19/07/2020
Vers une nouvelle TIC ?

14/10/2019
Pansements compressifs: Le test de la NAMRU
Pas nouveau mais instructif dans le contexte de bataille commerciale entre les industriels
28/07/2019
SAM JT extender:Pourles plaies axillaires
18/07/2019
Easywarm: Une autre couverture chauffante
Miniaturisation: La précision n'est pas au rendez-vous !
-----------------------------------
L'engouement pour la miniaturiation des équipements (PSE, Laryngoscope, Echographe) est grand. Encore faut il que la performance soit au rendez-vous. Ce n'est pas tout à fait le cas avec certains pousse-seringues, notamment en altitude. Ceci est très dommageable dès lors de la mise en oeuvre de perfusion d"amines pressives.
-----------------------------------
BACKGROUND:
Intravenous drug infusions in critically ill patients require accurate syringe infusion pumps (SIPs). This is particularly important during transportation of critically ill patients by helicopter emergency medical services (HEMS), where altitude may influence device performance. Because weight is a real concern in HEMS, new low-weight devices are very appealing. The aim of this study was to compare infusion flow rates delivered by low-weight versus standard SIP devices, in the prehospital emergency medicine setting, at different altitudes.
METHODS:
We conducted a comparative bench study involving five SIP devices (two standard and three low-weight models) at 300, 1700 and 3000 m altitude. The primary endpoint was the flow rate delivered by SIPs for prespecified values. We used two methods to measure flow. The normative method consisted in measuring weight (method A) and the alternate method consisted in measuring instantaneous flow (method B).
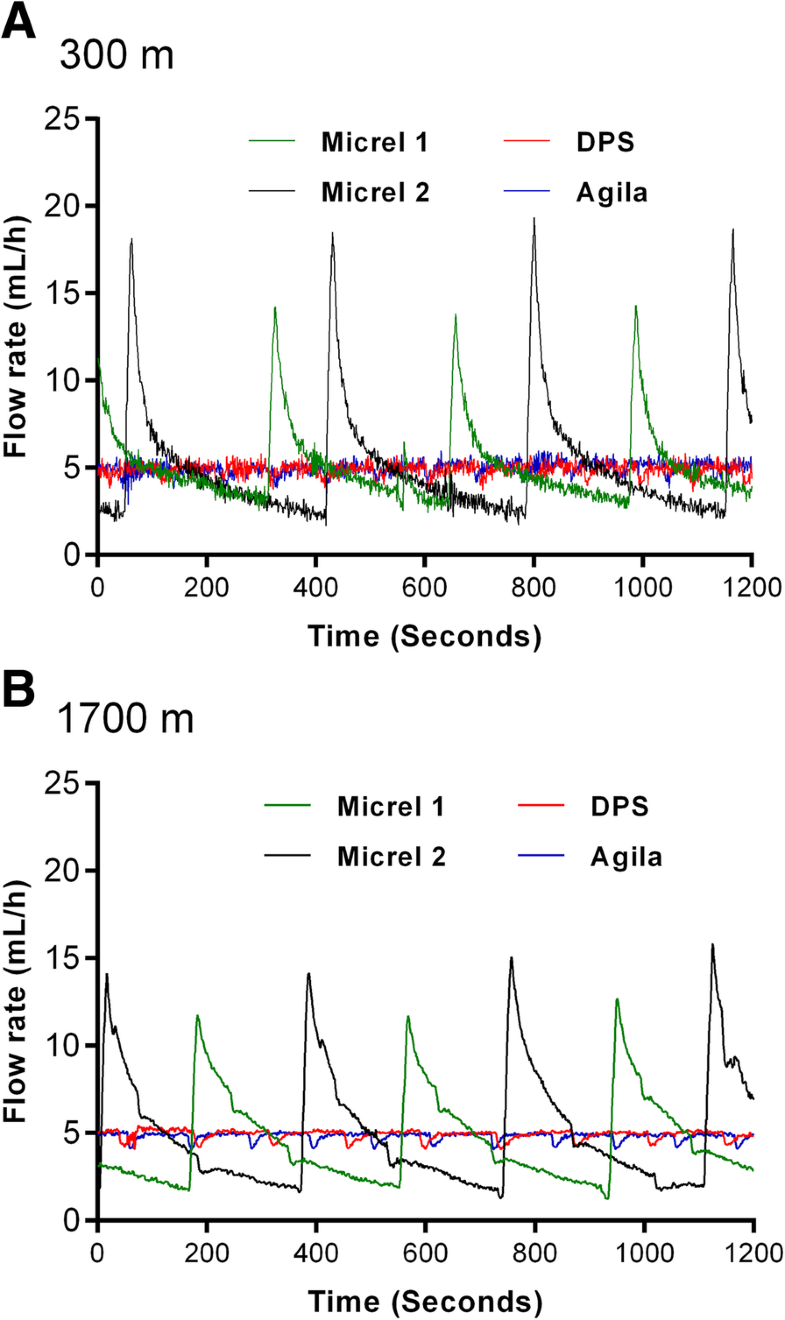
RESULTS:
Using method A, no significant differences were found in median flow rates and interquartile range depending on device and altitude for a prespecified 10-mL/h flow. However, method B showed that low-weight SIPs delivered multiple sequential boluses with substantial variations (1.2-15.8 mL/h) rather than a prespecified continuous 5-mL/h flow. At 1700 m altitude, the interquartile range of delivered flows increased only for low-weight devices (p for interaction< 0.001).
