17/01/2025
Du maintien des compétences: Un problème pour tous
Medical Training Falls Short at Army Combat Training Centers
Carius BM et Al. Military Medicine, Volume 190, Issue 1-2, January/February 2025, Pages 36–37
While combat arms project military strength and logistical support elements underwrite this power, medical support is vital for preservation of military life and readiness. We recently augmented different brigade rotations at an Army combat training center (CTC) as medical providers and find difficulty in confronting the depth and breadth of medical training inadequacies in support of this foundational training event. While we hope that our experiences are an aberrancy of isolated unit misfocus, the lack of medical training standards at Army CTCs demonstrates that rotational unit shortcomings are as much a byproduct of a systemic lack of medical training as individual organizations neglect. Despite coming from different backgrounds and experiences in medicine, the military, and CTC experience, we nevertheless came away with equally profound dismay at medical training shortfalls for both notional and real-world casualties.
As with most military forces, Army medics (medical occupational specialty 68W) are notably understrength and relatively inexperienced given exiting combat veterans and decreased deployments. Remaining medics disproportionately shoulder numerous administrative burdens, such as vehicle maintenance. This leaves little to no time to retain, refine, and practice basic skills initially taught in advanced individual training, let alone advance medical practices. Of dozens of medics we interacted with, all reported no substantial clinical opportunities to learn from direct supervision by a physician or physician assistant. Medics lacked essential pharmacotherapy understanding, including common medications like diphenhydramine and loperamide or emergent interventions such as epinephrine for anaphylaxis or pralidoxime for nerve agent exposure. The overwhelming majority acknowledged little clinical exposure beyond basic sick call. A small fraction of the few with combat experience expressed confidence with trauma management.
01/12/2022
Facteurs humains en situations critiques
08/06/2022
Trauma Prehospitalier: Aides
| Tags : traumatologie
19/12/2021
Ouvrir un cou: Ne s'invente pas !
Effectiveness of a simulation-based mastery learning to train clinicians on a novel cricothyrotomy procedure at an academic medical centre during a pandemic: a quasi-experimental cohort study
Nabil Issa N et Al. BMJ Open. 2021 Nov 19;11(11):e054746. doi: 10.1136/bmjopen-2021-054746.
Objectives: To develop and evaluate a simulation-based mastery learning (SBML) curriculum for cricothyrotomy using wet towels to suppress aerosolisation during a pandemic.
Design: Quasi-experimental, pre-post study.
Setting: Tertiary care, academic medical centre in Chicago.
Participants: Ear, nose and throat and general surgery residents, fellows and attendings.
Intervention: Cricothyroidotomy simulation-based mastery learning curriculum.
Outcomes measure: Pretest to posttest simulated cricothyrotomy skills checklist performance.
Results: 37 of 41 eligible surgeons participated in the curriculum. Median pretest score was 72.5 (IQR 55.0-80.0) and 100.0 (IQR 98.8-100.0) for the posttest p<0.001.

All participants scored at or above a minimum passing standard (93% checklist items correct) at posttest.
Conclusions: Using SBML is effective to quickly train clinicians to competently perform simulated cricothyrotomy during a pandemic.
06/04/2021
Inexpérimenté mais sûr de soi ! Constat alarmant
Inexperienced but Confident: A Survey of Advanced Life Support Providers and Life-saving Interventions in the Israel Defense Forces
Haddad N et Al. Military Medicine, Volume 186, Issue Supplement_1, January-February 2021,
----------------------------------------------------
Suivre une formation ne veut pas dire savoir faire. Il est impératif de VÉRIFIER le savoir faire
----------------------------------------------------
Objective:
The objective of this study was to assess the current experience of Israel Defense Forces' (IDF) advanced life support (ALS) providers in performing life-saving interventions (LSIs), the rate of doctors and paramedics achieving the Trauma and Combat Medicine Branch benchmarks, and the rate of providers feeling confident in performing the interventions although not achieving the benchmarks.
