21/06/2025
Crico en condition de combat
14/12/2023
Dispositifs supraglottiques:Pléthore ?
Review of Commercially Available Supraglottic Airway Devices for Prehospital Combat Casualty Care
01/04/2023
Trauma des voies aériennes
Blunt and Penetrating Airway Trauma
Duggan LV et Al.. Emerg Med Clin North Am. 2023 Feb;41(1S):e1-e15.
-----------------------------
C'est une chose compliquée, pas simple surtout en condition de combat et qui justifie la maîtrise d'un abord chirurgical du cou. Ce document est, je trouve, excellent.
-----------------------------
Airway injury, be that penetrating or blunt, is a high-stakes high-stress management challenge for any airway manager and their team. Penetrating and blunt airway injury vary in injury patterns requiring prepracticed skills and protocols coordinating care between specialties. Variables including patient cooperation, coexisting injuries, cardiorespiratory stability, care location (remote vs tertiary care center), and anticipated course of airway injury (eg, oxygenating well and comfortable vs increasing subcutaneous emphysema) all play a role in determining airway if and when airway management is required. Direct airway trauma is relatively infrequent, but its presence should be accompanied by in-person or virtual otolaryngology support.
| Tags : airway
16/03/2023
Crico: Rare mais une des justifications de la médicalisation de l'avant.
Incidence of rescue surgical airways after attempted orotracheal intubation in the emergency department: A National Emergency Airway Registry (NEAR) Study
Offenbacher J. et Al. Am J Emerg Med. 2023 Feb 25;68:22-27.
------------------------------------------
Il est fort probable qu'un médecin ou un infirmier militaire ne soit pas confronté à ce genre de situation. MAIS justement la présence d'un médecin ou d'un infirmier se justifie par la capacité à la réaliser. Il faut donc éviter de faire comme une autruche et ne pas se former et entretenir sa compétence en la matière.
------------------------------------------
Background:
Cricothyrotomy is a critical technique for rescue of the failed airway in the emergency department (ED). Since the adoption of video laryngoscopy, the incidence of rescue surgical airways (those performed after at least one unsuccessful orotracheal or nasotracheal intubation attempt), and the circumstances where they are attempted, has not been characterized.
Objective:
We report the incidence and indications for rescue surgical airways using a multicenter observational registry.
Methods:
We performed a retrospective analysis of rescue surgical airways in subjects ≥14 years of age. We describe patient, clinician, airway management, and outcome variables.
Results:
Of 19,071 subjects in NEAR, 17,720 (92.9%) were ≥14 years old with at least one initial orotracheal or nasotracheal intubation attempt, 49 received a rescue surgical airway attempt, an incidence of 2.8 cases per 1000 (0.28% [95% confidence interval 0.21 to 0.37]). The median number of airway attempts prior to rescue surgical airways was 2 (interquartile range 1, 2). Twenty-five were in trauma victims (51.0% [36.5 to 65.4]), with neck trauma being the most common traumatic indication (n = 7, 14.3% [6.4 to 27.9]).
Conclusion:
Rescue surgical airways occurred infrequently in the ED (0.28% [0.21 to 0.37]), with approximately half performed due to a trauma indication. These results may have implications for surgical airway skill acquisition, maintenance, and experience.
| Tags : coniotomie
04/01/2023
Crico dans le noir: S'éclairer ?
Cric in the Dark: Surgical Cricothyrotomy in Low Light Tactical Environments
CW Getz et al. J Spec Oper Med. 2022 Dec 16;22(4):50-54
Background:
Surgical cricothyrotomy (SC) is a difficult procedure with high failure rates in the battlefield environment. The difficulty of this procedure is compounded in a low-light tactical environment in which white light cannot be used. This study compared the use of red-green (RG) light and red (R) light in the performance of SC in a low-light environment.
Materials and methods:
Tactical Combat Casualty Care-certified navy corpsmen (n = 33) were provided 15 minutes of standardized instruction followed by hands-on practice with the Tactical CricKit and the H&H bougie-assisted Emergency Cricothyrotomy Kit. Participants acclimated to a dark environment for 30 minutes before performing SC on a mannequin with both devices using both R and RG light in a randomized order. Application time, success, participant preference, and participant confidence were analyzed.
