02/11/2024
Intraosseux: Passer l'os cortical
The relationship between intraosseous catheter tip placement, flow rates, and infusion pressures in a high bone density cadaveric swine (Sus scrofa) model
Gehrz JA et Al. J Am Coll Emerg Physicians Open. 2024 Jul 4;5(4):e13184.
Background: Intraosseous (IO) infusion is a life-preserving technique when intravenous access is unobtainable. Successful IO infusion requires sufficiently high flow rates to preserve life but at low enough pressures to avoid complications. However, IO catheter tips are often misplaced, and the relative flow rates and pressures between IO catheter tips placed in medullary, trabecular, and cortical bone are not well described, which has important implications for clinical practice.
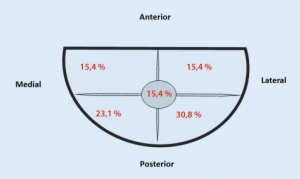
Objectives: We developed the Zone Theory of IO Catheter Tip Placement based on bone density and proximity to the venous central sinus and then tested the influence of catheter tip placement locations on flow rates and pressures in a cadaveric swine model.
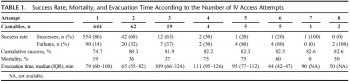
Methods: Three cross-trained participants infused 500 mL of crystalloid fluid into cadaveric swine humerus and sternum (N = 210 trials total) using a push‒pull method with a 60 cm3 syringe. Computed tomography scans were scored by radiologists and categorized as zone 1 (medullary space), zone 2 (trabecular bone), or zone 3 (cortical bone) catheter tip placements. Differences between zones in flow rates, mean pressures, and peak pressures were assessed using analysis of variance and analysis of covariance to account for participant and site differences at the p < 0.05 threshold.
Results: Zone 1 and zone 2 placements were essentially identical in flow rates, mean pressures, and peak pressures (each p > 0.05). Zone 1 and zone 2 placements were significantly higher in flow rates and lower in pressures than zone 3 placements (each p < 0.05 or less).
Flow rates by zone
Conclusion: Within the limitations of an unpressurized cadaveric swine model, the present findings suggest that IO catheter tip placements need not be perfect to acquire high flow rates at low pressures, only accurate enough to avoid the dense cortical bone of zone 3. Future research using in vivo animal and human models is needed to better define the clinical impact of IO catheter placement on infusion flow rates and pressures.
| Tags : i
21/10/2022
Plyo intraosseux ? Pas si simple
Intraosseous administration of freeze-dried plasma in the prehospital setting
Rittblat M et Al. Isr Med Assoc J. 2022 Sep;24(9):591-595.
Background:
Freeze dried plasma (FDP) is a commonly used replacement fluid in the prehospital setting when blood products are unavailable. It is normally administered via a peripheral intravenous (PIV) line. However, in severe casualties, when establishing a PIV is difficult, administration via intraosseous vascular access is a practical alternative, particularly under field conditions.
Objectives:
To evaluate the indications and success rate of intraosseous administration of FDP in casualties treated by the Israel Defense Forces (IDF).
Methods:
A retrospective analysis of data from the IDF-Trauma Registry was conducted. It included all casualties treated with FDP via intraosseous from 2013 to 2019 with additional data on the technical aspects of deployment collected from the caregivers of each case.
Results:
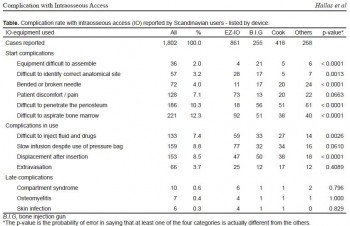
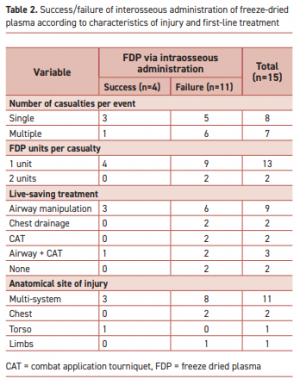
Of 7223 casualties treated during the study period, intravascular access was attempted in 1744; intraosseous in 87 of those. FDP via intraosseous was attempted in 15 (0.86% of all casualties requiring intravascular access). The complication rate was 73% (11/15 of casualties).