Methods:
This study was based on an online survey delivered to IDF ALS providers. The survey investigated demographics; experience in performing endotracheal intubation, cricothyroidotomy, tube thoracostomy, and intraosseous access on human patients; and confidence in performing these LSIs. All benchmarks chosen referred to the number of times performed in the previous year. The benchmarks were 20 for intubation, 3 for cricothyroidotomy, 4 for tube thoracostomy, and 3 for intraosseous access.
Results:
During the survey period, 175 IDF ALS providers started the survey, but only 138 (79%) completed it, 93 (67%) of them were paramedics. Doctors had higher rates than paramedics of failing to achieve the benchmarks for intubation (96 vs. 57%, P < .001) and intraosseous access (100 vs. 66%, P < .001). All respondents failed to achieve the benchmark for cricothyroidotomy, and all but one paramedic failed to achieve the tube thoracostomy benchmark. Doctors had lower rates of high confidence when failing to achieve the benchmark for intubation (35 vs. 64%, P = .008) and intraosseous access (7 vs. 31%, P = .005) compared to paramedics.
Conclusion:
IDF ALS providers have alarmingly limited experience in performing LSIs. Many of them are confident in their ability despite not achieving evidence-based benchmarks. Additional training is required, maybe as a part of an annual medical fitness test.
01/10/2019
Préparation mentale: Soyez pratiquants +++
Mental Skills in Surgery: Lessons Learned from Virtuosos, Olympians, and Navy Seals.
----------------------------------------
Les techniques de préparation mentale ont fait leurs preuves dans le domaine du sport. Elles commencent à être utilisées dans le domaine médical ET CELA MARCHE. Le document proposé fait le point sur son intérêt.
----------------------------------------
OBJECTIVE:
The present study investigated the role of mental skills in surgery through the unique lens of current surgeons who had previously served as Olympic athletes, elite musicians, or expert military personnel.
BACKGROUND:
Recent work has demonstrated great potential for mental skills training in surgery. However, as a field, we lag far behind other high-performance domains that explicitly train and practice mental skills to promote optimal performance. Surgery stands to benefit from this work. First, there is a need to identify which mental skills might be most useful in surgery and how they might be best employed.
METHODS:
Using a constructivist grounded theory approach, semi-structured interviews were conducted with 17 surgeons across the United States and Canada who had previously performed at an elite level in sport, music, or the military.
RESULTS:
Mental skills were used both to optimize performance in the moment and longitudinally. In the moment, skills were used proactively to enter an ideal performance state, and responsively to address unwanted thoughts or emotions to re-enter an acceptable performance zone. Longitudinally, participants used skills to build expertise and maintain wellness.
CONCLUSIONS:
Establishing a taxonomy for mental skills in surgery may help in the development of robust mental skills training programs to promote optimal surgeon wellness and performance.
26/07/2019
Maîtriser l'intubation: Un vrai challenge
Procedural Experience With Intubation: Results From a National Emergency Medicine Group.
---------------------------------
Un geste à laquelle les médecins urgentistes US sont peu exposés dans leur pratique quotidienne. Un vrai challenge personnel et pour les formateurs notamment des centres de simulations.
---------------------------------
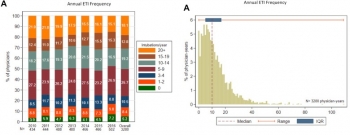
STUDY OBJECTIVE:
Although intubation is a commonly discussed procedure in emergency medicine, the number of opportunities for emergency physicians to perform it is unknown. We determine the frequency of intubation performed by emergency physicians in a national emergency medicine group.
METHODS:
Using data from a national emergency medicine group (135 emergency departments [EDs] in 19 states, 2010 to 2016), we determined intubation incidence per physician, including intubations per year, intubations per 100 clinical hours, and intubations per 1,000 ED patient visits. We report medians and interquartile ranges (IQRs) for estimated intubation rates among emergency physicians working in general EDs (those treating mixed adult and pediatric populations).
