16/04/2019
FST, chirurgie et USAparticulièrement innovant
TCCC: Un écosystème spécifique
Un regard sur l'émergence des nouvelles modalités de prise en charge des blessés de guerre avec pour point d'orgue l'innovation conduite et la construction d'un écosystème complet autour de la prise en charge du blessé de guerre. Une démarche à comprendre et à bien méditer.
Clic sur l'image pour accéder au document
19/03/2019
ATLS 9ème Edition
13/12/2018
Rétrospective sur les missions du SSA
A lire pour avoir une image actualisée du SSA. Certes peine à la peine mais, fidèle à ses traditions, n'a manifestement pas chômé ses dernières années
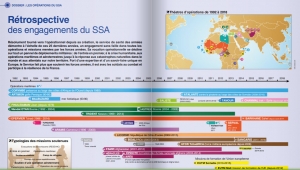
Clic sur l'image pour accéder à la publication
09/12/2018
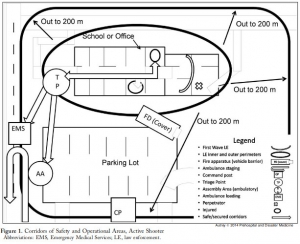
Tuerie massive: Les 30 premières min.
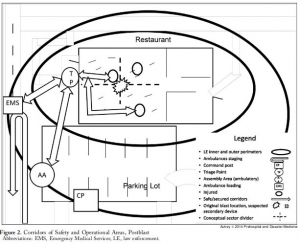
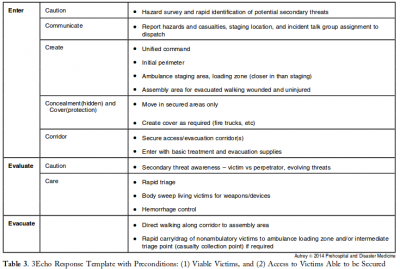
3 Echo: concept of operations for early care and evacuation of victims of mass violence
This report describes the successful use of a simple 3-phase approach that guides the initial 30 minutes of a response to blast and active shooter events with casualties: Enter, Evaluate, and Evacuate (3 Echo) in a mass-shooting event occurring in Minneapolis, Minnesota USA, on September 27, 2012. Early coordination between law enforcement (LE) and rescue was emphasized, including establishment of unified command, a common operating picture, determination of evacuation corridors, swift victim evaluation, basic treatment, and rapid evacuation utilizing an approach developed collaboratively over the four years prior to the event. Field implementation of 3 Echo requires multi-disciplinary (Emergency Medical Services (EMS), fire and LE) training to optimize performance.
This report details the mass-shooting event, the framework created to support the response, and also describes important aspects of the concepts of operation and curriculum evolved through years of collaboration between multiple disciplines to arrive at unprecedented EMS transport times in response to the event.
07/12/2018
K comme Killer ?
-----------------------------
K comme Killer ? Peut être pas, mais en tous cas plus fréquent que l'on croit.
-----------------------------
OBJECTIVE:
Fixed facilities and rapid global evacuation ensured that delayed complications of trauma, such as hyperkalemia, occurred late in the evacuation chain where renal replacement therapies were available. However, future conflicts or humanitarian disasters may involve prolonged evacuation times. We sought to quantify one potential risk of delayed evacuation by assessing hyperkalemia in combat casualties.
METHODS:
Retrospective study of military members admitted to intensive care units in Iraq and Afghanistan from February 1, 2002, to February 1, 2011. This study was approved by the U.S. Army Medical Research and Materiel Command Institutional Review Board. Demographics, injury severity score, burn injury, mechanism of injury, vital signs, creatinine, and potassium were collected. Logistic regression models were used to identify incidence and risk factors for hyperkalemia.
