03/03/2015
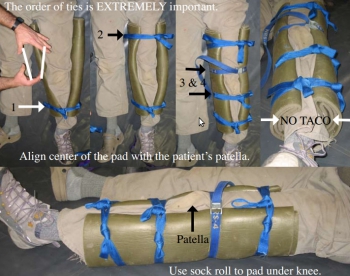
Tapis de sol: Pour immobiliser
| Tags : immobilisation
23/09/2014
Stabilisation pelvienne:
Les attelles de type Sam Splint sont INCONTOURNABLES en médecine militaire comme on peut le voir dans une brochure spécifique. Certains proposent de l'utiliser comme base d'une stabilisation pelvienne.
| Tags : immobilisation, pelvis
01/11/2013
Stabilisation pelvienne: Simple est efficace
Comparison of circumferential pelvic sheeting versus the T-POD on unstable pelvic injuries: A cadaveric study of stability
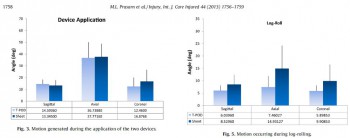
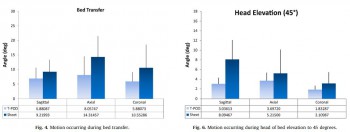
Prasarn ML et All. Injury. 2013 Jun 27. pii: S0020-1383(13)00256-8
Objectives: Commercially available binder devices are commonly used in the acute treatment of pelvic fractures, while many advocate simply placing a circumferential sheet for initial stabilization of such injuries. We sought to determine whether or not the T-POD would provide more stability to an unstable pelvic injury as compared to circumferential pelvic sheeting.
Methods: Unstable pelvic injuries (OTA type 61-C-1) were surgically created in five fresh, lightly embalmed whole human cadavers. Electromagnetic sensors were placed on each hemi-pelvis. The amount of angular motion during testing was measured using a Fastrak, three-dimensional, electromagnetic motion analysis device (Polhemus Inc., Colchester, VT). Either a T-POD or circumferential sheet was applied in random order for testing. The measurements recorded in this investigation included maximum displacements for sagittal, coronal, and axial rotation during application of the device, bed transfer, log-rolling, and head of bed elevation.
Results: There were no differences in motion of the injured hemi-pelvis during application of either the T-POD or circumferential sheet. During the bed transfer, log-rolling, and head of bed elevation, there were no significant differences in displacements observed when the pelvis was immobilized with either a sheet or pelvic binder (T-POD).
Conclusions: A circumferential pelvic sheet is more readily available, costs less, is more versatile, and is equally as efficacious at immobilizing the unstable pelvis as compared to the T-POD. We advocate the use of circumferential sheeting for temporary stabilization of unstable pelvic injuries.
| Tags : pelvis
24/11/2012
Stabilisation pelvienne: Un état des lieux à lire
The use of pelvic binders in the emergent management of potential pelvic trauma
Chesser TJS et all. Injury, Int. J. Care Injured 43 (2012) 667–669
| Tags : pelvis
03/12/2011
Rachis: Immobilisation et traumatismes pénétrants, que dit le PHTLS ?
Prehospital Spine Immobilization for Penetrating Trauma—Review
and Recommendations From the Prehospital Trauma Life Support
Executive Committe
http://www.ucdmc.ucdavis.edu/emergency/education/residenc...
- There are no data to support routine spine immobilization in patients with penetrating trauma to the neck or torso.
- There are no data to support routine spine immobilization in patients with isolated penetrating trauma to the cranium.
- Spine immobilization should never be done at the expense of accurate physical examination or identification and correction of life-threatening conditions in patients with penetrating trauma.
- Spinal immobilization may be performed after penetrating injury when a focal neurologic deficit is noted on physical examination although there is little evidence of benefit even in these cases.
ATTENTION
Le PHTLS, qui correspond à un ensemble de procédures destinée à être mises en oeuvre par des techniciens d'urgence, ne reflète pas du tout la pratique française.
20/11/2011
Stabilisation pelvienne: Au bon niveau
Ce document est à mettre en lien avec l'impotrance d'un positionnement correct de ces dispositifs. Il s'agit seulement d'une fois sur 2 d'un positionnement au niveau des grands trochanter. Dans près de 40% des cas le positionnement était trop haut.
| Tags : immobilisation, pelvis
Stabilisation pelvienne: Sam Sling, Tpod ou autre chose ?