CONCLUSIONS:
Despite satisfactory normative tests, low-weight SIPs deliver discontinuous flow with potential clinical implications for critically ill patients receiving vasoactive drugs. This study also highlights a thus far unknown negative impact of altitude on SIP function. We believe that normative requirements for SIP approval should be revised accordingly.
16/05/2019
PST hémostatiques: Equivalents mais bases scientifiques pauvres
Systematic review of prehospital haemostatic dressings.
INTRODUCTION:
Haemorrhage is one of the leading causes of battlefield and prehospital death. Haemostatic dressings are an effective method of limiting the extent of bleeding and are used by military forces extensively. A systematic review was conducted with the aim of collating the evidence on current haemostatic products and to assess whether one product was more effective than others.
METHODS:
A systematic search and assessment of the literature was conducted using 13 health research databases including MEDLINE and CINAHL, and a grey literature search. Two assessors independently screened the studies for eligibility and quality. English language studies using current-generation haemostatic dressings were included. Surgical studies, studies that did not include survival, initial haemostasis or rebleeding and those investigating products without prehospital potential were excluded.
RESULTS:
232 studies were initially found and, after applying exclusion criteria, 42 were included in the review. These studies included 31 animal studies and 11 clinical studies. The outcomes assessed were subject survival, initial haemostasis and rebleeding. A number of products were shown to be effective in stopping haemorrhage, with Celox, QuikClot Combat Gauze and HemCon being the most commonly used, and with no demonstrable difference in effectiveness.
CONCLUSIONS:
There was a lack of high-quality clinical evidence with the majority of studies being conducted using a swine haemorrhage model. Iterations of three haemostatic dressings, Celox, HemCon and QuikClot, dominated the studies, probably because of their use by international military forces and all were shown to be effective in the arrest of haemorrhage.
12/05/2019
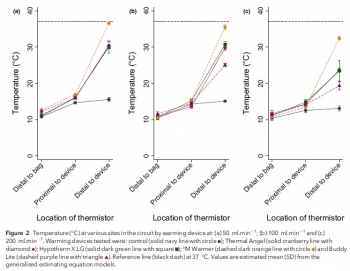
Réchauffeur: M Warmer, the best ?
Comparison of portable blood-warming devices under simulated pre-hospital conditions: a randomised in-vitro blood circuit study.
---------------------------------------------
Lire aussi cet article qui met en avant la performance du Qiflow warmer
---------------------------------------------
Pre-hospital transfusion of blood products is a vital component of many advanced pre-hospital systems. Portable fluid warmers may be utilised to help prevent hypothermia, but the limits defined by manufacturers often do not reflect their clinical use. The primary aim of this randomised in-vitro study was to assess the warming performance of four portable blood warming devices (Thermal Angel, Hypotherm X LG, °M Warmer, Buddy Lite) against control at different clinically-relevant flow rates. The secondary aim was to assess haemolysis rates between devices at different flow rates. We assessed each of the four devices and the control, at flow rates of 50 ml.min-1 , 100 ml.min-1 and 200 ml.min-1 , using a controlled perfusion circuit with multisite temperature monitoring. Free haemoglobin concentration, a marker of haemolysis, was measured at multiple points during each initial study run with spectrophotometry. At all flow rates, the four devices provided superior warming performance compared with the control (p < 0.001). Only the °M Warmer provided a substantial change in temperature at all flow rates (mean (95%CI) temperature change of 21.1 (19.8-22.4) °C, 20.4 (19.1-21.8) °C and 19.4 (17.7-21.1) °C at 50 ml.min-1 , 100 ml.min-1 and 200 ml.min-1 , respectively).