RESULTS:
Of 6,011 patient records, 1,472 had sufficient data to be included for analysis. Hyperkalemia occurred in 5.8% of patients. Those with hyperkalemia had higher injury severity scores, higher shock index, were more likely to have acute kidney injury, and were more likely to die. On multivariate analysis, acute kidney injury and shock index were significantly associated with the development of hyperkalemia. In a subgroup of patients with data on creatine kinase, rhabdomyolysis was associated with hyperkalemia in the univariate model, but was not significant after adjustment.
CONCLUSION:
Hyperkalemia occurred in 5.8% of patients in our cohort of critically injured combat casualties. The development of hyperkalemia was independently associated with acute kidney injury and shock index. In future conflicts, with prolonged evacuation times, mitigation strategies should be developed to treat hyperkalemia in casualties before arrival at definitive care.
01/11/2018
Combat urbain: Problématique
08/10/2018
Military Medicine: Numéro spécial 2018
25/09/2018
Intervenir sur une tuerie massive: Un savoir faire à acquérir
This report describes the successful use of a simple 3-phase approach that guides the initial 30 minutes of a response to blast and active shooter events with casualties: Enter, Evaluate, and Evacuate (3 Echo) in a mass-shooting event occurring in Minneapolis, Minnesota USA, on September 27, 2012. Early coordination between law enforcement (LE) and rescue was emphasized, including establishment of unified command, a common operating picture, determination of evacuation corridors, swift victim evaluation, basic treatment, and rapid evacuation utilizing an approach developed collaboratively over the four years prior to the event. Field implementation of 3 Echo requires multi-disciplinary (Emergency Medical Services (EMS), fire and LE) training to optimize performance.
This report details the mass-shooting event, the framework created to support the response, and also describes important aspects of the concepts of operation and curriculum evolved through years of collaboration between multiple disciplines to arrive at unprecedented EMS transport times in response to the event.
15/09/2018
Aggressions collectives par arme de guerre
10/09/2018
Settings standard for CCC
08/09/2018
Le TCCC dans la vraie vie
Survey of Casualty Evacuation Missions Conducted by the 160th Special Operations Aviation Regiment During the Afghanistan Conflict.
BACKGROUND:
Historically, documentation of prehospital combat casualty care has been relatively nonexistent. Without documentation, performance improvement of prehospital care and evacuation through data collection, consolidation, and scientific analyses cannot be adequately accomplished. During recent conflicts, prehospital documentation has received increased attention for point-of-injury care as well as for care provided en route on medical evacuation platforms. However, documentation on casualty evacuation (CASEVAC) platforms is still lacking. Thus, a CASEVAC dataset was developed and maintained by the 160th Special Operations Aviation Regiment (SOAR), a nonmedical, rotary-wing aviation unit, to evaluate and review CASEVAC missions conducted by their organization.
METHODS:
A retrospective review and descriptive analysis were performed on data from all documented CASEVAC missions conducted in Afghanistan by the 160th SOAR from January 2008 to May 2015. Documentation of care was originally performed in a narrative after-action review (AAR) format. Unclassified, nonpersonally identifiable data were extracted and transferred from these AARs into a database for detailed analysis. Data points included demographics, flight time, provider number and type, injury and outcome details, and medical interventions provided by ground forces and CASEVAC personnel.
RESULTS:
There were 227 patients transported during 129 CASEVAC missions conducted by the 160th SOAR. Three patients had unavailable data, four had unknown injuries or illnesses, and eight were military working dogs. Remaining were 207 trauma casualties (96%) and five medical patients (2%). The mean and median times of flight from the injury scene to hospital arrival were less than 20 minutes. Of trauma casualties, most were male US and coalition forces (n = 178; 86%). From this population, injuries to the extremities (n = 139; 67%) were seen most commonly. The primary mechanisms of injury were gunshot wound (n = 89; 43%) and blast injury (n = 82; 40%). The survival rate was 85% (n = 176) for those who incurred trauma. Of those who did not survive, most died before reaching surgical care (26 of 31; 84%).