"According to the manufacturer’s specifications, the reconstituted lyophilized plasma product is delivered from a glass bottle with the rate of infusion determined primarily by gravity. This procedure precludes the care providers from applying external pressure to increase the plasma infusion rate. Therefore, the pressure gradient is determined primarily by gravity with respect to height of the bottle."
Complications were more frequent when the event included multiple casualties or when the injury included multiple organs. Of the 11 failed attempts, 5 were reported as due to slow flow of the FDP through the intraosseous apparatus. Complications in the remaining six were associated with deployment of the intraosseous device.
Conclusions:
Administration of FDP via intraosseous access in the field requires a high skill level.
| Tags : intraosseux
11/03/2020
Le SAM IO
SAM medical propose un nouveau dispositif d'abord intraosseux. Peut être un concurrent à l'EZ_IO
| Tags : intraosseux
19/10/2018
Pour voir: Etre dans le bleu!
Safest light in a combat area while performing intravenous access in the dark.
INTRODUCTION:
Cannulation for the administration of intravenous fluids is integral to the prehospital management of injured military patients. However, this may be technically challenging to undertake during night-time conditions where the use of light to aid cannulation may give the tactical situation away to opponents. The aim of this study was to investigate the success and tactical safety of venepuncture under battlefield conditions with different colour light sources.
METHOD:
The procedure was carried out with naked eye in a bright room in the absence of a separate light source, with a naked eye in a dark room under red, white, blue and green light sources and under an infrared light source while wearing night vision goggles (NVGs). The success, safety, degree of difficulty and completion time for each procedure were then explored.
RESULTS:
All interventions made in daylight and in a dark room were found to be 100% successful. Interventions performed under infrared light while wearing NVGs took longer than under other light sources or in daylight. Interventions performed under blue light were tactically safer when compared with interventions performed under different light sources.
CONCLUSION:
Blue light offered the best tactical safety during intravenous cannulation under night-time conditions and is recommended for future use in tactical casualty care. The use of NVGs using infrared light cannot be recommended if there is the possibility of opponents having access to the technology.
12/04/2018
Intra-Osseux: En 1er ? Chez les plus graves
The intraosseous have it : A prospective observational study of vascular access success rates in patients in extremis using video review.
Chreiman KM et Al. J Trauma Acute Care Surg. 2018 Apr;84(4):558-563.
-------------
Attention dans cette étude les abords vasculaires ne sont pas réalisés par les mêmes personnels. Ainsi les VVP sont posées en grande majorité par des infirmiers dont la pratique pour ce geste est grande. Ceci pour dire que l'intérêt de l'intra-osseux est majeur, tout particulièrement quand on emploie un dispositif motorisé tel que l'EZ-IO dont l'apprentissage est simplissime pour qui sait employer une perceuse.
-------------
BACKGROUND:
Quick and successful vascular access in injured patients arriving in extremis is crucial to enable early resuscitation and rapid OR transport for definitive repair. We hypothesized that intraosseous (IO) access would be faster and have higher success rates than peripheral intravenous (PIV) or central venous catheters (CVCs).
METHODS:
High-definition video recordings of resuscitations for all patients undergoing emergency department thoracotomy from April 2016 to July 2017 were reviewed as part of a quality improvement initiative. Demographics, mechanism of injury, access type, access location, start and stop time, and success of each vascular access attempt were recorded. Times to completion for access types (PIV, IO, CVC) were compared using Kruskal-Wallis test adjusted for multiple comparisons, while categorical outcomes, such as success rates by access type, were compared using χ test or Fisher's exact test.
