12/11/2017
Lunettes de vision nocturne: Une aide ? A voir !
-----------------------------------
Des résultats bien étonnants quand on connait les problèmes de profondeur de champ inhérents à l'emploi de dispositifs de vision nocturne, surtout monoculaires. Comme toujours maîtriser le geste en conditions normales, maîtriser l'outil de vision et s'entraîner dans ces conditions. Lire également 1, 2, 3
-----------------------------------
BACKGROUND:
In the patients with multiple and serious trauma, early applications of life-saving procedures are related to improved survival. We tried to experimentally determine the feasibility of life-saving interventions that are performed with the aid of night vision goggles (NVG) in nighttime combat scenario.
METHODS:
Chest tube thoracostomy (CTT), emergency cricothyroidotomy (EC), and needle thoracostomy (NT) interventions were performed by 10 combatant medical staff. The success and duration of interventions were explored in the study. Procedures were performed on the formerly prepared manikins/models in a bright room and in a dark room with the aid of NVG. Operators graded the ease of interventions.
RESULTS:
All interventions were found successful. Operators stated that both CTT and EC interventions were more difficult in dark than in daytime (p<0.05). No significant difference was observed in the difficulty in the NT interventions. No significant difference was observed in terms of completion times of interventions between in daytime and in dark scenario.
CONCLUSION:
The operators who use NVGs have to be aware of that they can perform their tactic and medical activities without taking off the NVGs and without the requirement of an extra light source.
| Tags : vision nocturne
10/11/2017
Formation des personnels des FS: Réflexions OTAN
11/10/2017
Numéro Spécial SSA
06/09/2017
Wilderness medicine: Numéro spécial
05/05/2017
TCCC. Point sur la recherche US
05/03/2017
Prolonged field care: Un retex
| Tags : prolonged field care
18/12/2016
Coagulopathie traumatique. Données actuelles
Acute traumatic coagulopathy: pathophysiology and resuscitation.
Acute Traumatic Coagulopathy occurs immediately after massive trauma when shock, hypoperfusion, and vascular damage are present. Mechanisms for this acute coagulopathy include activation of protein C, endothelial glycocalyx disruption, depletion of fibrinogen, and platelet dysfunction. Hypothermia and acidaemia amplify the endogenous coagulopathy and often accompany trauma. These multifactorial processes lead to decreased clot strength, autoheparinization, and hyperfibrinolysis. Furthermore, the effects of aggressive crystalloid administration, haemodilution from inappropriate blood product transfusion, and prolonged surgical times may worsen clinical outcomes. We review normal coagulation using the cell-based model of haemostasis and the pathophysiology of acute traumatic coagulopathy. Developed trauma systems reduce mortality, highlighting critical goals for the trauma patient in different phases of care. Once patients reach a trauma hospital, certain triggers reliably indicate when they require massive transfusion and specialized trauma care. These triggers include base deficit, international normalized radio (INR), systolic arterial pressure, haemoglobin concentration, and temperature. Early identification for massive transfusion is critically important, as exsanguination in the first few hours of trauma is a leading cause of death. To combat derangements caused by massive haemorrhage, damage control resuscitation is a technique that addresses each antagonist to normal haemostasis. Components of damage control resuscitation include damage control surgery, permissive hypotension, limited crystalloid administration, haemostatic resuscitation, and correction of hyperfibrinolysis.
11/12/2016
Suppression métabolique ?
Inducing metabolic suppression in severe hemorrhagic shock: Pilot study results from the Biochronicity Project.
BACKGROUND:
Suspended animation-like states have been achieved in small animal models, but not in larger species. Inducing metabolic suppression and temporary oxygen independence could enhance survivability of massive injury. Based on prior analyses of key pathways, we hypothesized that phosphoinositol-3-kinase inhibition would produce metabolic suppression without worsening organ injury or systemic physiology.
METHODS:
Twenty swine were studied using LY294002 (LY), a nonselective phosphoinositol-3-kinase inhibitor. Animals were assigned to trauma only (TO, n = 3); dimethyl sulfoxide only (DMSO, n = 4), LY drug only (LYO, n = 3), and drug + trauma (LY + T, n = 10) groups. Both trauma groups underwent laparotomy, 35% hemorrhage, severe ischemia/reperfusion injury, and protocolized resuscitation. Laboratory, physiologic, cytokine, and metabolic cart data were obtained. Histology of key end organs was also compared.