Results: There were similarly high levels of successful placement (>87.5%) in all four cohorts. Light choice did not appear to affect placement time with either of the two kits. On Likert-scale surveys, participants reported that RG decreased difficulty (p < .0001) and increased confidence (p < .0001) in performing the procedure.
Conclusion: RG light increased confidence and decreased perceived difficulty when performing SC, though no differences in placement time or success were observed.
09/11/2022
Ouvrir le cou quand on ne voit rien
Definitive Management of a Traumatic Airway: Case Report
Fabich RA et Al. , MILITARY MEDICINE, 185, 1/2:e312, 2020
Maxillofacial and neck trauma from penetrating injuries present unique challenges for anesthesia providers and surgeons. In the austere conditions of a combat setting these challenges may be amplified due to limited resources and injury severity. Currently there is a lack of evidence and consensus on how to best manage a traumatized airway in this situation. The authors of this paper present the successful emergency management of a traumatized airway from a severe maxillofacial and neck-penetrating wound. A stepwise team approach using strong communication and a global mental model facilitated definitive airway management in this case allowing for safe transport to definitive care.
| Tags : coniotomie
04/10/2022
NAEMSP Prehospital Airway Position Papers
The National Association of EMS Physicians Compendium of Airway Management Position Statements and Resource Documents
Clic sur le titre pour accéder à la page de présentation des documents
| Tags : airway
05/07/2022
Dispositifs supraglottiques:Pléthore ?
Review of Commercially Available Supraglottic Airway Devices for Prehospital Combat Casualty Care
19/12/2021
Ouvrir un cou: Ne s'invente pas !
Effectiveness of a simulation-based mastery learning to train clinicians on a novel cricothyrotomy procedure at an academic medical centre during a pandemic: a quasi-experimental cohort study
Nabil Issa N et Al. BMJ Open. 2021 Nov 19;11(11):e054746. doi: 10.1136/bmjopen-2021-054746.
Objectives: To develop and evaluate a simulation-based mastery learning (SBML) curriculum for cricothyrotomy using wet towels to suppress aerosolisation during a pandemic.
Design: Quasi-experimental, pre-post study.
Setting: Tertiary care, academic medical centre in Chicago.
Participants: Ear, nose and throat and general surgery residents, fellows and attendings.
Intervention: Cricothyroidotomy simulation-based mastery learning curriculum.
Outcomes measure: Pretest to posttest simulated cricothyrotomy skills checklist performance.
Results: 37 of 41 eligible surgeons participated in the curriculum. Median pretest score was 72.5 (IQR 55.0-80.0) and 100.0 (IQR 98.8-100.0) for the posttest p<0.001.

All participants scored at or above a minimum passing standard (93% checklist items correct) at posttest.
Conclusions: Using SBML is effective to quickly train clinicians to competently perform simulated cricothyrotomy during a pandemic.
27/02/2021
Coniotomie: Apprendre ET s'entretenir
Emergency Cricothyrotomy: A 10-Year Single Institution Experience
Moroco AE et Al. Am Surg. 2021 Feb 10;3134821995075. doi: 10.1177/0003134821995075.
--------------------------------
Même entre des mains chirurgicales ce geste n'est pas si simple que certains le disent. Pourtant il faut le connaître et surtout maintenir la pratique enseignée.
--------------------------------
Background:
With recent technological advances reducing the demand for emergent surgical airway placement, surgeons are less often performing this life-saving procedure. We sought to assess the characteristics and outcomes surrounding patients undergoing modern emergent cricothyrotomy.
Methods:
A retrospective case series was performed between January 2010 and January 2020 at a single tertiary academic level 1 trauma center. Patients who underwent tracheostomy (CPT 31600, 31601) within 48 hours of admission or listed in the trauma registry were queried. Charts were individually reviewed to identify patients with cricothyrotomy. Demographic, operative and relevant hospital course data were collected.