RESULTS:
We analyzed 53,904 intubations performed by 2,108 emergency physicians in general EDs (53,265 intubations) and pediatric EDs (639 intubations). Intubation incidence varied among general ED emergency physicians (median 10 intubations per year; IQR 5 to 17; minimum 0, maximum 109). Approximately 5% of emergency physicians did not perform any intubations in a given year. During the study, 24.1% of general ED emergency physicians performed fewer than 5 intubations per year (range 21.2% in 2010 to 25.7% in 2016).
Emergency physicians working in general EDs performed a median of 0.7 intubations per 100 clinical hours (IQR 0.3 to 1.1) and 2.7 intubations per 1,000 ED patient visits (IQR 1.2 to 4.6).
CONCLUSION:
These findings provide insights into the frequency with which emergency physicians perform intubations.
16/07/2019
Always Ready; Responding to an Emergency at Sea
Always Ready; Responding to an Emergency at Sea
I’m surrounded by the lush jungle of Okinawa on a muggy day,
The warm glow of the sun on my face brings me to life.
The alarm screeches overhead jarring me out of my reverie.
“Attention in the medical bay. This is not a drill.”
An airplane is in the water. Casualties inbound,
The medical bay of the aircraft carrier is abuzz with anticipation.
Drill after drill--for this.
Years of study and experience come down to this one moment.
Medical school;
Field trauma training;
Internship;
Aviation medicine;
Are you ready? Is your team ready? Could you have done more?
We are prepared. We are ready!
Eyes are on you, “Sir, what do we do?”
What do we know? What happened? Who’s involved? Where are they?
Details are scarce.
Take a breath…think…remember your training.
---ABCDE.
Airway, breathing, circulation, disability, environment;
The mantra marches to the forefront of my thoughts like an eager Marine.
Assign roles, prepare the equipment,
New information, the two pilots are my friends.
Only one is recovered. Push the sorrow to the rear. Three minutes out.
We are ready.
The whirling rotors are deafening as we unload the patient,
We move by instinct thanks to constant drilling,
Next thing I know we are in Trauma One.
He has one question, “The crew, are they safe?”
Airway is clear, he is breathing and ventilating. Brain is perfused.
Primary survey; distal femur and posterior hip are shattered,
Our team of nurses, corpsmen, and doctors take to their assigned roles,
We splint the femur and bind the hip.
Medical management with morphine, normal saline, and antibiotics.
A job well done; he is going to be okay.
We medevac him via helicopter to Roll 3 ashore,
His parting words. “Any updates on the crew?”
I tell him answers will come, but I know in my heart the truth.
He is in the water…Our brother is dead.
How do you prepare for that?
08/04/2019
Simulation: Pas que le sauvetage au combat
Simulation Training for Operational Medicine Providers (STOMP): Impact of a Comprehensive Skills-Based Curriculum for Military General Medical Officers
Spooner MT et Al. Mil Med. 2018 Dec 4. doi: 10.1093/milmed/usy346
-----------------------------------------------
Nos camarades US ont identifié 22 gestes qu'ils considèrent comme devoir être acquis par leur médecins généralistes. Ce travail démontre l'apport de la simulation pour l'apprentissage de ce geste et milite pour un curriculum basé sur la maîtrise de gestes choisis.
-----------------------------------------------
A standardized training curriculum designed for general medical officers (GMO) titled Simulation Training for Operational Medicine Providers (STOMP) was recently developed to educate and improve GMOs’ procedural skills through directed feedback prior to assuming duties in an operational environment. This study aimed to determine the impact this novel curriculum had on GMOs’confidence levels in 21 core privileges covering eight different subspecialties while stationed at Naval Medical Center Portsmouth (NMCP).
