30/04/2014
Pédiatrie en OPEX: Vue US
| Tags : pédiatrie
23/04/2014
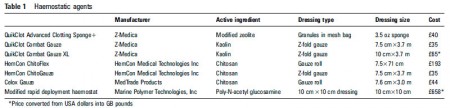
Haemostatic dressings in prehospital care
Haemostatic dressings in prehospital care
Smith AH et Al. Emerg Med J 2013;30:784–789
ABSTRACT
Massive haemorrhage still accounts for up to 40% of mortality after traumatic injury. The importance of limiting blood loss after injury in order to prevent its associated complications has led to rapid advances in the development of dressings for haemostatic control. Driven by recent military conflicts, there is increasing evidence to support their role in the civilian prehospital care environment. This review aims to summarise the key characteristics of the haemostatic dressings currently available on the market and provide an educational review of the published literature that supports their use. Medline and Embase were searched from start to January 2012. Other sources included both manufacturer and military publications. Agents not designed for use in prehospital care or that have been removed from the market due to significant safety concerns were excluded. The dressings reviewed have differing mechanisms of action. Mineral based dressings are potent activators of the intrinsic clotting cascade resulting in clot formation. Chitosan based dressings achieve haemostasis by adhering to damaged tissues and creating a physical barrier to further bleeding. Acetylated glucosamine dressings work via a combination of platelet and clotting cascade activation, agglutination of red blood cells and local vasoconstriction. Anecdotal reports strongly support the use of haemostatic dressings when bleeding cannot be controlled using pressure dressings alone; however, current research focuses on studies conducted using animal models. There is a paucity of published clinical literature that provides an evidence base for the use of one type of haemostatic dressing over another inhumans.
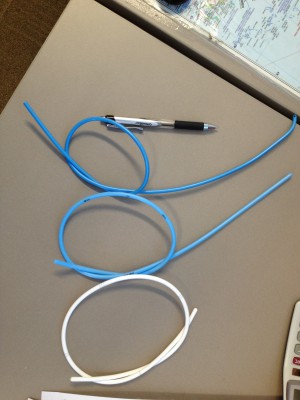
Le pansement OLAES MODULAR BANDAGE
Probablement le meilleur des pansements compressifs
C'est un pansement polyvalent qui permet trois actions. C'est d'abord un pansement plus compressif que le pansement israélien. Il permet en plus la réalisation d'un "packing" de plaie car il contient une bande de gaze en plus. Il permet également la réalisation d'un équivalent de pansement trois côtés ou un emballage succinct d'éviscération car il contient un petit champ transparent. Enfin de taille 6' au lieu de 4', il permet de couvrir des plaies plus importantes que le pansement israélien. Ce pansement est mis en place pour devenir le pansement standard de l'auxiliaire sanitaire.
Une démonstration de mise en oeuvre est --là-- . A noter qu'il existe une version non stérile, moins chère, en principe prévue pour l'entraînement.
15/04/2014
Analyse cognitive de tâche: Une nécessité pour l'enseignant
The Effectiveness of a Cognitive Task Analysis Informed Curriculum to Increase Self-Efficacy and Improve Performance for an Open Cricothyrotomy
Campbell J et All. J Surg Educ. 2011 Sep-Oct;68(5):403-7.
Un des enjeux de l'apprentissage d'un geste technique est de reproduire la séquence nécessaire tele que décrite par un expert. Hors il est démontré que près de la moitié des phases nécessaires ne sont pas décrites par ces derniers. L'analyse cognitive de tâche est une technique visant à identifier toutes ces phases réalisées de manière inconsciente par les experts qui dès lors de les décrivent pas. La référence proposée porte sur la coniotomie, mais toute activité technique est concernée.
OBJECTIVE: This study explored the effects of a cognitive task analysis (CTA)-informed curriculum to increase surgical skills cothyrotomy, procedural skills, surgical skills, curriculum performance and self-efficacy beliefs for medical students and development postgraduate surgical residents learning how to perform an open cricothyrotomy.
METHODS: Third-year medical students and postgraduate year 2 and 3 surgery residents were assigned randomly to either the CTA group (n ϭ 12) or the control group (n ϭ 14). The CTA group learned the open cricothyrotomy procedure using the CTA curriculum. The control group received the traditional curriculum.
RESULTS: The CTA group outperformed the control group significantly based on a 19-point checklist score (CTA mean score: 17.75, standard deviation [SD] ϭ 2.34; control mean score: 15.14, SD ϭ 2.48; p ϭ 0.006). The CTA group also reported significantly higher self-efficacy scores based on a 140- point self-appraisal inventory (CTA mean score: 126.10, SD ϭ 16.90; control: 110.67, SD ϭ 16.8; p ϭ 0.029).
CONCLUSIONS: The CTA curriculum was effective in increasing the performance and self-efficacy scores for postgraduate surgical residents and medical students performing an open cricothyrotomy.