Results:
A total of 1642 patients were identified with 12 of those found to have met inclusion criteria. The population was mostly male (91.7%) with an average age of 43 years and average body mass index of 30. Survival rate of patients was 75%. A total of 7 patients (58%) had appropriate anatomical placement of cricothyrotomy. Of those patients, 75% were performed by Trauma Surgery. Of the 5 patients with misplaced cricothyrotomy, all were male, with an average age and body mass index of 36 years and 25, respectively. Procedures were performed by prehospital personnel (20%), referring hospital (20%), and Trauma Surgery (60%).
Discussion:
Cricothyrotomy remains a vital tool in the successful management of emergent airway access. The most common complication observed was improper anatomical placement, which occurred in nearly half of patients. Trauma surgeons perform 75% of cricothyrotomies, with an anatomical accuracy rate of 66.7%.
27/11/2020
Trauma du larynx: Faites une échographie !
Novel role of focused airway ultrasound in early airway assessment of suspected laryngeal trauma
Adi et al. Ultrasound J (2020) 12:37
Case presentation
We report a case series that illustrate the diagnostic value of focused airway ultrasound in the diagnosis of laryngeal trauma in patients presenting with blunt neck injury.
Conclusion
Early recognition, appropriate triaging, accurate airway evaluation, and prompt management of such injuries are essential. In this case series, we introduce the potential role of focused airway ultrasound in suspected laryngeal trauma, and the correlation of these exam findings with that of computed tomography (CT) scanning, based on the Schaefer classification of laryngeal injury.
26/09/2020
Le doigt plutôt qu'un guide
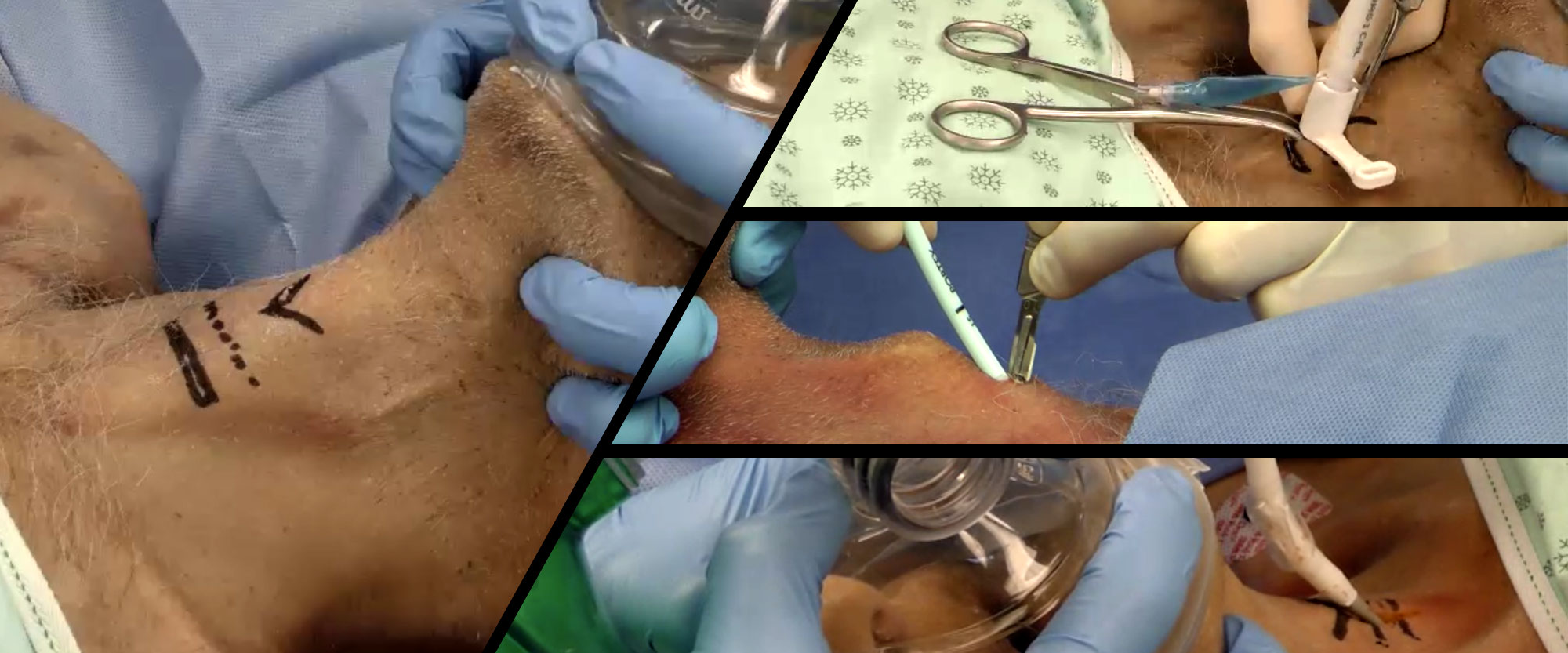
Front-of-neck airway rescue with impalpable anatomy during a simulated cannot intubate, cannot oxygenate scenario: scalpel-finger-cannula versus scalpel-finger-bougie in a sheep model