A cohort study from 2015 to 2017 was designed to address our specific aim to examine if the implementation of the STOMP curriculum increased GMOs’ confidence levels. Fifty-seven participants enrolled in the study. The GMO case group completed the STOMP curriculum (n = 22), while the control or GMO self-study group (n = 35) did not complete the curriculum. Six months after starting clinical practice at NMCP, both groups completed an online survey that assessed their confidence level in performing each core privilege using a 5-point Likert scale. Scores were analyzed using a Wilcoxon Mann–Whitney test. Research data were derived from an approved Naval Medical Center, Portsmouth, Virginia IRB, protocol number: NMCP.2016.0010.
Participants demonstrated a statistically significant increase in self-rated confidence scores (p < 0.05) in nine core privilege skills: punch biopsy, shave biopsy, excisional biopsy, removal of otic foreign body, removal of nasal foreign body, removal of ocular foreign body, tonometry, incision and drainage of a thrombosed hemorrhoid, and reduction of simple closed fractures and dislocations.

These findings suggest that a novel and recently developed standardized simulation training curriculum entitled STOMP improves the confidence levels of early career physicians’ in several primary care procedural skills and is an ideal adjunct to traditional lecture-based teaching prior to independent practice in a primary care environment.
19/03/2019
Trauma et formation: Progrès encore à faire
Surgical interns in 2018: Objective assessment suggests they are better but still lack critical knowledge and skill.
BACKGROUND:
The transition from fourth-year medical student to surgical intern is difficult. A lack of repetitions, experience, and knowledge is problematic. We report our experience using simulation-based technical and nontechnical skills to assess the competency of surgical interns in July and January of their intern year.
DESIGN:
As part of a larger assessment effort, our general surgery interns (2010-2016) have been tested on performing an emergent cricothyrotomy, interpreting 2 arterial blood gases, and reading 3 chest x-rays in fewer than 7 minutes. We retrospectively analyzed general surgery interns' performance on these 3 tests (total score = 20).
RESULTS:
A total of 210 interns completed both July and January (identical) assessments. Overall mean scores improved from July (12.62 ± 3.44) to January (16.5 ± 2.46; P < .05). During the study period general surgery interns' mean baseline scores improved in both July (P < .05) and in January (P < .05). Although most individual general surgery interns did improve their total scores (92% improved, 3% same, 5% worse) between July and January (P < .05), in January 40% could not perform an emergent cricothyrotomy swiftly, and 6% missed a tension pneumothorax on chest x-ray.
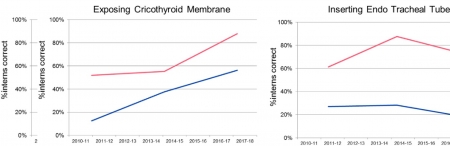
CONCLUSION:
Our data suggest that surgical interns start residency training with low levels of skill and comprehension with emergent cricothyrotomy, arterial blood gas, and chest x-ray. They improve with 6 months of clinical and simulation training. Encouragingly, overall scores for both July and January assessments have improved during the study period. Given that some interns still struggle in January to perform these three tasks, we believe that 2018 interns are better, but still potentially lack critical knowledge and skill.
16/03/2019
Reco Simulation
07/12/2018
Zone de confort: En sortir pour progresser ?
Biological Response to Stress During Battlefield Trauma Training: Live Tissue Versus High-Fidelity Patient Simulator.
INTRODUCTION:
Tactical Combat Casualty Care (TCCC) training imposes psychophysiological stress on medics. It is unclear whether these stress levels vary with the training modalities selected. It is also unclear how stress levels could have an impact on medical performance and skill uptake.
MATERIALS AND METHODS:
We conducted a pilot study to compare the effects of live tissue (LT) with a high-fidelity patient simulator (SIM) on the level of stress elicited, performance, and skill uptake during battlefield trauma training course in an operating room (OR) and in a simulated battlefield scenario (field). In the report, we studied the effects of training modalities and their changes on stress levels by measuring different biomarkers (salivary amylase, plasma catecholamines, and neuropeptide Y) at various time points during the trauma training course.