14/04/2014
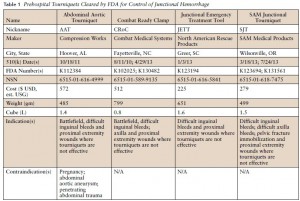
Tourniquet jonctionnel: Réflexions US
Management of Junctional Hemorrhage in Tactical Combat Casualty Care: TCCC Guidelines–Proposed Change 13-03
Kotwal RS et Al. J Spec Oper Med. 2013 Winter;13(4):85-93.
Clic sur l'image pour accéder au document
L'industrie nous propose des "garrots jonctionnels". Difficile de se faire une idée précise. Les US ont intégré le CRoC au TCCC. Cependant ce dispositif n'est pas si simple à monter. Cet article offre une lecture intéressante sur le sujet. Le tourniquet abdominal ne doit pas être appliqué plus d'une heure. Les autres le peuvent pour une durée maximum de 4 heures. Enfin le Sam Junctional Tourniquet est homologué par la FDA en tant que ceinture pelvienne.
| Tags : jonctionnel
09/04/2014
Gestion de l'eau: OXFAM
| Tags : soutien populations
Gestion de l'eau: CICR
| Tags : soutien populations
Situation d'urgences et population: CARE
Clic sur l'image pour accéder au document
L'intérêt de ce document est de proposer un panel de formulaires opérationnels
| Tags : soutien populations
Situation d'urgences et population: UNICEF
| Tags : soutien populations
Situation d'urgences et population: UNHCR
| Tags : soutien populations
08/04/2014
Coniotomie au Combat: Simuler pour retenir le savoir
Vincent H. et Al. Anesthesiology 2014; 120:999-1008
background:
The effectiveness of simulation is rarely evaluated. The aim of this study was to assess the impact of a short training course on the ability of anesthesiology residents to comply with current difficult airway management guidelines.
METHODS:
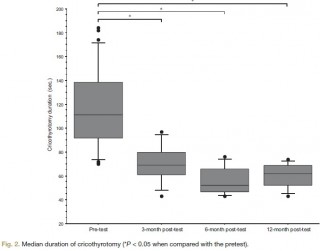
Twenty-seven third-year anesthesiology residents were assessed on a simulator in a "can't intubate, can't ventilate" scenario before the training (the pretest) and then randomly 3, 6, or 12 months after training (the posttest). The scenario was built so that the resident was prompted to perform a cricothyrotomy. Compliance with airway management guidelines and the cricothyrotomy's duration and technical quality were assessed as a checklist score [0 to 10] and a global rating scale [7 to 35].
RESULTS:
After training, all 27 residents (100%) complied with the airway management guidelines, compared with 17 (63%) in the pretest (P < 0.005). In the pretest and the 3-, 6-, and 12-month posttests, the median [range] duration of cricothyrotomy was respectively 117 s [70 to 184], 69 s [43 to 97], 52 s [43 to 76], and 62 s [43 to 74] (P < 0.0001 vs. in the pretest), the median [range] checklist score was 3 [0 to 7], 10 [8 to 10], 9 [6 to 10], and 9 [4 to 10] (P < 0.0001 vs. in the pretest) and the median [range] global rating scale was 12 [7 to 22], 30 [20 to 35], 33 [23 to 35], and 31 [18 to 33] (P < 0.0001 vs. in the pretest). There were no significant differences between performance levels achieved in the 3-, 6-, and 12-month posttests.
CONCLUSION: The training session significantly improved the residents' compliance with guidelines and their performance of cricothyrotomy.
| Tags : airway, intubation
07/04/2014
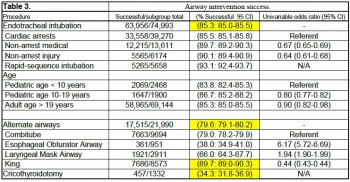
Airway en préhospitalier US: Plus tube que dispositif glottique
An update on out-of-hospital airway management practices in the United States
Diggs LA. et Al. Resuscitation. 2014 Mar 15. pii: S0300-9572
______________________________________________________
Ce document fait le point sur la pratique préhospitalière US. Cette dernière est faite avant tout d'intubation et la prudence est de mise concernant les performances réelles des dispositifs supra-glottiques avec lesquels (excepté le tube de king) les résultats sont moins bons.
______________________________________________________
OBJECTIVE: We characterized out-of-hospital airway management interventions, outcomes, and complications using the 2012 NEMSIS Public-Release Research Data Set containing almost 20 million Emergency Medical Services activations from 40 states and two territories. We compared the outcomes with a previous study that used 2008 NEMSIS data containing 16 states with 4 million EMS activations.
METHODS:
Patients who received airway management interventions including endotracheal intubation (ETI), alternate airways (Combitube, Laryngeal Mask Airway (LMA), King LT, Esophageal-Obturator Airway (EOA)), and cricothyroidotomy (needle and surgical) were identified. Using descriptive statistics, airway management success and complications were examined in the full cohort and key subsets including cardiac arrest, non-arrest medical, non-arrest injury, children<10 years, children 10-19 years, rapid sequence intubation (RSI), population setting, US census region, and US census division.