RESULTS:
Baseline values were similar among the groups. Compared with the TO group, the LYO group had reversible decreases in heart rate, mean arterial pressure, cardiac output, oxygen consumption, and carbon dioxide production. Compared with TO, LY + T showed sustained decreases in heart rate (113 vs. 76, p = 0.03), mean arterial pressure (40 vs. 31 mm Hg, p = 0.02), and cardiac output (3.8 vs. 1.9 L/min, p = 0.05) at 6 hours. Metabolic parameters showed profound suppression in the LY + T group. Oxygen consumption in LY + T was lower than both TO (119 vs. 229 mL/min, p = 0.012) and LYO (119 vs. 225 mL/min, p = 0.014) at 6 hours. Similarly, carbon dioxide production was decreased at 6 hours in LY + T when compared with TO (114 vs. 191 mL/min, p = 0.043) and LYO (114 vs. 195 mL/min, p = 0.034) groups. There was no worsening of acidosis (lactate 6.4 vs. 8.3 mmol/L, p = 0.4) or other endpoints. Interleukin 6 (IL-6) showed a significant increase in LY + T when compared with TO at 6 hours (60.5 vs. 2.47, p = 0.043). Tumor necrosis factor α and IL-1β were decreased, and IL-10 increased in TO and LY + T at 6 hours. Markers of liver and kidney injury were no different between TO and LY + T groups at 6 hours.
CONCLUSIONS:
Phosphoinositol-3-kinase inhibition produced metabolic suppression in healthy and injured swine without increasing end-organ injury or systemic physiologic markers and demonstrated prolonged efficacy in injured animals. Further study may lead to targeted therapies to prolong tolerance to hemorrhage and extend the "golden hour" for injured patients.
10/12/2016
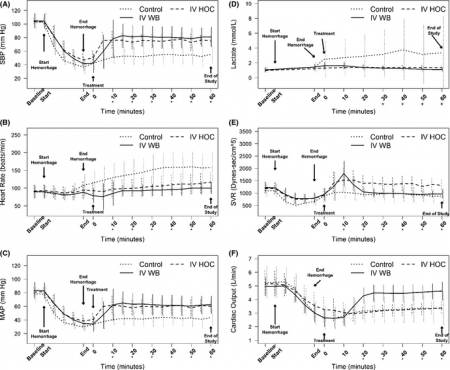
Maintenir la pression: Hydroxocobalamine ou adré ?
A prospective, randomized trial of intravenous hydroxocobalamin versus whole blood transfusion compared to no treatment for Class III hemorrhagic shock resuscitation in a prehospital swine model.
OBJECTIVES:
The objective was to compare systolic blood pressure (sBP) over time in swine that have had 30% of their blood volume removed (Class III shock) and treated with intravenous (IV) whole blood or IV hydroxocobalamin, compared to nontreated controlanimals.
METHODS:
Thirty swine (45 to 55 kg) were anesthetized, intubated, and instrumented with continuous femoral and pulmonary artery pressure monitoring. Animals were hemorrhaged a total of 20 mL/kg over a 20-minute period. Five minutes after hemorrhage, animals were randomly assigned to receive 150 mg/kg IV hydroxocobalamin solubilized in 180 mL of saline, 500 mL of whole blood, or no treatment. Animals were monitored for 60 minutes thereafter. A sample size of 10 animals per group was determined based on a power of 80% and an alpha of 0.05 to detect an effect size of at least a 0.25 difference (>1 standard deviation) in mean sBP between groups. sBP values were analyzed using repeated-measures analysis of variance (RANOVA). Secondary outcome data were analyzed using repeated-measures multivariate analysis of variance (RMANOVA).