RESULTS:
We found that the training resulted in significant psychophysiological stress as indicated by elevated levels of various biomarkers relative to baseline immediately after both OR and field assessment (p < 0.05). Compared with pre-OR levels, the LT training in the OR resulted in significant increases in the plasma levels of epinephrine, norepinephrine, and neuropeptide (p = 0.013, 0.023, 0.004, respectively), whereas the SIM training in the OR resulted in significant increases in the plasma levels of norepinephrine and neuropeptide (p = 0.003 and 0.008). Compared with pre-field levels, we found significant increases in plasma epinephrine concentration in the SIM group (p = 0.016), plasma norepinephrine concentration in the LT group (p = 0.015), and plasma neuropeptide Y concentration in both LT (p = 0.006) and SIM groups (p = 0.029). No differences in the changes of biomarker levels were found between LT and SIM groups in the OR and field. Compared with pre-field levels, the testing on the same modality as that in the OR in the simulated battlefield resulted in significant increases in norepinephrine and neuropeptide levels (p = 0.013 and 0.015), whereas the testing on different modalities resulted in significant increases in amylase, epinephrine, and neuropeptide levels (p = 0.016, 0.05, 0.018, respectively). There was a significantly larger increase in plasma norepinephrine concentration (p = 0.031) and a trend toward a greater increase in the salivary amylase level (p = 0.052) when the field testing involved a different modality than the OR compared with when OR and field testing involved the same modality. Although most of the biomarkers returned to baseline levels after 24 h, plasma norepinephrine levels remained significantly higher regardless of whether field testing occurred on the same or different modality compared with OR (p = 0.040 and 0.002).
CONCLUSION:
TCCC training led to significant increase in psychophysiological stress, as indicated by elevated levels of various biomarkers. The training modalities did not result in any differences in stress levels, whereas the switch in training modalities appeared to elicit greater stress as evidenced by changes in specific biomarkers (amylase and norepinephrine). A comparative study with a larger sample size is warranted.
16/09/2018
Airway, pour être au RDV: S'entraîner
A Continuous Quality Improvement Airway Program Results in Sustained Increases in Intubation Success.
INTRODUCTION:
Airway management is a critical skill for air medical providers, including the use of rapid sequence intubation (RSI) medications. Mediocre success rates and a high incidence of complications has challenged air medical providers to improve training and performance improvement efforts to improve clinical performance.
OBJECTIVES:
The aim of this research was to describe the experience with a novel, integrated advanced airway management program across a large air medical company and explore the impact of the program on improvement in RSI success.
METHODS:
The Helicopter Advanced Resuscitation Training (HeART) program was implemented across 160 bases in 2015. The HeART program includes a novel conceptual framework based on thorough understanding of physiology, critical thinking using a novel algorithm, difficult airway predictive tools, training in the optimal use of specific airway techniques and devices, and integrated performance improvement efforts to address opportunities for improvement. The C-MAC video/direct laryngoscope and high-fidelity human patient simulation laboratories were implemented during the study period. Chi-square test for trend was used to evaluate for improvements in airway management and RSI success (overall intubation success, first-attempt success, first-attempt success without desaturation) over the 25-month study period following HeART implementation.
RESULTS:
A total of 5,132 patients underwent RSI during the study period. Improvements in first-attempt intubation success (85% to 95%, p < 0.01) and first-attempt success without desaturation (84% to 94%, p < 0.01) were observed. Overall intubation success increased from 95% to 99% over the study period, but the trend was not statistically significant (p = 0.311).
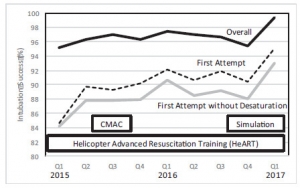
CONCLUSIONS:
An integrated advanced airway management program was successful in improving RSI intubation performance in a large air medical company.
| Tags : airway
08/09/2018
Le TCCC dans la vraie vie
Survey of Casualty Evacuation Missions Conducted by the 160th Special Operations Aviation Regiment During the Afghanistan Conflict.