RESULTS:
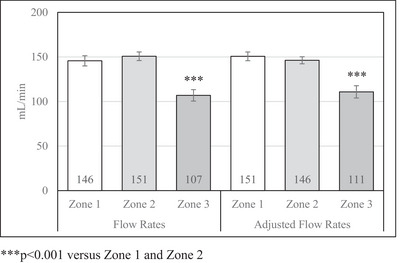
Study patients had a median age of 30 years (interquartile range [IQR], 25-38 years), 92% were male, 92% were African American, and 93% sustained penetrating trauma. A total of 145 access attempts in 38 patients occurred (median, 3.8; SD, 1.4 attempts per patient). There was no difference between duration of PIV and IO attempts (0.63; IQR, 0.35-0.96 vs. 0.39 IQR, 0.13-0.65 minutes, adjusted p = 0.03), but both PIV and IO were faster than CVC attempts (3.2; IQR, 1.72-5.23 minutes; adjusted p < 0.001 for both comparisons). Intraosseous lines had higher success rates than PIVs or CVCs (95% vs. 42% vs. 46%, p < 0.001).
CONCLUSION:
Access attempts using IO are as fast as PIV attempts but are more than twice as likely to be successful. Attempts at CVC access in patients in extremis have high rates of failure and take a median of over 3 minutes. While IO access may not completely supplant PIVs and CVCs, IO access should be considered as a first-line therapy for trauma patients in extremis.
| Tags : intraosseux
30/06/2017
Intra-osseux: Pas un gadget
En route intraosseous access performed in the combat setting
OBJECTIVE:
To describe and compare vascular access practices used by en route care providers during medical evacuation (MEDEVAC).
DESIGN:
This was a retrospective cohort study. Medical records of US military personnel injured in combat and transported by MEDEVAC teams were queried.
PATIENTS:
The subjects were transported by military en route care providers, in the combat theater during Operation Enduring Freedom (OEF) between January 2011 and March 2014. The authors reviewed 1,267 MEDEVAC records of US casualties and included 832 subjects that had vascular access attempts.
MAIN OUTCOME MEASURES:
The outcome measures for this study were vascular access success rates, including intravenous (IV) and intraosseous (IO) attempts. Subjects were grouped by type of vascular access: None, peripheral intravenous (PIV), IO, and PIV + IO (combination of PIV and IO) and by vascular access (PIV or IO) success (No versus Yes). Survival rate, in-flight events, ventilator, intensive care and in hospital days, and 30-day outcomes were compared among groups.
STATISTICAL ANALYSIS:
The authors used chisquare or Fisher's exact tests to evaluate categorical variables. Analysis of variance (ANOVA) or Kruskal-Wallis tests were used for continuous variables.
RESULTS:
Vascular access was attempted in 832 (66 percent) of the 1,267 subjects transported by MEDEVAC during this study period. The majority (n = 758) of the access attempts were PIV of which 93 percent (706/758) were successful. In 74 subjects, IO was the only access attempted with an 85 percent (n = 63) success rate. The overall success rate with IO placement was 88 percent.
CONCLUSIONS:
Intraosseous access has been used successfully in the combat setting and accounts for approximately 12 percent of vascular access in the MEDEVAC population the authors studied.
| Tags : intraosseux
01/05/2017
Intraosseux ? Ne pas aller trop profond
Intramedullary placement of intraosseous cannulas inserted in the preclinical treatment of polytrauma patients : A retrospective, computed tomography-assisted evaluation
Jansen Get Al. Anaesthesist. 2017 Mar;66(3):168-176
-------------------------------
Le recours à la voie intra-osseuse trouve a sa place lors de la prise en charge de traumatisé sévère. Il faut néanmoins s'assurer du bon positionnement intra-médullaire de l'aiguille. Ce travail appelle à de la prudence car il met en évidence la fréquence de positionnements non optimaux notamment un peu trop profond. Une vérification régulière s'impose dans le contexte de la traumatologie sévère.
-------------------------------
BACKGROUND:
Use of intraosseous access to the vascular system is rare in the pre-hospital setting (<1%). However, as patients for which the use of an intraosseous device is indicated are usually in a critical condition, awareness of possible application errors is vital. A survey was performed to evaluate intramedullary needle placement by means of computed axial tomography.
METHODS:
In the period of 01/01/2011 to 31/12/2015 all multislice-CT trauma scans performed in a trauma center were monitored for intraosseous devices in situ. The placement site, type of intraosseous device and needle deployed, thickness of bone and soft tissues, site for optimum needle placement, and both deviation from gold standard placement and visible complications were also recorded.