RESULTS:
There were no significant differences between hemodynamic parameters of IV hydroxocobalamin versus whole blood versus control group at baseline (MANOVA; Wilks' lambda; p = 0.868) or immediately posthemorrhage (mean sBP = 47 mm Hg vs. 41 mm Hg vs. 37 mm Hg; mean arterial pressure = 39 mm Hg vs. 28 mm Hg vs. 34 mm Hg; mean serum lactate = 1.2 mmol/L vs. 1.4 mmol/L vs. 1.4 mmol/L; MANOVA; Wilks' lambda; p = 0.348). The outcome RANOVA model detected a significant difference by time between groups (p < 0.001). Specifically, 10 minutes after treatment, treated animals showed a significant increase in mean sBP compared to nontreated animals (mean sBP = 76.3 mm Hg vs. 85.7 mm Hg vs. 51.1 mm Hg; p < 0.001). RMANOVA modeling of the secondary data detected a significant difference in mean arterial pressure, heart rate, and serum lactate (p < 0.001). Similar to sBP, 10 minutes after treatment, treated animals showed a significant increase in mean arterial pressure compared to nontreated animals (mean arterial pressure = 67.7 mm Hg vs. 61.4 mm Hg vs. 40.5 mm Hg). By 10 minutes, mean heart rate was significantly slower in treated animals compared to nontreated animals (mean heart rate = 97.3 beats/min vs. 95.2 beats/min vs. 129.5 beats/min; p < 0.05). Serum lactate, an early predictor of shock, continued to rise in the control group, whereas it did not in treated animals. Thirty minutes after treatment, serum lactate values of treated animals were significantly lower compared to nontreated animals (p < 0.05). This trend continued throughout the 60-minute observation period such that 60-minute values for lactate were 1.4 mmol/L versus 1.1 mmol/L versus 3.8 mmol/L. IV hydroxocobalamin produced a statistically significant increase in systemic vascular resistance compared to control, but not whole blood, with a concomitant decrease in cardiac output.
CONCLUSIONS:
Intravenous hydroxocobalamin was more effective than no treatment and as effective as whole blood transfusion, in reversing hypotension and inhibiting rises in serum lactate in this prehospital, controlled, Class III swine hemorrhage model.
| Tags : choc
24/09/2016
Transfusion en vol: Sécurité assurée
Risk Management Analysis of Air Ambulance Blood Product Administration in Combat Operations
BACKGROUND:
Between June-October 2012, 61 flight-medic-directed transfusions took place aboard U.S. Army Medical Evacuation (medevac) helicopters in Afghanistan. This represents the initial experience for pre-hospital blood product transfusion by U.S. Army flight medics.
METHODS:
We performed a retrospective review of clinical records, operating guidelines, after-action reviews, decision and information briefs, bimonthly medical conferences, and medevac-related medical records.
RESULTS:
A successful program was administered at 10 locations across Afghanistan. Adherence to protocol transfusion indications was 97%. There were 61 casualties who were transfused without any known instance of adverse reaction or local blood product wastage. Shock index (heart rate/systolic blood pressure) improved significantly en route, with a median shock index of 1.6 (IQR 1.2-2.0) pre-transfusion and 1.1 (IQR 1.0-1.5) post-transfusion (P < 0.0001). Blood resupply, training, and clinical procedures were standardized across each of the 10 areas of medevacoperations.
DISCUSSION:
Potential risks of medical complications, reverse propaganda, adherence to protocol, and diversion and/or wastage of limited resources were important considerations in the development of the pilot program. Aviation-specific risk mitigation strategies were important to ensure mission success in terms of wastage prevention, standardized operations at multiple locations, and prevention of adverse clinical outcomes. Consideration of aviation risk mitigation strategies may help enable other helicopter emergency medical systems to develop remote pre-hospital transfusion capability. This pilot program provides preliminary evidence that blood product administration by medevac is safe.
| Tags : transfusion
22/09/2016
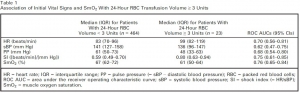
SmO2: Utile ?
Muscle Oxygen Saturation Improves Diagnostic Association Between Initial Vital Signs and Major Hemorrhage: A Prospective Observational Study.
L'hémorragie reste la cause principale des décès évitable et l'importance de la mise en oeuvre d'une stratégie transfusionnelle précoce est actée. Mais sur quels critères. Au delà des critères cliniques simples, on peut citer le recours au suivi des lactates. Le suivi de paramètres d'oxygénation tissulaire simple est maintenant possible. Ce qu'évoque ce document est l'emploi de la SmO2, élément déjà utilisé en médecine du sport. Le recours à un tel paramètre est donc potentiellement très intéressant si cette pertinence était confirmée et sa mesure valide avec des outils simples.
OBJECTIVES:
During initial assessment of trauma patients, vital signs do not identify all patients with life-threatening hemorrhage. We hypothesized that a novel vital sign, muscle oxygen saturation (SmO2 ), could provide independent diagnostic information beyond routine vital signs for identification of hemorrhaging patients who require packed red blood cell (RBC) transfusion.