Heard A. et All. Br J Anaesth. 2020 Aug;125(2):184-191.----------------
Une situation au final rare mais c'est pour ce genre d'évènements qu'un médecin ENTRAÎNE est sur place. C'est clair.
Background: Front-of-neck airway rescue in a cannot intubate, cannot oxygenate (CICO) scenario with impalpable anatomy is particularly challenging. Several techniques have been described based on a midline vertical neck incision with subsequent finger dissection, followed by either a cannula or scalpel puncture of the now palpated airway. We explored whether the speed of rescue oxygenation differs between these techniques.
Methods: In a high-fidelity simulation of a CICO scenario in anaesthetised Merino sheep with impalpable front-of-neck anatomy, 35 consecutive eligible participants undergoing airway training performed scalpel-finger-cannula and scalpel-finger-bougie in a random order. The primary outcome was time from airway palpation to first oxygen delivery. Data, were analysed with Cox proportional hazards.
Results: Scalpel-finger-cannula was associated with shorter time to first oxygen delivery on univariate (hazard ratio [HR]=11.37; 95% confidence interval [CI], 5.14-25.13; P<0.001) and multivariate (HR=8.87; 95% CI, 4.31-18.18; P<0.001) analyses. In the multivariable model, consultant grade was also associated with quicker first oxygen delivery compared with registrar grade (HR=3.28; 95% CI, 1.36-7.95; P=0.008).
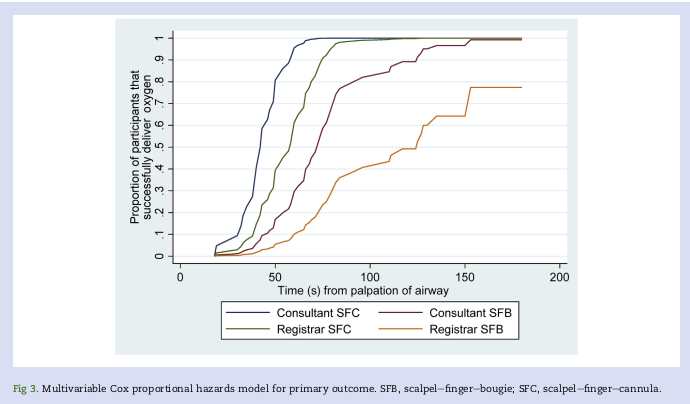
With scalpel-finger-cannula, successful oxygen delivery within 3 min of CICO declaration and ≤2 attempts was more frequent; 97% vs 63%, P<0.001. In analyses of successful cases only, scalpel-finger-cannula resulted in earlier improvement in arterial oxygen saturations (-25 s; 95% CI, -35 to -15; P<0.001), but a longer time to first capnography reading (+89 s; 95% CI, 69 to 110; P<0.001). No major complications occurred in either arm.