Une présentation d'une publication portant sur la comparaison du T Pod, de la Sam Pelvic sling et du Pelvic binder qui sont les 3 dispositifs les plus couramment utilisés.
http://www.medicalsca.com/files/jb__js_-_pelvic_devices_c...
| Tags : immobilisation, pelvis
Pelvic Fracture Hemorrhage—Update and Systematic Review
| Tags : immobilisation, pelvis
12/11/2011
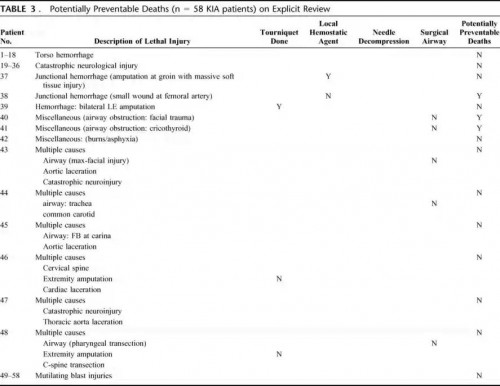
Cause de décès en afghanistan: Actualités canadiennes
Causes of Death in Canadian Forces Members Deployed to Afghanistan and Implications on Tactical Combat Casualty Care Provision
Pannell D et all. J Trauma. 2011;71: S401–S407
Ce document identifie par ailleurs l'importance de la formation des personels à la gestion des voies aériennes, des mesures de stabilisation du rachis en cas d'IED, du recours aux sondes de foley pour le tamponenment des hémorragies jonctionnelles en cas de non application possible de pansement hémostatique.
-------Morceaux choisis:
We recommend that combat medical technicians should continue to practice surgical airways in live-tissue laboratories. In addition, didactic teaching should continue to review the indications for cricothyrotomy on the battlefield. .........
...... Based on this review, we also feel that future Canadian TCCC courses may be improved by giving battlefield providers a treatment option for dealing with exsanguination from small wounds at junctional areas (groin, axillary, and neck). Currently, TCCC providers only have hemostatic dressings to deal with this difficult problem. However, unfavorable wound geometry can make utilization of these products unfeasible. In addition, TCCC providers have no option for treating carotid artery hemorrhage in the neck. We suggest that combat medical technicians also carry urinary catheters; these can be inserted into wound tracts of small wounds. Insufflation of the balloon may provide temporary hemostasis of junctional bleeding and buy enough time for evacuation to a definitive surgical facility. Another option would be to pack such wounds with ribbon gauze. These options may also be used for posterior packing of lifethreatening epistaxis associated with facial fractures.
On our review, we also noted that three casualties.....
....we recommend that spinal immobilization be considered for all casualties suffering from blunt trauma or IED-related incidents during “Tactical Field Care,” if the tactical situation permits, and if the medical technician deems the situation to be safe enough to proceed with this procedure.
Rachis: Immobilisation et IED, point de vue canadien
L'immobilisation du rachis sous le feu direct n'est pas recommandé par la procédure du sauvetage au combat. Cela ne veut pas dire qu'il ne faut jamais stabiliser un rachis. Les fractures du rachis sont relativement fréquentes chez le blessé par VBIED. Ce contexte est rarement celui d'une exposition des sauveteurs au feu direct de l'ennemi. Il est donc particulièrement important de bien faire, dans les programme de formation des personnels, entre la prise en charge d'un blessé dans le cadre de combat d'infanterie et de la prise en charge de blessés par balle ou éclats provenant de munition et celui de VBIED où en plus des projectiles interviennent les notions de projection éventuelles et d'exposition au blast.
C'est ce qu'exprime le document présenté, fruit de l'expérience canadienne qui rappelle la fréquence des lésions du rachis dans ce contexte et malheureusement l'insuffisance du recours à la stabilisation du rachis.
----------------------------
Spinal Injuries After Improvised Explosive Device Incidents: Implications for Tactical Combat Casualty Care
Comstock S et al. JTrauma. 2011;71:S413–S417
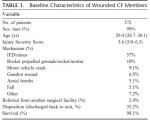
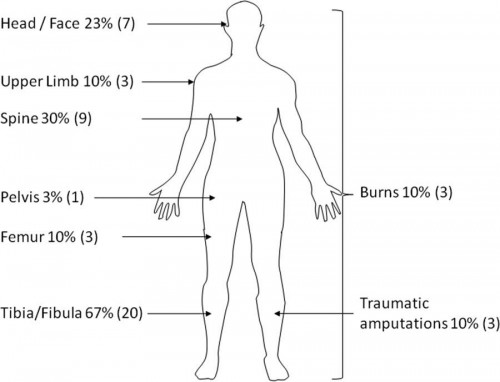
Background: Tactical Combat Casualty Care aims to treat preventable causes of death on the battlefield but deemphasizes the importance of spinal immobilization in the prehospital tactical setting. However, improvised explosive devices (IEDs) now cause the majority of injuries to Canadian Forces (CF) members serving in Afghanistan. We hypothesize that IEDs are more frequently associated with spinal injuries than non-IED injuries and that spinal precautions are not being routinely employed on the battlefield.
Methods: We examined retrospectively a database of all CF soldiers who were wounded and arrived alive at the Role 3 Multinational Medical Unit in Kandahar, Afghanistan, from February 7, 2006, to October 14, 2009. We collected data on demographics, injury mechanism, anatomic injury descriptions, physiologic data on presentation, and prehospital interventions performed. Outcomes were incidence of any spinal injuries.