METHODS:
This was an observational study of adult trauma patients treated at a Level I trauma center. Study staff placed the CareGuide 1100 tissue oximeter (Reflectance Medical Inc., Westborough, MA), and we analyzed average values of SmO2 , systolic blood pressure (sBP), pulse pressure (PP), and heart rate (HR) during 10 minutes of early emergency department evaluation. We excluded subjects without a full set of vital signs during the observation interval. The study outcome was hemorrhagic injury and RBC transfusion ≥ 3 units in 24 hours (24-hr RBC ≥ 3). To test the hypothesis that SmO2 added independent information beyond routine vital signs, we developed one logistic regression model with HR, sBP, and PP and one with SmO2 in addition to HR, sBP, and PP and compared their areas under receiver operating characteristic curves (ROC AUCs) using DeLong's test.
RESULTS:
We enrolled 487 subjects; 23 received 24-hr RBC ≥ 3. Compared to the model without SmO2 , the regression model with SmO2 had a significantly increased ROC AUC for the prediction of ≥ 3 units of 24-hr RBC volume, 0.85 (95% confidence interval [CI], 0.75-0.91) versus 0.77 (95% CI, 0.66-0.86; p < 0.05 per DeLong's test). Results were similar for ROC AUCs predicting patients (n = 11) receiving 24-hr RBC ≥ 9.
CONCLUSIONS:
SmO2 significantly improved the diagnostic association between initial vital signs and hemorrhagic injury with blood transfusion. This parameter may enhance the early identification of patients who require blood products for life-threatening hemorrhage.
01/09/2016
Médecine de catastrophe en France
27/08/2016
Interventions salvatrices: Bien sûr mais lesquelles ?
Major incident triage: A consensus based definition of the essential life-saving interventions during the definitive care phase of a major incident
Vassallo J. et Al. Injury, Int. J. Care Injured 47 (2016) 1898–190
-------------------------
Plus le contexte d'intervention est difficile soit du fait de l'environnement soit du fait du danger tactique et plus le choix des nterventions médicales doit être réflechi et restreint et mis en oeuvre par uintervenant pas forcément médecin mas formé spécifiquement à la pratique d'une action nécessaire à la survie. Ce travail identiife ainsi une trentaine de conduites essentielles à un réseau de traumatisés graves. Lire aussi cet article
-------------------------
Introduction: Triage is a key principle in the effective management of major incidents. The process currently relies on algorithms assigning patients to specific triage categories; there is, however, little guidance as to what these categories represent. Previously, these algorithms were validated against injury severity scores, but it is accepted now that the need for life-saving intervention is a more important outcome. However, the definition of a life-saving intervention is unclear. The aim of this study was to define what constitutes a life-saving intervention, in order to facilitate the definition of an adult priority one patient during the definitive care phase of a major incident.
Methods: We conducted a modified Delphi study, using a panel of subject matter experts drawn from the United Kingdom and Republic of South Africa with a background in Emergency Care or Major Incident Management. The study was conducted using an online survey tool, over three rounds between July and December 2013. A four point Likert scale was used to seek consensus for 50 possible interventions, with a consensus level set at 70%.
Results: 24 participants completed all three rounds of the Delphi, with 32 life-saving interventions reaching consensus.
Conclusions: This study provides a consensus definition of what constitutes a life-saving intervention in the context of an adult, priority one patient during the definitive care phase of a major incident. The definition will contribute to further research into major incident triage, specifically in terms of validation of an adult major incident triage tool.