There was no association between warming and haemolysis with any device (p = 0.949) or flow rate (p = 0.169). Practical issues, which may be relevant to clinical use, also emerged during testing. Our results suggest that there were significant differences in the performance of portable blood warming devices used at flow rates encountered in clinical practice.
02/05/2019
Tourniquet gonflable: Un nouveau venu
Rescue Bandage TQ Inflatable Tourniquet

Un garrot développé dans le cadre de la campagne STOP THE BLEED.
07/04/2019
Un drone pour le blessé de guerre ? Plutôt plusieurs
| Tags : drone
20/11/2018
The MARCH belt
De quoi avoir sur soi et sans ouvrir son sac pour réaliser le MARCH

CRO MARCH Belt (CROMEDICALGEAR.COM)
19/10/2018
Intubation dans le noir: Plutôt Poncho que JVN
OBJECTIVE:
Strict blackout discipline is extremely important for all military units. To be able to effectively determine wound characteristics and perform the necessary interventions at nighttime, vision and light restrictions can be mitigated through the use of tactical night vision goggles (NVGs). The lamp of the classical laryngoscope (CL) can be seen with the naked eye; infrared light, on the other hand, cannot be perceived without the use of NVGs. The aim of the study is to evaluate the safety of endotracheal intubation (ETI) procedures in the darkunder tactically safe conditions with modified laryngoscope (ML) model.
METHODS:
We developed an ML model by changing the standard lamp on a CL with an infrared light-emitting diode lamp to obtain a tool which can be used to perform ETI under night conditions in combination with NVGs. We first evaluated the safety of ETI procedures in prehospital conditions under darkness by using both the CL and the ML for the study, and then researched the procedures and methods by which ETI procedure could be performed in the dark under tactically safe conditions. In addition, to better ensure light discipline in the field of combat, we also researched the benefits, from a light discipline standpoint, of using the poncho liner (PL) and of taking advantage of the oropharyngeal region during ETIs performed by opening the laryngoscope blades directly in the mouth and using a cover. During the ETI procedures performed on the field, two experienced combatant staff simulated the enemy by determining whether the light from the two different types of laryngoscope could be seen at 100-m intervals up to 1,500 m.
RESULTS:
In all scenarios, performing observations with an NVG was more advantageous for the enemy than with the naked eye. The best measure that can be taken against this threat by the paramedic is to ensure tactical safety by having an ML and by opening the ML inside the mouth with the aid of a PL. The findings of the study are likely to shed light on the tactical safety of ETI performed with NVGs under darkness.
CONCLUSION:
Considering this finding, we still strongly recommend that it would be relatively safer to open the ML blade inside the mouth and to perform the procedures under a PL. In chaotic environments where it might become necessary to provide civilian health services for humanitarian aid purposes (Red Crescent, Red Cross, etc.) without NVGs, we believe that it would be relatively safer to open the CL blade inside the mouth and to perform the procedures under a PL.
17/01/2018
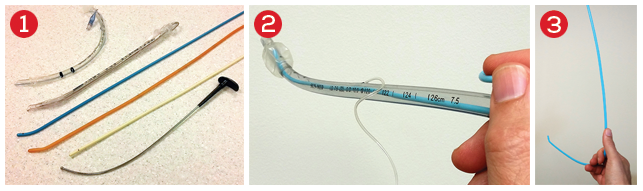
Histoire de mandrin
Il n'est parfois pas simple de bien maintenir un mandrin d'intubation dans le bon axe. Vous sont proposé en 3,4 et 5 plusieurs manières de s'en sortir.