RESULTS:
In 11 out of 982 patients with suspected polytrauma that were studied during the observation period, 13 intraosseous cannulas were found (1.12%). In all cases, the EZ-IO® (Teleflex, P.O. Box 12600, Research Triangle Park, NC 27709, USA) intraosseous vascular access system was used. All applications were placed correctly in the medullary cavity, but none concurred with the current guidelines: The site of the puncture deviated laterally in seven cases, medially in two cases, cranially in four cases, and caudally in two cases.
The most common error in all 13 cases was overshooting during needle introduction.
CONCLUSION:
Even though clinical criteria may suggest correct placement of an intraosseous device, the results of this survey provide evidence that deviations in positioning are common. Placement of the needle too deep can cause complications within the soft tissues or potentially impede intraosseous infusion.
| Tags : intraosseux
09/03/2017
Intraosseux: Oui, INTRA
Deltoid Compartment Syndrome: A Rare Complication after Humeral Intraosseous Access
| Tags : intraosseux
02/01/2017
Plyo: En intraosseux aussi
Pre-hospital intra-osseous freeze dried plasma transfusion: a case report
Rottenstreich et al. Disaster and Military Medicine 2015, 1:8
Background: Hemorrhage and coagulopathy are among the leading causes of death in combat and are considered the leading causes of preventable deaths. Plasma, in the form of Fresh Frozen Plasma (FFP) is considered a key component in the Damage Control Resuscitation performed within hospitals. Freeze-Dried Plasma (FDP) can be stored at room temperature and therefore is potentially useful in pre-hospital conditions. Our case report join to few cases where FDP was administered at the point of injury. It is also unique as it describes an intra- osseous administration given to pediatric patient.
Case report: M.S. otherwise healthy 13 year old girl was injured due to gunshots and grenade blast. On the first triage by the IDF medical teams she suffered from: Severe hemorrhagic shock, (Blood pressure could not be measured, Heart rate 163), superficial wounds to her face, (forehead and Rt. Eye), gunshot wounds with active bleeding from her Lt. Arm and her RT. Knee (Mangled Extremity Severity Score (MESS) 8) and open fractures of left elbow and right thigh. A peripheral intravenous catheter was established and 1 g tranexamic acid in 500 ml of Hartman fluid were administered. Due to difficulties in establishing a functioning intra-venous line, an intra-osseous catheter was established and one unit of FDP (250 ml) was given in the field. She was transferred by a military medical team to a regional civilian hospital for further treatment. Upon arrival to the hospital her blood pressure and heart rate were significantly improved. After three weeks of hospitalization M.S. was discharged and she was returned to her homeland.
Conclusion: We have described the successful use of FDP for pre hospital resuscitation of a 13 year old girl suffering from severe hemorrhagic shock as a result of gunshots and grenade blast. This case report demonstrates that intra-osseous FDP administration for as part pre hospital resuscitation of children has a favorable outcome.
| Tags : intraosseux
15/09/2016
Position intraosseuse ? Echographiez !
A Serious Adult Intraosseous Catheter Complication and Review of the Literature.
OBJECTIVE:
Current guidelines recommend the use of intraosseous access when IV access is not readily attainable. The pediatric literaturere ports an excellent safety profile, whereas only small prospective studies exist in the adult literature. We report a case of vasopressor extravasation and threatened limb perfusion related to intraosseous access use and our management of the complication. We further report our subsequent systematic review of intraosseous access in the adult population.
DATA SOURCES:
Ovid Medline was searched from 1946 to January 2015.
STUDY SELECTION:
Articles pertaining to intraosseous access in the adult population (age greater than or equal to 14 years) were selected. Search terms were "infusion, intraosseous" (all subfields included), and intraosseous access" as key words.
DATA EXTRACTION:
One author conducted the initial literature review. All authors assessed the methodological quality of the studies and consensus was used to ensure studies met inclusion criteria.
