Implications for Tactical Combat Casualty Care
Comstock S et al. JTrauma. 2011;71:S413–S417
Background: Tactical Combat Casualty Care aims to treat preventable causes of death on the battlefield but deemphasizes the importance of spinal immobilization in the prehospital tactical setting. However, improvised explosive devices (IEDs) now cause the majority of injuries to Canadian Forces (CF) members serving in Afghanistan. We hypothesize that IEDs are more frequently associated with spinal injuries than non-IED injuries and that spinal precautions are not being routinely employed on the battlefield.
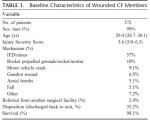
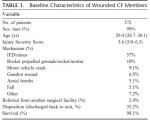
Methods: We examined retrospectively a database of all CF soldiers who were wounded and arrived alive at the Role 3 Multinational Medical Unit in Kandahar, Afghanistan, from February 7, 2006, to October 14, 2009. We collected data on demographics, injury mechanism, anatomic injury descriptions, physiologic data on presentation, and prehospital interventions performed. Outcomes were incidence of any spinal injuries.
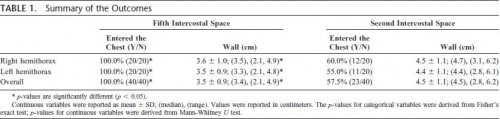
Results: Three hundred seventy-two CF soldiers were injured during the study period and met study criteria. Twenty-nine (8%) had spinal fractures identified. Of these, 41% (n = 12) were unstable, 31% (n = 9) stable, and 28% indeterminate. Most patients were injured by IEDs (n = 212, 57%). Patients injured by IEDs were more likely to have spinal injuries than those injured by non–IED-related mechanisms (10.4% vs. 2.3%; p < 0.01). IED victims were even more likely to have spinal injuries than patients suffering blunt trauma (10.4% vs. 6.7%; p = 0.02). Prehospital providers were less likely to immobilize the spine in IED victims compared with blunt trauma patients (10% [22 of 212] vs. 23.0% [17 of 74]; p < 0.05).

Conclusions: IEDs are a common cause of stable and unstable spinal injuries in the Afghanistan conflict. Spinal immobilization is an underutilized intervention in the battlefield care of casualties in the conflict in Afghanistan. This may be a result of tactical limitations; however, current protocols should continue to emphasize the judicious use of immobilization in these patients.