BACKGROUND:
Historically, documentation of prehospital combat casualty care has been relatively nonexistent. Without documentation, performance improvement of prehospital care and evacuation through data collection, consolidation, and scientific analyses cannot be adequately accomplished. During recent conflicts, prehospital documentation has received increased attention for point-of-injury care as well as for care provided en route on medical evacuation platforms. However, documentation on casualty evacuation (CASEVAC) platforms is still lacking. Thus, a CASEVAC dataset was developed and maintained by the 160th Special Operations Aviation Regiment (SOAR), a nonmedical, rotary-wing aviation unit, to evaluate and review CASEVAC missions conducted by their organization.
METHODS:
A retrospective review and descriptive analysis were performed on data from all documented CASEVAC missions conducted in Afghanistan by the 160th SOAR from January 2008 to May 2015. Documentation of care was originally performed in a narrative after-action review (AAR) format. Unclassified, nonpersonally identifiable data were extracted and transferred from these AARs into a database for detailed analysis. Data points included demographics, flight time, provider number and type, injury and outcome details, and medical interventions provided by ground forces and CASEVAC personnel.
RESULTS:
There were 227 patients transported during 129 CASEVAC missions conducted by the 160th SOAR. Three patients had unavailable data, four had unknown injuries or illnesses, and eight were military working dogs. Remaining were 207 trauma casualties (96%) and five medical patients (2%). The mean and median times of flight from the injury scene to hospital arrival were less than 20 minutes. Of trauma casualties, most were male US and coalition forces (n = 178; 86%). From this population, injuries to the extremities (n = 139; 67%) were seen most commonly. The primary mechanisms of injury were gunshot wound (n = 89; 43%) and blast injury (n = 82; 40%). The survival rate was 85% (n = 176) for those who incurred trauma. Of those who did not survive, most died before reaching surgical care (26 of 31; 84%).
CONCLUSION:
Performance improvement efforts directed toward prehospital combat casualty care can ameliorate survival on the battlefield. Because documentation of care is essential for conducting performance improvement, medical and nonmedical units must dedicate time and efforts accordingly. Capturing and analyzing data from combat missions can help refine tactics, techniques, and procedures and more accurately define wartime personnel, training, and equipment requirements. This study is an example of how performance improvement can be initiated by a nonmedical unit conducting CASEVAC missions.
21/12/2017
Préparateur sportif et trauma sévère: Une évidence !
Cocks M et Al. J Surg Educ. 2014 Mar-Apr;71(2):262-9
BACKGROUND:
Mental practice has been successfully applied in professional sports for skills acquisition and performance enhancement. The goals of this review are to describe the literature on mental practice within sport psychology and surgery and to explore how the specific principles of mental practice can be applied to the improvement of surgical performance-both in novice and expert surgeons.
METHOD:
The authors reviewed the sports psychology, education, and surgery literatures through Medline, PubMed, PsycINFO, and Embase.
RESULTS:
In sports, mental practice is a valuable tool for optimizing existing motor skill sets once core competencies have been mastered. These techniques have been shown to be more advantageous when used by elite athletes. Within surgery, mental practice studies have focused on skill acquisition among novices with little study of how expert surgeons use it to optimize surgical preparation.
CONCLUSIONS:
We propose that performance optimization and skills acquisition should be viewed as 2 separate domains of mentalpractice. Further understanding of this phenomenon has implications for changing how we teach and train not only novice surgeons but also how experienced surgeons continue to maintain their skills, acquire new ones, and excel in surgery.
| Tags : top
10/11/2017
Formation des personnels des FS: Réflexions OTAN
21/10/2017
Serious game ? Peut-être mais pas sûr
- ---------------------------------------------------
AIM:
In modern warfare, almost 25% of combat-related deaths are considered preventable if life-saving interventions are performed. Therefore, Tactical Combat Casualty Care (TCCC) training for soldiers is a major challenge. In 2014, the French Military Medical Service supported the development of 3D-SC1®, a serious game designed for the French TCCC program, entitled Sauvetage au Combat de niveau 1 (SC1). Our study aimed to evaluate the impact on performance of additional training with 3D-SC1®.