Conclusions: The scalpel-finger-cannula technique was associated with superior oxygen delivery performance during a simulated CICO scenario in sheep with impalpable front-of-neck anatomy.
| Tags : airway
20/01/2020
Vidéos de cricothyroïdotomie de l'Université de Sherbrooke
21/12/2019
Crico Chir:Plutôt avec 1 bougie ?
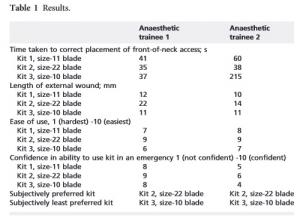
Randomized Comparative Assessment of Three Surgical Cricothyrotomy Devices on Airway Mannequins.
-------------------------------------------------
Un travail qui met en avant l'intérêt de l'emploi d'une bougie, l'importance de l'entraînement pour cette procédure peu fréquemmment réaloisée et le recul nécessaire à avoir envers les nouveaux équipements , en l'occurence le control-cric, fussent ils promus par le TCCC.
-------------------------------------------------
Background:
Airway obstruction is the second leading cause of preventable battlefield death, at least in part because surgical cricothyrotomy (SC) failure rates remain unacceptably high. Ideally, SC should be a rapid, simple, easily-learned, and reliably-performed procedure. Currently, 3 SC devices meet Tactical Combat Casualty Care (TCCC) standards: The Tactical CricKit® (TCK), Control-CricTM(CC), and Bougie-assisted Technique (BAT). However, no previous studies have compared these devices in application time, application success, user ratings, and user preference.
Methods:
United States Navy Corpsmen (N = 25) were provided 15 minutes of standardized instruction, followed by hands-on practice with each device on airway mannequins. Participants then performed SC with each of the 3 devices in a randomly assigned sequence. In this within-subjects design, application time, application success, participant ratings, and participant preference data were analyzed using repeated-measures ANOVA, regression, and non-parametric statistics at p < 0.05.
Results:
Application time for CC (M = 184 sec, 95% CI 144-225 sec) was significantly slower than for BAT (M = 135 sec, 95% CI 113-158 sec, p < 0.03) and TCK (M = 117 sec, 95% CI 93-142 sec, p < 0.005). Success was significantly greater for BAT (76%) than for TCK (40%, p < 0.02) and trended greater than CC (48%, p = 0.07). CC was rated significantly lower than TCK and BAT in ease of application, effectiveness, and reliability (each p < 0.01). User preference was significantly (p < 0.01) higher for TCK (58%) and BAT (42%) than for CC (0%). Improved CC blade design was the most common user suggestion.
Conclusion:
While this study was limited by the use of mannequins in a laboratory environment, present results indicate that none of these devices was ideal for performing SC. Based on slow application times, low success rates, and user feedback, the Control-CricTM cannot be recommended until improvements are made to the blade design
| Tags : coniotomie
07/10/2019
Membrane cricoïdienne à (0.13xP kg) + 0.86 mm
Depth to the airway lumen at the level of the cricothyroid membrane measured by ultrasound.
BACKGROUND:
Knowing the likely depth to the airway before emergency cricothyroidotomy may improve success in cases where it cannot be measured. Our aim was to measure the depth to the airway at the cricothyroid membrane by ultrasound in a large group of adult patients.
METHOD:
Prospective, observational study in two centres, Oxford and Gloucester. Patients presenting for a large variety of surgical operations were studied. Patients under 18 years old; pregnant; critically ill; had a history of neck surgery not included. Ultrasound examination was performed pre-operatively while participants lay supine with their head and neck extended, with light transducer pressure. We measured depth to the airway lumen in mm; age; weight; height and sex.
RESULTS:
In total 352 patients were studied. We found that depth to the airway lumen strongly correlated with weight (r=0.855, p<0.001) and to a lesser extent body mass index (r=0.781, p<0.001) but did not correlate to sex. Statistical analysis produced an equation to predict upper 95% CI of depth to the airway from the patient's weight: Depth to the airway lumen in mm = (0.13 x weight in kg) + 0.86.
