15/11/2011
Exsuflation par voie antérieure: Au 5ème axillaire plutôt qu'au 2ème antérieur?
Optimal Positioning for Emergent Needle Thoracostomy: A Cadaver-Based Study
Inaba K et all. J Trauma. 2011;71: 1099–1103
Un travail de plus sur la pertinence de la remise en cause de la recommandation d'aborder la paroi thoracique au 2ème espace intercostal sur la ligne médioclaviculaire. Ces repères sont en rapport avec une plus grande profondeur de l'espace pleural source d'échec de décompression pleurale lors d'exsufflation à l'aiguille. Certains proposent de réaliser cette dernière par voie latérale. Un travail de plus qui conforte cette approche.
-----------------------
Background: Needle thoracostomy is an emergent procedure designed to relieve tension pneumothorax. High failure rates because of the needle not penetrating into the thoracic cavity have been reported. Advanced Trauma Life Support guidelines recommend placement in the second intercostal space, midclavicular line using a 5-cm needle. The purpose of this study was to evaluate placement in the fifth intercostal space, midaxillary line, where tube thoracostomy is routinely performed. We hypothesized that this would result in a higher successful placement rate.
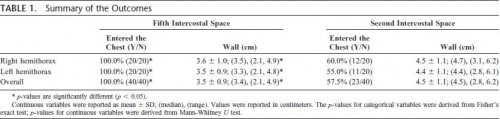
Methods: Twenty randomly selected unpreserved adult cadavers were evaluated. A standard 14-gauge 5-cm needle was placed in both the fifth intercostal space at the midaxillary line and the traditional second intercostal space at the midclavicular line in both the right and left chest walls. The needles were secured and thoracotomy was then performed to assess penetration into the pleural cavity. The right and left sides were analyzed separately acting as their own controls for a total of 80 needles inserted into 20 cadavers. The thickness of the chest wall at the site of penetration was then measured for each entry position.
Results: A total of 14 male and 6 female cadavers were studied. Overall, 100% (40 of 40) of needles placed in the fifth intercostal space and 57.5% (23 of 40) of the needles placed in the second intercostal space entered the chest cavity (p 0.001); right chest: 100% versus 60.0% (p 0.003) and left chest: 100% versus 55.0% (p 0.001). Overall, the thickness of the chest wall was 3.5 cm 0.9 cm at the fifth intercostal space and 4.5 cm 1.1 cm at the second intercostal space (p 0.001). Both right and left chest wall thicknesses were similar (right, 3.6 cm 1.0 cm vs. 4.5 cm 1.1 cm,p 0.007; left, 3.5 0.9 cm vs. 4.4 cm 1.1 cm, p 0.008).
Conclusion: In a cadaveric model, needle thoracostomy was successfully placed in 100% of attempts at the fifth intercostal space but in only 58% at the traditional second intercostal position. On average, the chest wall was 1 cm thinner at this position and may improve successful needle placement. Live patient validation of these results is warranted.

Les commentaires sont fermés.