MATERIAL AND METHODS:
The study assessed the performance of soldiers randomly assigned to one of two groups, before (measure 1) and after (measure 2) receiving additional training. This training involved either 3D-SC1® (Intervention group), or a DVD (Control group). The principal measure was the individual performance (on a 16-point scale), assessed by two investigators during a hands-on simulation. First, the mean performance score was compared between the two measures for Intervention and Control groups using a two-tailed paired t-test. Second, a multivariable linear regression was used to determine the difference in the impacts of 3D-SC1® and DVD training, and the order of presentation of the two scenarios, on the mean change from baseline in performance scores.
RESULTS AND DISCUSSION:
A total of 96 subjects were evaluated: seven could not be followed-up, while 50 were randomly allocated to the Intervention group, and 39 to the Control group. Between measure 1 and measure 2, the mean (SD) performance score increased from 9.9 (3.13) to 14.1 (1.23), and from 9.4 (2.97) to 12.5 (1.83), for the Intervention group and Control group, respectively (p<0.0001). The adjusted mean difference in performance scores between 3D-SC1® and DVD training was 1.1 (95% confidence interval -0.3, 2.5) (p=0.14). Overall, the study found that supplementing SC1 training with either 3D-SC1® or DVD improved performance, assessed by a hands-on simulation. However, our analysis did not find a statistically significant difference between the effects of these two training tools. 3D-SC1® could be an efficient and pedagogical tool to train soldiers in life-saving interventions. In the current context of terrorist threat, a specifically-adapted version of 3D-SC1®may be a cost-effective and engaging way to train a large civilian public.
09/08/2017
Un grimé comme assistant pédagogique
Conveying practical clinical skills with the help of teaching associates-a randomised trial with focus on the long term learning retention
Hoefer SH et Al. BMC Med Educ. 2017; 17: 65.
BACKGROUND:
Ensuring that all medical students achieve adequate clinical skills remains a challenge, yet the correct performance of clinical skills is critical for all fields of medicine. This study analyzes the influence of receiving feedback by teaching associates in the context of achieving and maintaining a level of expertise in complex head and skull examination.
METHODS:
All third year students at a German university who completed the obligatory surgical skills lab training and surgical clerkship participated in this study. The students were randomized into two groups.
CONTROL GROUP:
lessons by an instructor and peer-based practical skills training. Intervention group: training by teaching associates who are examined as simulation patients and provided direct feedback on student performance. Their competency in short- and long-term competence (directly after intervention and at 4 months after the training) of head and skull examination was measured. Statistical analyses were performed using SPSS Statistics version 19 (IBM, Armonk, USA). Parametric and non-parametric test methods were applied. As a measurement of correlation, Pearson correlations and correlations via Kendall's-Tau-b were calculated and Cohen's d effect size was calculated.
RESULTS:
A total of 181 students were included (90 intervention, 91 control). Out of those 181 students 81 agreed to be videotaped (32 in the control group and 49 in the TA group) and examined at time point 1. At both time points, the intervention group performed the examination significantly better (time point 1, p = <.001; time point 2 (rater 1 p = .009, rater 2 p = .015), than the control group. The effect size (Cohens d) was up to 1.422.
CONCLUSIONS:
The use of teaching associates for teaching complex practical skills is effective for short- and long-term retention. We anticipate the method could be easily translated to nearly every patient-based clinical skill, particularly with regards to a competence-based education of future doctors.
17/02/2017
Visualisation mentale: Mieux que l'ATLS
Lorello GR et Al CJEM. 2016 Mar;18(2):136-42. doi: 10.1017/cem.2015.4. Epub 2015 Apr 10.