CONCLUSION:
Performance improvement efforts directed toward prehospital combat casualty care can ameliorate survival on the battlefield. Because documentation of care is essential for conducting performance improvement, medical and nonmedical units must dedicate time and efforts accordingly. Capturing and analyzing data from combat missions can help refine tactics, techniques, and procedures and more accurately define wartime personnel, training, and equipment requirements. This study is an example of how performance improvement can be initiated by a nonmedical unit conducting CASEVAC missions.
06/06/2018
March: Aussi chez les chinois
Expert consensus on the evaluation and diagnosis of combat injuries of the Chinese People’s Liberation Army
30/01/2018
Golden hour: Un concept + qu'une obligation
20/01/2018
Queensland Clinical Practice Manual
17/01/2018
Guide de médecine rurale AUS
09/01/2018
A lire
Prolonged Field Care of a Casualty With Penetrating Chest Trauma Case Report
Barnhart G. et Al. J Spec Oper Med. Winter 2016;16(4):99-101
As Special Operations mission sets shift to regions with less coalition medical infrastructure, the need for quality long-term field care has increased. More and more, Special Operations Medics will be expected to maintain casualties in the field well past the "golden hour" with limited resources and other tactical limitations. This case report describes an extended-care scenario (>12 hours) of a casualty with a chest wound, from point of injury to eventual casualty evacuation and hand off at a Role II facility. This case demonstrates the importance of long-term tactical medical considerations and the effectiveness of minimal fluid resuscitation in treating penetrating thoracic trauma.
Histoire à lire
A Case of Prehospital Traumatic Arrest in a US Special Operations Soldier: Care From Point of Injury to Full Recovery
During an assault on an extremely remote target, a US Special Operations Soldier sustained multiple gunshot and fragmentation wounds to the thorax, resulting in a traumatic arrest and subsequent survival. His care, including care under fire, tactical field care, tactical evacuation care, and Role III, IV, and V care, is presented. The case is used to illustrate the complex dynamics of Special Operations care on the modern battlefield and the exceptional outcomes possible when evidence-based medicine is taken to the warfighter with effective,
13/11/2017
les "Brit" en Irak 2003
A quoi sert un médecin ?
The Role Of The Physician In Modern Military Operations: 12 Months Experience In Southern Iraq
Grainge C et Al. J R Army Med Corps 2005 151: 101-1
--------------------------------------
Vaste débat surtout pour nous français élevé à la sauce de l a médecine préhospitalière type SAMU. D'autres ont une vision bien différente qui, bien qu'elle évolue (1) avec le concept de "prolonged field care" - ie: une certaine médicalisation de l'avant -, n'est globalement pas remise en cause après les engagements US et UK en irak et en afghanistan. Dans ce travail il apparait que les problématiques d'hygiène et de médecine de prévention, le préhospitalier n'est pas mentionné, sont pour nos alliés anglais au coeur du rôle de leurs médecins. On rappelle juste qu'ils sont aussi les adeptes de MEDEVAC très performantes - les MERT-Enhanced (équipes composées d'un médecin anesthésiste ou urgentiste expérimenté en matière de trauma, d'un-e infirmier-ère, de deux paramedics et d'une équipe de protection oeuvrant dans un Chinook CH-47.
--------------------------------------
Objectives To examine the profile of medical morbidity and the role of the physician in modern conflict.
Methods Retrospective survey of admission records at a British Military Field Hospital on operational duty in Southern Iraq.
Results 62.5% of 4870 admissions to the Field Hospital in Shaibah during the first 12 months of military operations in Iraq were under the care of physicians. Of these 1531 (31.4%) were due to diarrhoea and vomiting (D&V) and 764 (15.7%) due to heat illness. The incidence of heat illness rose with ambient temperature, but soldiers were more likely to be admitted with heat illness shortly after arrival in theatre than when fully acclimatised. There was also a steady flow of admissions with a broad spectrum of medical pathology requiring the clinical skills of a general physician.
Conclusions A general physician is a necessary part of the clinical team in modern conflict. The incidence of D&V and of heat illness on military operations remains high. Planners for any operation in tropical climates should take this into consideration and put preventative measures into place early.