Results: Three hundred seventy-two CF soldiers were injured during the study period and met study criteria. Twenty-nine (8%) had spinal fractures identified. Of these, 41% (n = 12) were unstable, 31% (n = 9) stable, and 28% indeterminate. Most patients were injured by IEDs (n = 212, 57%). Patients injured by IEDs were more likely to have spinal injuries than those injured by non–IED-related mechanisms (10.4% vs. 2.3%; p < 0.01). IED victims were even more likely to have spinal injuries than patients suffering blunt trauma (10.4% vs. 6.7%; p = 0.02). Prehospital providers were less likely to immobilize the spine in IED victims compared with blunt trauma patients (10% [22 of 212] vs. 23.0% [17 of 74]; p < 0.05).
Conclusions: IEDs are a common cause of stable and unstable spinal injuries in the Afghanistan conflict. Spinal immobilization is an underutilized intervention in the battlefield care of casualties in the conflict in Afghanistan. This may be a result of tactical limitations; however, current protocols should continue to emphasize the judicious use of immobilization in these patients.
16/10/2011
Rachis: Immobilisation et trauma du membre inférieur par VB IED
The Modern "Deck-Slap" Injury-Calcaneal Blast Fractures From Vehicle Explosions. Ramasamy A. et all
DOI: 10.1097/TA.0b013e318227a999
07/07/2011
Rachis: Immobilisation cervicale sans collier ?
Rachis: Immobilisation cervicale nécessaire au combat ?
L'immobilisation du rachis cervical n'estpas recommandée en CONDITION de combat d'INFANTERIE. Dans un travail effectué sur les blessés au Vietnam seuls % des blessés auraitent pu en tirer bénéfice. Mais la pose d'un collier cervical prend du temps exposant le sauveteur. 10% des blessés le sont à l'occasion de sauvetage.
En complément de l'article précédent:
"Care of the combat casualty with spinal column or spinal cord injury has not been previously described,
particularly in regards to spinal immobilization. The ultimate goal of spinal immobilization in the combat
casualty is to first ‘‘do no further harm’’ and then provide a stable, painless spine and an optimal
neurologic recovery. The protocol for treatment of the combat casualty with suspected spinal column
or spinal cord injury from the battlefield to final arrival at a definitive treatment center is discussed,
and the special considerations for medical evacuation off the battlefield and for aeromedical transport
are delineated. Selective prehospital spine immobilization, which involves spinal immobilization with
backboard, semi-rigid cervical collar, lateral supports, and straps or tape, is recommended if there
is suspicion of spinal column or spinal cord injury in the combat casualty and when conditions and
resources permit. The authors do not recommend spinal immobilization for the combat casualty with
isolated penetrating trauma. "
06/05/2011
Rachis: Immobilisation et plaies cervicales par balle
Unstable Cervical Spine Fracture After Penetrating Neck Injury: A Rare Entity in an Analysis of 1,069 Patients
Lustenberger T. et All.
JTrauma. 2011;70:870–872
-------------------------------------------------
En gros pas besoin de mettre en place une minerve en cas de plaie du cou sauf si le blessé est incosncient ou présente des signes neurologiques périphériques.
-------------------------------------------------
Background: The value of cervical spine immobilization after penetrating trauma to the neck is the subject of lively debate. The purpose of this study was to review the epidemiology of unstable cervical spine injuries (CSI) after penetrating neck trauma in a large cohort of patients.
Methods: This is a retrospective analysis of patients admitted with penetrating neck injuries to a Level I trauma center from January 1996 through December 2008. A penetrating neck injury was defined as a gunshot wound (GSW) or stab wound (SW) between the clavicles and the base of the skull. Univariate and multivariate analyses were performed to investigate associations between injury mechanisms, the presence of CSI instability, and mortality. Risk factors independently associated with the presence of a CSI were identified.
Results: A total of 1,069 patients met inclusion criteria, of which 463 patients (43.3%) and 606 patients (56.7%) were sustaining GSW and SW, respectively. Overall, 65 patients (6.1%) were diagnosed with a CSI with a significantly higher incidence after GSWs compared with SWs (12.1% vs. 1.5%; p < 0.001). In four patients (0.4%), the CSI was considered unstable, all of them following GSW. All patients with unstable CSI had obvious neurologic deficits or altered mental status at the time of admission. Risk factors independently associated with the presence of a CSI were GSW to the neck and a Glasgow Coma Scale score.
Conclusion: The overall incidence of unstable CSI after penetrating trauma to the neck is exceedingly low at 0.4%. Following GSW to the neck, an unstable CSI was noted in
-------------------------------------------------
Détail de la publication:
-------------------------------------------------
In four patients (0.4%), the CSI was considered unstable, all of them after GSW to the neck (0.9% for GSW vs. 0% for SW; p = 0.035). All patients with unstable CSI had obvious neurologic deficits or altered mental status at the time of initial presentation: two patients presented with tetraplegia and two patients had a GCS score of 3 on admission with subsequent brain death during their SICU stay. Stabilization of the spine was performed in both patients with tetraplegia but was without significant neurologic recovery after surgery.