31/01/2014
Douleur et dossiers UPSA
| Tags : douleur douleur
29/01/2014
Trauma ballistique de la face: 1/3 nécessitent un airway sécurisé
Gunshot wounds and blast injuries to the face are associated with significant morbidity and mortality: Results of an 11-year multi-institutional study of 720 patients
Shackford et All. J Trauma Acute Care Surg. 2014;76: 347-352
BACKGROUND:
Gunshot wounds and blast injuries to the face (GSWBIFs) produce complex wounds requiring management by multiple surgical specialties. Previous work is limited to single institution reports with little information on processes of care or outcome. We sought to determine those factors associated with hospital complications and mortality.
METHODS:
We performed an 11-year multicenter retrospective cohort analysis of patients sustaining GSWBIF. The face, defined as the area anterior to the external auditory meatuses from the top of the forehead to the chin, was categorized into three zones: I, the chin to the base of the nose; II, the base of the nose to the eyebrows; III, above the brows. We analyzed the effect of multiple factors on outcome.
RESULTS:
From January 1, 2000, to December 31, 2010, we treated 720 patients with GSWBIF (539 males, 75%), with a median age of 29 years. The wounding agent was handgun in 41%, explosive (shotgun and blast) in 20%, rifle in 6%, and unknown in 33%. Prehospital or resuscitative phase airway was required in 236 patients (33%). Definitive care was rendered by multiple specialties in 271 patients (38%). Overall, 185 patients died (26%), 146 (79%) within 48 hours. Of the 481 patients hospitalized greater than 48 hours, 184 had at least one complication (38%). Factors significantly associated with any of a total of 207 complications were total number of operations (p < 0.001), Revised Trauma Score (RTS, p < 0.001), and head Abbreviated Injury Scale (AIS) score (p < 0.05). Factors significantly associated with mortality were RTS (p < 0.001), head AIS score (p < 0.001), total number of operations (p < 0.001), and age (p < 0.05). An injury located in Zone III was independently associated with mortality (p < 0.001).
CONCLUSION:
GSWBIFs have high mortality and are associated with significant morbidity. The multispecialty involvement required for definitive care necessitates triage to a trauma center and underscores the need for an organized approach and the development of effective guidelines.
| Tags : airway
28/01/2014
Airway préhospitalier: L'approche israélienne
Prehospital intubation success rates among Israel Defense Forces providers: Epidemiologic analysis and effect on doctrine
Katzenell U. et All. J Trauma Acute Care Surg. 2013 Aug;75(2 Suppl 2):S178-83
-------------------------------------------------------------------------------------------
Un taux de succès somme toute acceptable mais par la répétition des essais. Un algorithme simple puisqu'il ne fait appel qu'à 3 techniques: l'intubation, la coniotomie et la ventilation au masque. Les auteurs recommandent de ne pas se tromper de combat et d'éviter de rentrer dans celui de l'intubation si le contexte opérationnel est très présent. Au final assez proche de ce qui est prôné dans la procédure du sauvetage au combat.
-------------------------------------------------------------------------------------------
BACKGROUND:
Advanced airway management is composed of a set of vital yet potentially difficult skills for the prehospital provider, with widely different clinical guidelines. In the military setting, there are few data available to inform guideline development. We reevaluated our advanced airway protocol in light of our registry data to determine if there were a preferred maximum number of endotracheal intubation (ETI) attempts; our success with cricothyroidotomy (CRIC) as a backup procedure; and whether there were cases where advanced airway interventions should possibly be avoided.
METHODS:
This is a descriptive, registry-based study conducted using records of the Israel Defense Forces Trauma Registry at the research section of the Trauma and Combat Medicine Branch, Surgeon General's Headquarters. We included all casualties for whom ETI was the initial advanced airway maneuver, and the number of ETI attempts was known. Descriptive statistics were used.