CONCLUSIONS:
If ultrasound measurement is not possible before emergency cricothyroidotomy, the clinician could use our results to predict the depth to the airway by using the patient's weight. If the upper 95% CI were used as the depth of incision, it would enter the airway in 39 out of 40 patients of that weight, without damage to posterior structures in those with a shallower airway.
26/07/2019
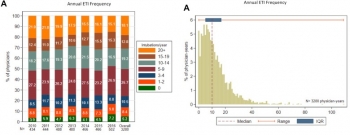
Maîtriser l'intubation: Un vrai challenge
Procedural Experience With Intubation: Results From a National Emergency Medicine Group.
---------------------------------
Un geste à laquelle les médecins urgentistes US sont peu exposés dans leur pratique quotidienne. Un vrai challenge personnel et pour les formateurs notamment des centres de simulations.
---------------------------------
STUDY OBJECTIVE:
Although intubation is a commonly discussed procedure in emergency medicine, the number of opportunities for emergency physicians to perform it is unknown. We determine the frequency of intubation performed by emergency physicians in a national emergency medicine group.
METHODS:
Using data from a national emergency medicine group (135 emergency departments [EDs] in 19 states, 2010 to 2016), we determined intubation incidence per physician, including intubations per year, intubations per 100 clinical hours, and intubations per 1,000 ED patient visits. We report medians and interquartile ranges (IQRs) for estimated intubation rates among emergency physicians working in general EDs (those treating mixed adult and pediatric populations).
RESULTS:
We analyzed 53,904 intubations performed by 2,108 emergency physicians in general EDs (53,265 intubations) and pediatric EDs (639 intubations). Intubation incidence varied among general ED emergency physicians (median 10 intubations per year; IQR 5 to 17; minimum 0, maximum 109). Approximately 5% of emergency physicians did not perform any intubations in a given year. During the study, 24.1% of general ED emergency physicians performed fewer than 5 intubations per year (range 21.2% in 2010 to 25.7% in 2016).
Emergency physicians working in general EDs performed a median of 0.7 intubations per 100 clinical hours (IQR 0.3 to 1.1) and 2.7 intubations per 1,000 ED patient visits (IQR 1.2 to 4.6).
CONCLUSION:
These findings provide insights into the frequency with which emergency physicians perform intubations.
25/07/2019
Crico: Plutôt une lame de 20 ?
Scalpel bougie tube versus hook-assisted emergency front of neck airway—a prospective randomised bench top study in porcine larynges
Caulfield K. et Al. https://doi.org/10.1016/j.bja.2019.05.017
Cette lettre a pour objet de comparer l'insertion d'une canule au travers de la membrane crico-thyroidienne d'un larynx de cochon (membrane que l'on sait relativement profonde) soit en utilisant un crochet de Hook soit une bougie. Les deux techniques se valent. Chose intéressante ils observent près de 17% de difficultés d'insertion avec une lame de 10 versus 7% avec une lame de 20. Cette dernière, qui est une version XL de la lame 10, semble donc préférable ?

"...In the Phase 1 study, the maximum sized ET tube to be placed into the CTM was a size 8. Time to insertion of ET tube averaged 30 s using a Size 20 blade and 31 s using a size 10 blade for all ETT sizes. There was a 16% recorded difficulty by candidates with the size 10 blade and only 7.5% recorded difficulty with the size 20 blade. In the Phase 2 study (blinded RCT), all attempted eFONA attempts were ultimately successful. There were no differences in time required, proportion successful in less than 40 s, or perceived difficulty between groups. Neither CTM incision width nor the proportion of attempts requiring re-incision was different between groups. Reassuringly, all eFONA attempts with both techniques were successful. Neither technique outperformed the other in any aspect of performance."
05/05/2019
Pour savoir, se ets'in/former
The effectiveness of educational methods for cricothyroid membrane identification by dental students: A prospective study using neck photographs and tracheotomy trainers.
Goto T et Al. Clin Exp Dent Res. 2019 Mar 4;5(2):170-177.