15/01/2018
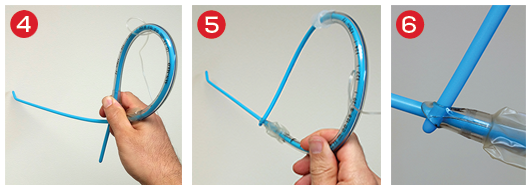
Une sonde de Foley dans le thorax
Balloon Foley catheter compression as a treatment for intercostal vessel bleeding
Chao BF et Al. Injury. 2011 Sep;42(9):958-9.
Avoir DEUX FOLEY avec soi, et ce n'est pas pour faire un sondage urinaire mais pour réaliser un tamponnement nasal, intercostale, d'une plaie cervicale ou tout simpment pour draîner un thorax
21/07/2017
SOFT-Tourniquet: Du nouveau
Tactical Médical Solutions qui est le fabricant du SOFT-Tourniquet, garrot en dotation dans l'armée française, propose une nouvelle version de son garrot Wide. Sa nouvelle boucle est d'emploi bien plus aisé que la précédente et positionne ce garrot parmi les tous meilleurs(CAT, SOFT-T, TK4,...)

Clic sur l'image pour accéder au site. Le distributeur en France.
| Tags : tourniquet
21/09/2016
Trauma Jonctionnel: Quels dispositifs appliquables ?
12/01/2016
Echographe ultraportable: Du choix !
L'embarras du choix mais l'expertise doit passer avant





| Tags : échographie
18/12/2015
Ejector ventilator: Quésaco ?
Ventrain: an ejector ventilator for emergency use
Hamaekers AE et Al. Br J Anaesth. 2012 Jun;108(6):1017-21
----------------------------------------
La ventilation sur cathéter de coniotomie n'est pas chose aisée du fait de l'importance des résistances à l'écoulement des gaz dans un cathéter de petit diamètre. On considère que sans dispositif d'injection de type manujet, il faut un cathéter d'au moins 4 mm pour assurer un minimum acceptable. Certains ont proposé d'avoir recours à une expiration active. Il s'agissait de dispositifs expérimentaux. Ce n'est pas le cas du Ventrain qui apparaît être un produit abouti. A suivre
----------------------------------------
The Use of Ventrain from Ventinova Medical BV on Vimeo.
| Tags : coniotomie
23/11/2015
Médecine militaire et civile
Apports de la médecine de l’avant militaire en situation préhospitalière civile
Derkenne C. et Al. Ann. Fr. Med. Urgence (2015) 5:245-251
L’évolution récente des matériels issus de la médecine de guerre pourrait profiter à la médecine préhospitalièrecivile. Des dispositifs comme les garrots ou les pansements hémostatiques sont encore très peu diffusés en pratique civile, malgré des recommandations fortes et assez anciennes de sociétés savantes civiles. Les dispositifs de lutte contre l’hypothermie en préhospitalier sont, en pratique civile, limités, là où les praticiens militaires disposent de couvertures perfectionnées et beaucoup plus efficaces. Enfin, un modèle de kit de drain thoracique, ergonomique, léger et autorisant l’autotransfusion nous paraît pouvoir avantageusement remplacer les différents moyens disponibles en Smur. Selon des données scientifiques issues essentiellement de la médecine militaire, l’utilisation de ces matériels en médecine préhospitalière civile pourrait être particulièrement utile lors de la prise en charge de traumatisés sévères.
| Tags : matériel
04/11/2015
Refroidir sans eau au Mali: Possible !
Couverture Polarskin Pervivolabs
La précocité du refroidissement d'une hyperthermie est fondamentale. Problème comment faire quand on n'a pas d'eau. Cette situation est particulièrement fréquente au sahel. Des produits innovants comme ceux de la gamme Polarskin de la société Pervivolabs, qui dispose d'un distributeur en France, pourraient apporter une solution. Il faut néanmoins que ces couvertures soient transportées en glacière. Mais ceci est plus facile à trouver que de l'eau.
| Tags : hyperthermie
11/10/2015
Bande de compression
Battle Wrap et Battle Bandage

Pouvoir réaliser un pansement compressif est essentiel notamment lors de la prise en charge de trauma jonctionnels. La réalisation et la tenue dans le temps des pansements peut s'avérer complexe. Le produit proposé par cette société semble intéressant car il permet de pouvoir disposer sous un très faible volume/poids d'un équipement permettant un bandage compressif large.
| Tags : pansement