RESULTS:
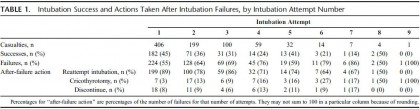
Of 5,553 casualties in the Israel Defense Forces Trauma Registry, 406 (7.3%) met the inclusion criteria. Successful ETI was performed in 317 casualties (78%) after any number of ETI attempts; an additional 46 (11%) underwent CRIC, and 43 (11%) had advanced airway efforts discontinued. ETI was successful in 45%, 36%, and 31% of the first, second, and third attempts, respectively, with an average of 28% success over all subsequent attempts. CRIC was successful in 43 (93%) of 46 casualties in whom it was attempted. Of the 43 casualties in whom advanced airway efforts were discontinued, 29 (67%) survived to hospital discharge.
CONCLUSION:
After the first ETI attempt, success with subsequent attempts tended to fall, with minimal improvement in overall ETI success seen after the third attempt. Because CRIC exhibited excellent success as a backup airway modality, we advocate controlling the airway with CRIC if ETI efforts have failed after two or three attempts. We recommend that providers reevaluate whether definitive airway control is truly necessary before each attempt to control the airway.
The tourniquet manual
| Tags : tourniquet
AMEDD Journal
27/01/2014
Scandinavian Journal
Reanoxyo
Médecine et Armées
Actusanté
16/01/2014
Coup de chaleur: Bases
| Tags : hyperthermie
15/01/2014
Coup de chaleur: Refroidir
Hyperthermie d’effort : comment refroidir ?
| Tags : hyperthermie
14/01/2014
L'enfant traumatisé: Une rencontre CERTAINE
Management of children in the deployed intensive care unit at Camp Bastion, Afghanistan
Inwald DP, et al. J R Army Med Corps 2013;0:1–5. doi:10.1136/jramc-2013-000177
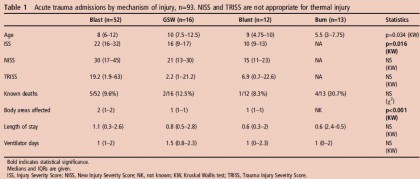
Background The deployed Intensive Therapy Unit (ITU) in the British military field hospital in Camp Bastion, Afghanistan, admits both adults and children. The purpose of this paper is to review the paediatric workload in the deployed ITU and to describe how the unit copes with the challenge of looking after critically injured and ill children.
Methods Retrospective review of patients <16 years of age admitted to the ITU in the British military field hospital in Camp Bastion, Afghanistan, over a 1-year period from April 2011 to April 2012.
Results 112/811 (14%) admissions to the ITU were paediatric (median age 8 years, IQR 6–12, range 1–16).80/112 were trauma admissions, 13 were burns, four were non-trauma admissions and 15 were readmissions.
Mechanism of injury in trauma was blunt in 12, blast (improvised explosive device) in 45, blast (indirect fire) in seven and gunshot wound in 16. Median length of stay was 0.92 days (IQR 0.45–2.65). 82/112 admissions (73%) were mechanically ventilated, 16/112 (14%) required inotropic support. 12/112 (11%) died before unit discharge. Trauma scoring was available in 65 of the 80 trauma admissions. Eight had Injury Severity Score or New Injury Severity Score >60, none of whom survived. However, of the 16 patients with predicted mortality >50% by Trauma Injury Severity Score, seven survived. Seven cases required specialist advice and were discussed with the Birmingham Children’s Hospital paediatric intensive care retrieval service. The mechanisms by which the Defence Medical Services support children admitted to the deployed adult ITU are described, including staff training in clinical, ethical and child protection issues, equipment, guidelines and clinical governance and rapid access to specialist advice in the UK.
Conclusions With appropriate support, it is possible to provide intensive care to children in a deployed military ITU.
| Tags : pédiatrie
13/01/2014
Coup de chaleur: Explorer
Hyperthermie d’effort : pourquoi explorer ?
| Tags : hyperthermie
12/01/2014
Exsufflation: 1 / 4 sans pneumothorax !
Inadequate Needle Thoracostomy Rate in the Prehospital Setting for Presumed Pneumothorax. An Ultrasound Study
Blaivas M. J Ultrasound Med 2010; 29:1285–1289
---------------------------------------------------------------------
Nombreux ont attiré l'attention sur le risque d'inefficacité des exsufflations au cathéter à cause de la longueur de ces derniers, plus court que l'épaisseur de la paroi thoracique. Certains prônent l'emploi de cathéter de plus de 8 cm sans véritablement de fondements scientifiques (Lire cette analyse). Entre des mains peu expérimentées cette pratique apparaît dangereuse du fait du fait des erreurs faites sur les niveaux de ponction, ce d'autant que ces cathéters ne sont pas très efficaces dans le temps. L'article proposé incite encore plus à la nécessaire prudence à avoir avant de faire pénétrer une aiguille dans un thorax. En effet ce geste serait pratiqué 1 fois sur 4 en l'absence de pneumothorax.