The purpose of this study was to evaluate the accurate identification of the cricothyroid membrane (CTM) by fifth grade dental students, before undergoing the relevant anesthesiology practicum. Moreover, we aimed to determine the educational effectiveness of the cricothyrotomy practicum in anesthesiology.
Before the lecture and without prior notification, 119 students were provided with a photograph of a man's neck and instructed to attach a blue sticker to the cricothyrotomy puncture site and to a palpable tracheotomy trainer, after applying sufficient palpation. After this, students attended a 60-min lecture on the emergency airway management method. Two and 16 days after the lecture and practicum, students were presented with a new neck photograph and the tracheotomy trainer and asked again to place stickers (red stickers: at 2 days; green stickers: at 16 days) on the cricothyrotomy penetration site. The data were analyzed with an image processing software, by superimposing the 119 stickers on the neck photographs and tracheotomy trainers, to visually examine the accuracy of CTM identification.
The rate of correct sticker placement in the neck photographs was 41.2% before the lecture, 80.7% 2 days after the lecture, and 77.3% 16 days after the lecture (before vs. 2 and 16 days after, p value < 0.01). For the tracheotomy trainer, the rate was 36.1% before the lecture, 97.5% 2 days after the lecture, and 94.1% 16 days after the lecture (before vs. 2 and 16 days after, p value < 0.01).
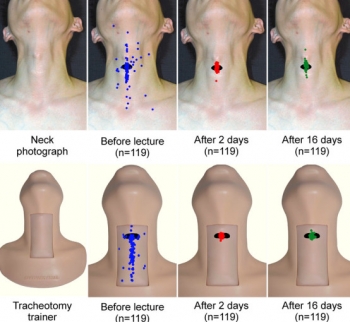
Furthermore, the proportion of students with mistakes above and below the CTM was higher than that of students with mistakes to the right or left. In conclusion, the rate of accurate CTM identification among dental students was low before they underwent the relevant practicum, but most students were able to identify the CTM accurately after the lecture and practicum in a small class.
16/04/2019
Coniotomie: Plutôt une lame de 22
Front-of-neck access technique and scalpels
Clic sur l'image pour accéder au document
| Tags : airway
07/04/2019
ControlCric: Plutôt à éviter
Necessity to depict difficult neck anatomy for training of cricothyroidotomy: A pilot study evaluating two surgical devices on a new hybrid training model.
BACKGROUND:
Everyone dealing with airway emergencies must be able to accomplish cricothyroidotomy, which cannot be trained in real patients. Training models are necessary.
OBJECTIVE:
To evaluate the suitability of a hybrid training model combining synthetic and porcine parts to depict variable neck anatomy.
DESIGN:
Model-based comparative trial.
SETTING:
Armed Forces Hospital Ulm, Germany, August 2018.
INTERVENTION:
On four anatomical neck variations (long slim/long obese/short slim/short obese) we performed two surgicalrapproaches to cricothyroidotomy (SurgiCric II vs. ControlCric).
PARTICIPANTS:
Forty-eight volunteers divided into two groups based on their personal skill level: beginners group and proficient performers group.
MAIN OUTCOME MEASURES:
Time to completion was recorded for each procedure. Once the operator had indicated completion, the correct anatomical tube placement was confirmed by dissection and structures were inspected for complications. Primary outcomes were successful tracheal placement of an airway tube and time needed to achieve a patent airway. Secondary outcome was assessment of complications.
RESULTS:
Overall, 384 procedures were performed. Median time to completion was 74 s. In total, 284 procedures (74%) resulted in successful ventilation. Time to completion was longer in short obese than in long slim and the risk of unsuccessful procedures was increased in short obese compared with long slim. Even if ControlCric resulted in faster completion of the procedure, its use was less successful and had an increased risk of complications compared with SurgiCric II. Proficient performers group performed faster but had an increased risk of injuring the tracheal wall compared with beginners group.
CONCLUSION:
Participants had difficulties in performing cricothyroidotomy in obese models, but various and difficult anatomical situations must be expected in airway management and therefore must be taught. A new hybrid model combining porcine and synthetic materials offers the necessary conditions for the next step in training of surgical airway procedures.