--------------------------------
l'ATLS (Advanced trauma life support) est souvent présenté comme la panacée en matière de prise en charge du traumatisé. Il n'est pas inintéressant d'avoir une analyse très critique de ce type de formation dont le but originel était d'apporter, en 2 jours et demi, des connaissances de base à des équipes peu formées à la pris en charge de traumatisés sévères. Aussi doit on considérer qu'elle a été d'un apport fondamental dans les pays ne disposant pas de réseaux avancés. Si le contenu structuré et le recours à des ateliers pratiques apparaît attrayant , le contenu médical est régulièrement non conforme aux bonnes pratiques et les enseignants souvent non experts du sujet (1, 2). Il a pu être proposé de traduire l'acronyme ATLS par "Archaic Trauma Life Support"(3). Le travail proposé confirme bien les limites de cette formation qui ne parait plus adapté au contexte actuel pour des professionnels de l'affaire (4). Quand on s'adresse à des étudiants avancés dans leur cursus de formation, la préparation d'un exercice de simulation en équipe par l'imagerie mentale est plus efficace.
L'ATLS demeure néanmoins un bon moyen d'appréhender pour les novices les bases fondamentales de la prise en charge des traumatisés. Ce n'est pas le seul et il existe d'autres approches notamment le DIU de traumatisés sévères (5) ou l'European Trauma Course (6), dernier donnant un grande place à la simulation.
INTRODUCTION:
Effective trauma resuscitation requires the coordinated efforts of an interdisciplinary team. Mental practice (MP) is defined as the mental rehearsal of activity in the absence of gross muscular movements and has been demonstrated to enhance acquiring technical and procedural skills. The role of MP to promote nontechnical, team-based skills for trauma has yet to be investigated.
METHODS:
We randomized anaesthesiology, emergency medicine, and surgery residents to two-member teams randomly assigned to either an MP or control group. The MP group engaged in 20 minutes of MP, and the control group received 20 minutes of Advanced Trauma Life Support (ATLS) training. All teams then participated in a high-fidelity simulated adult trauma resuscitation and received debriefing on communication, leadership, and teamwork. Two blinded raters independently scored video recordings of the simulated resuscitations using the Mayo High Performance Teamwork Scale (MHPTS), a validated team-based behavioural rating scale. The Mann-Whitney U-test was used to assess for between-group differences.
RESULTS:
Seventy-eight residents provided informed written consent and were recruited. The MP group outperformed the control group with significant effect on teamwork behaviour as assessed using the MHPTS: r=0.67, p<0.01.
CONCLUSIONS:
MP leads to improvement in team-based skills compared to traditional simulation-based trauma instruction. We feel that MP may be a useful and inexpensive tool for improving nontechnical skills instruction effectiveness for team-based trauma care.
| Tags : top
03/12/2016
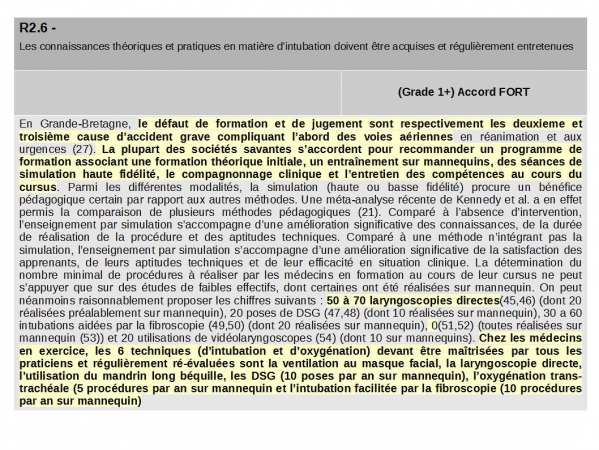
Voies aériennes: Objectifs de formation CHIFFRE
A n'en pas douter: Il faut un minimum de pratique pour pouvoir prétendre jouer un rôle. Le caractère obligatoire de quotas de geste est en route.
Clic sur l'image pour accéder à la RFE