---------------------------------------------------------------------
Objective. The purpose of this study was to evaluate the frequency of inadequate needle chest tho-racostomy in the prehospital setting in trauma patients suspected of having a pneumothorax (PTX) onthe basis of physical examination.
Methods. This study took place at a level I trauma center. All trauma patients arriving via emergency medical services with a suspected PTX and a needle thoracostomy were evaluated for a PTX with bedside ultrasound. Patients too unstable for ultrasound evaluation before tube thoracostomy were excluded, and convenience sampling was used. All patients were scanned while supine. Examinations began at the midclavicular line and included the second through fifth ribs. If no sliding lung sign (SLS) was noted, a PTX was suspected, and the lung point was sought for definitive confirmation. When an SLS was noted throughout and a PTX was ruled out on ultrasound imaging, the thoracostomy catheter was removed. Descriptive statistics were calculated.
Results. A total of 57 patients were evaluated over a 3-year period. All had at least 1 needle thoracostomy attempted; 1 patient underwent 3 attempts. Fifteen patients (26%) had a normal SLS on ultrasound examination and no PTX after the thoracostomy catheter was removed. None of the 15 patients were later discovered to have a PTX on subsequent computed tomography. Conclusions. In this study, 26% of patients who received needle thoracostomy in the prehospital setting for a suspected PTX appeared not to have had a PTX originally, nor had 1 induced by the needle thoracostomy. It may be prudent to evaluate such patients with bedside ultrasound instead of automatically converting all needle thoracostomies to tube thoracostomies.
---------------------------------------------------------------------
Recourir à l'échographie pleurale et réaliser ce geste par voie latérale avec un cathéter de 5 cm apparaissent être sécuritaire.
| Tags : exsufflation, decompression
11/01/2014
Prise en charge de la douleur
Clic sur l'image pour accéder à la plateforme
La connexion à ce site nécessite une inscription préalalble gratuite et donne accès aux cours du DIU et de la capacité
| Tags : douleur
07/01/2014
Pansement hémostatique: Restons critiques !
An Evidence-Based Review of the Use of a Combat Gauze (QuikClot) for Hemorrhage Control
Gegel BT et Al. Am Surg. 2011 Feb;77(2):162-5.
_________________________________________________________________________
L'efficacité des pansements hémostatiques apparaît être une évidence. Ils sont utilisés de manière large sans véritables fondements scientiifiques prouvés. Une analyse critique s'impose, ce d'autant qu'il s'agit de produits onéreux et que l'industrie a bien façonné notre manière de raisonner. Cet article le rappelle.
_________________________________________________________________________
Trauma is a leading cause of morbidity and mortality. Uncontrolled hemorrhage related to the traumatic event is often the major cause of complications and death. The use of hemostatic agents may be one of the easiest and most effective methods of treating hemorrhage. The US military recommends a hemostatic combat gauze (QuikClot Combat Gauze) as the first-line hemostatic agent for use in treatment of severe hemorrhage. This review provides essential information for evidence-based use of this agent. The PICO (patient, intervention, comparison, outcome) question guiding this search for evidence was: Is QuikClot Combat Gauze, a hemostatic agent, effective and safe in controlling hemorrhage in trauma patients in the prehospital setting? The evidence appraised was a combination of lower-level human and animal research. It did not conclusively demonstrate that this combat gauze is an effective hemostatic agent for use in trauma patients, but the results are promising in supporting its use. The evidence does not describe serious side effects, exothermic reaction, and thromboemboli formation associated with other hemostatic agents. Further inves tigation to determine the effectiveness of hemostatic agents, specifically QuikClot Combat Gauze, in the management of trauma casualties in the prehospital setting is required. These should include large-scale, multicenter, prehospital randomized controlled trials.
| Tags : hémorragie, pansement