| Results of the Delphi Process – Life-Saving Interventions. | |
| 1 | Intubation for actual airway obstruction |
| 2 | Intubation for impending airway obstruction |
| 3 | Surgical airway for airway obstruction |
| 4 | Surgical airway for impending airway obstruction |
| 5 | Needle thoracocentesis |
| 6 | Finger thoracostomy |
| 7 | Tube thoracostomy |
| 8 | Application of a chest seal (commercial/improvised) |
| 9 | Positive Pressure Ventilation for ventilatory inadequacy |
| 10 | Application of a tourniquet for haemorrhage control |
| 11 | Use of haemostatic agents for haemorrhage control |
| 12 | Insertion of an intra-osseous device for resuscitation purposes |
| 13 | Receiving uncross-matched blood |
| 14 | Receiving≥4 units of blood/blood products |
| 15 | Administration of tranexamic acid |
| 16 | Laparotomy for trauma |
| 17 | Thoracotomy for trauma |
| 18 | Pericardial window for trauma |
| 19 | Surgery to gain proximal vascular control |
| 20 | Interventional radiology for haemorrhage control |
| 21 | Application of a pelvic binder |
| 22 | ALS/ACLS protocols for a patient in a peri-arrest situation |
| 23 | ALS/ACLS protocols for a patient in cardiac arrest |
| 24 | Neurosurgery for the evacuation of an intra-cranial haematoma |
| 25 | Craniotomy |
| 26 | Burr Hole Insertion |
| 27 | Spinal nursing for a C1-3 fracture |
| 28 | Administration of a seizure-terminating medication |
| 29 | Active rewarming for initial core temp<32° celcius |
| 30 | Passive rewarming for initial core temp<32° celcius |
| 31 | Correction of low blood glucose |
| 32 | Administration of chemical antidotes |
| Tags : triage
11/08/2016
Transfusion, Thrombosis and Bleeding Management
Special Issue: Transfusion, Thrombosis and Bleeding Management
January 2015 - Volume 70, Issue Supplement s1 - Pages 1–e41
Clic sur l'image pour accéder au numéro en ligne
Blood – the most important humour? (pages 1–e1)
C. R. Bailey, A. A. Klein and B. J. Hunt
Version of Record online: 1 DEC 2014 | DOI: 10.1111/anae.12930
Review Articles
L. Green, S. Allard and R. Cardigan
☛ CPD available at http://www.learnataagbi.org
Corrected by:
Corrigendum: Modern banking, collection, compatibility testing and storage of blood and blood components
Vol. 70, Issue 3, 373, Version of Record online: 11 FEB 2015
Evidence and triggers for the transfusion of blood and blood products (pages 10–e3)
A. Shah, S. J. Stanworth and S. McKechnie
Pre-operative anaemia (pages 20–e8)
B. Clevenger and T. Richards
The pathophysiology and consequences of red blood cell storage (pages 29–e12)
D. Orlov and K. Karkouti
Red cell transfusion and the immune system (pages 38–e16)
S. Hart, C. M. Cserti-Gazdewich and S. A. McCluskey
The current place of aprotinin in the management of bleeding (pages 46–e17)
D. Royston
The current place of tranexamic acid in the management of bleeding (pages 50–e18)
B. J. Hunt
Practical management of major blood loss (pages 54–e20)
R. Gill
Management of peri-operative anti-thrombotic therapy (pages 58–e23)
J. J. van Veen and M. Makris
Laboratory monitoring of haemostasis (pages 68–e24)
A. Fowler and D. J. Perry
Point-of-care monitoring of haemostasis (pages 73–e26)
S. V. Mallett and M. Armstrong
Haemostatic management of obstetric haemorrhage (pages 78–e28)
R. E. Collis and P. W. Collins
Haemostatic management of cardiac surgical haemorrhage (pages 87–e31)
M. W. Besser, E. Ortmann and A. A. Klein
The pathogenesis of traumatic coagulopathy (pages 96–e34)
A. Cap and B. J. Hunt
Management of traumatic haemorrhage – the European perspective (pages 102–e37)
H. Schöchl, W. Voelckel and C. J. Schlimp
Management of traumatic haemorrhage – the US perspective (pages 108–e38)
R. P. Dutton
Surgery in patients with inherited bleeding disorders (pages 112–e40)
P. K. Mensah and R. Gooding
The management of abnormal haemostasis in the ICU (pages 121–e41)
A. Retter and N. A. Barrett
31/07/2016
Revue du CIMM/ICMM
29/06/2016
Afghanistan et le bilan hollandais
27/06/2016
The Trauma Manual: Trauma and Acute Care Surgery
Trauma anesthesia
14/06/2016
Combat Trauma. Lessons Learned from Military Operations
13/06/2016
Can J Surg: Numéro spécial 2015
Foreword
Avant-Propos
Introduction
Commentaries
Review
Research
- Correction in:
- Can J Surg. 2015 Oct; 58(5): 317.
Discussions in Surgery




1365-2044/asset/olbannerleft.gif?v=1&s=bd83df57543a1d11ffc15f630bb1301f0be80859)