Introduction Pelvic fractures often result from high-energy trauma and are associated with a 10% mortality rate and significant morbidity. Pelvic binders are applied in suspected pelvic injury to stabilise fractured bone, decrease bleeding and potentiate tamponade. A binder must hold the pelvis with sufficient force for this effect to be achieved. This study aims to quantify the ability of proprietary and improvised pelvic binders to hold a target tensile force over time.
Methods The ability of three proprietary and three improvised binders to hold a binding force for 2 hours was tested. A uniaxial materials testing machine was used to tension each binder to 150 N and then hold the displacement for 2 hours; the drop in tension over time was recorded for each binder. The ability to hold tension above 130 N after 2 hours was set as the metric of binder performance.
Results The median tension at 2 hours was above 130 N for the SAM Pelvic Sling II and T-POD Pelvic Stabilisation Device and was below 130 N for the Prometheus Pelvic Splint, field-expedient pelvic splint (FES) and the Personal Clothing System-Multi-Terrain Pattern Combat Trousers binders. The tension in the improvised FES after 2 hours was approximately at the target 130 N; however, in 40% of the tests, it held above 130 N.
Conclusions Binders varied in their ability to maintain sufficient tension to treat a pelvic fracture over the 2-hour testing period. The FES performed well under our testing regime; with relatively low cost and weight, it represents a good alternative to proprietary binders for the austere environment.
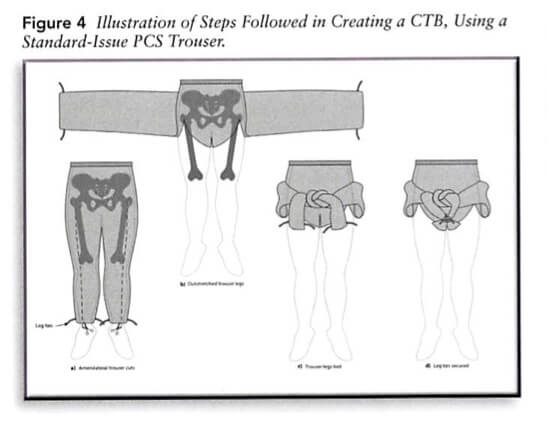
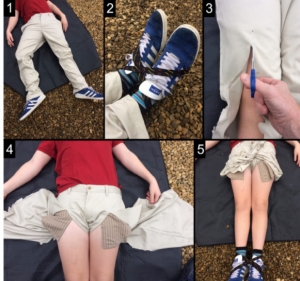
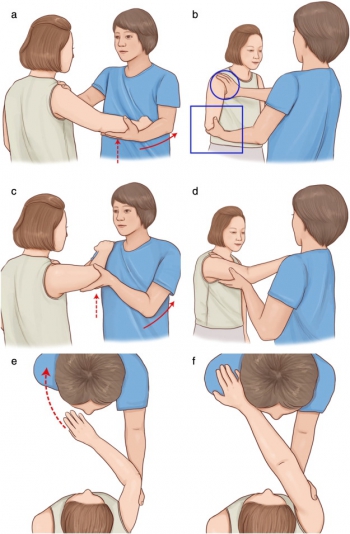
Le Field expedient System: Construit avec un garrot et une attelle SamSplint