RESULTS:
Among 19,831,189 EMS activations, there were 74,993 ETIs, 21,990 alternate airways, and 1332 cricothyroidotomies. ETI success rates were: overall 63,956/74,993 (85.3%; 95% CI: 85.0-85.5), cardiac arrest 33,558/39,270 (85.5%), non-arrest medical 12,215/13,611 (89.7%), non-arrest injury (90.1%), children<10 years 2069/2468 (83.8%), children 10-19 years 1647/1900 (86.7%), adults>19 years 58,965/69,144 (85.3%), and rapid sequence intubation 5265/5658 (93.1%). Major complications included bleeding 677 (4.4 per 1000 interventions), vomiting 1221 (8 per 1000 interventions), esophageal intubation immediately detected 874 (5.7 per 1000 interventions), and esophageal intubations other 219 (1.4 per 1000 interventions).
CONCLUSIONS:
Paramedics provide life-saving emergency medical care to patients in the out-of-hospital setting. Only selected emergency medical procedures have proved to be safe and effective. The safety and efficacy profile of ETI has been challenged in the last ten years. Intubation has been the standard of care in the United States for more than thirty years and is regarded as one of the most important EMS procedures. In this study, we retrospectively examined the largest aggregate of EMS data currently available and observed low out-of-hospital ETI success rates.
ETI is a complex procedure requiring skilled choreography and numerous critical decisions and actions. In the absence of qualified personnel, or if ETI proves problematic, alternate airways are commonly employed. As more EMS systems embrace alternate airway devices in lieu of ETI, it is important to have a clear appreciation of the true success rates of airway procedures using these devices across a variety of patient characteristics and clinical settings. This study examined the most commonly used alternate airway devices including the Combitube, Esophageal Obturator Airway, Laryngeal Mask Airway, King Laryngeal Tube, and cricothyroidotomy and observed very low alternate airway success rates in the largest population sample to date. Alternate airway success rates were substantially lower than ETI success rates except for the King LT.
| Tags : airway, intubation
Le point sur le contrôle des hémorragies externes
An Evidence-based Prehospital Guideline for External Hemorrhage Control: American College of Surgeons Committee on Trauma
Bulger EM et Al. Prehosp Emerg Care. 2014 Apr-Jun;18(2):163-73.
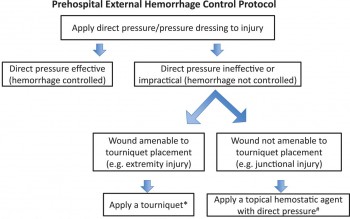
Cet article fait le point à partir de données publiées sur les grands principes d'arrêt des hémorragies externes: Compression directe, garrot artériel en cas d'inefficacité, relatif faible niveau de preuves pour les pansements hémostatiques à utiliser néanmoins comme agent de packing de plaies, nécessité de poursuivre la recherche sur les dispositifs de compression jonctionnelle.
ATTENTION Il s'agit de préhospitalier CIVIL
Clic sur l'image pour accéder au document
| Tags : hémorragie, garrot
05/04/2014
Garrot tactique: En bref
01/04/2014
Bougie d'intubation: Pas toutes égales
Bougie-related airway trauma: dangers of the hold-up sign
Marson BA et Al. Anaesthesia 2014, 69, 219–223
Le bon positionnement d'un mandrin d'intubation est confirmé parles sensations de ressaut quand l'extrémité de ce dernier franchit les anneaux trachéaux et par le blocage de ce dernier dans l'arbre bronchique. Ce dernier signe est appelé "the hold up sign" par les anglo-saxons. Ce blocage confirme que le mandrin n'est pas intra-oesophagien auquel cas il n'existerait pas. Cette publication attire l'attention sur le danger potentiel de traumatisme trachéal.
----------------------------------------------------------------------------
The bougie is a popular tool in difficult intubations. The hold-up sign is used to confirm tracheal placement of a bougie. This study aimed to establish the potential for airway trauma when using this sign with an Eschmann reusable bougie or a Frova single-use bougie. Airways were simulated using a manikin (hold-up force) and porcine lung model (airway perforation force). Mean (SD) hold-up force (for airway lengths over the range 25–45 cm) of 1.0 (0.4) and 5.2 (1.1) N were recorded with the Eschmann and Frova bougies, respectively (p < 0.001). The mean (SD) force required to produce airway perforation was 0.9 (0.2) N with the Eschmann bougie and 1.1 (0.3) N with the Frova bougie (p = 0.11). It is possible to apply a force at least five times greater than the force required to produce significant trauma with a Frova single-use bougie. We recommend that the hold-up sign should no longer be used with single-use bougies. Clinicians should be cautious when eliciting this sign using the Eschmann re-usable bougie.
--------------------------------------------------------------------------------------------------------------
Il existe d'autres bougies que celle d'eschmann et de Frova comme l'Introes pocket bougie ou la traffic light bougie. Cette dernière apparaît très intéressante car permettant de limiter la longueur de mandrin inséré dans la trachée et partant le risque de perforation trachéale.
| Tags : intubation