DATA SYNTHESIS:
The case of vasopressor extravasation was successfully treated with pharmacologic interventions, which reversed the effects of the extravasated vasopressors: intraosseous phentolamine, topical nitroglycerin ointment, and intraarterial verapamil and nitroglycerin. Our systematic review of the adult literature found 2,332 instances of intraosseous insertion. A total of 2,106 intraosseous insertion attempts were made into either the tibia or the humerus; 192 were unsuccessful, with an overall success rate of 91%. Five insertions were associated withserious complications. A total of 226 insertion attempts were made into the sternum; 54 were unsuccessful, with an overall success rate of 76%.
----
Color Doppler ultrasonography has been described as a method to verify placement of an intraosseous catheter. A high-frequency linear array transducer is placed near the intraosseous insertion site in either transverse or longitudinal axis. The color Doppler sample box is adjusted to include the subcutaneous compartment, the periosteum, and the intraosseous space, with the tomographic plane oriented to intersect the axis of the intraosseous needle . A 10-mL syringe filled with normal saline is attached to the intraosseous catheter and is rapidly infused with real-time ultrasonography imaging. If the intraosseous catheter is properly placed, color Doppler signal is seen in the subperiosteal (intraosseous) compartment. The presence of color Doppler signal in the extraosseous compartment indicates improper intraosseous catheter placement with extravasation.
----
CONCLUSIONS:
Intraosseous catheter insertion provides a means for rapid delivery of medications to the vascular compartment with a favorable safety profile. Our systematic literature review of adult intraosseous access demonstrates an excellent safety profile with serious complications occurring in 0.3% of attempts. We report an event of vasopressor extravasation that was potentially limb threatening. Therapy included local treatment and injection of intraarterial vasodilators. Intraosseous access complications should continue to be reported, so that the medical community will be better equipped to treat them as they arise.
| Tags : intraosseux
05/08/2016
Echo pour abord vasculaire: Intérêt modéré ?
Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization
Cochrane Database Syst Rev. 2015 Jan 9;1:CD011447. doi: 10.1002/14651858.CD011447.
-------------------------------------
La mise en place d'un abord veineux central est une éventualité peu fréquente en médecine tactique. La maîtrise de l'abord vasculaire périphérique et l'apport de la perfusion intraosseuse suffisent le plus souvent à répondre aux besoins. Néanmoins ce besoin ne peut être écarté. Alors que la majorité des sociétés savantes recommandent le recours à la pose échoguidée, il semblerait qu'une analyse critique de l'intérêt d'une telle pratique ne soit pas encore complètement en faveur de telles recommandations (???). Même si de très grandes avancées technologiques ont lieu et permettent de disposer d'appareil et de sondes adhoc utilisables hors de l'hôpital, dans nos conditions d'exercice et donc in fine de notre aptitude à cette pratique sans échographe.
-------------------------------------
BACKGROUND:
Central venous catheters can help with diagnosis and treatment of the critically ill. The catheter may be placed in a large vein in the neck (internal jugular vein), upper chest (subclavian vein) or groin (femoral vein). Whilst this is beneficial overall, inserting the catheter risks arterial puncture and other complications and should be performed in as few attempts as possible.In the past, anatomical 'landmarks' on the body surface were used to find the correct place to insert these catheters, but ultrasound imaging is now available. A Doppler mode is sometimes used to supplement plain 'two-dimensional' ultrasound.
OBJECTIVES:
The primary objective of this review was to evaluate the effectiveness and safety of two-dimensional ultrasound (US)- or Dopplerultrasound (USD)-guided puncture techniques for subclavian vein, axillary vein and femoral vein puncture during central venous catheter insertion in adults and children. We assessed whether there was a difference in complication rates between traditional landmark-guided and any ultrasound-guided central vein puncture.When possible, we also assessed the following secondary objectives: whether a possible difference could be verified with use of the US technique versus the USD technique; whether there was a difference between using ultrasound throughout the puncture ('direct') and using it only to identify and mark the vein before starting the puncture procedure ('indirect'); and whether these possible differences might be evident in different groups of patients or with different levels of experience among those inserting the catheters.
SEARCH METHODS:
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 1), MEDLINE (1966 to 15 January 2013), EMBASE (1966 to 15 January 2013), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1982 to 15 January 2013), reference lists of articles, 'grey literature' and dissertations. An additional handsearch focused on intensive care and anaesthesia journals and abstracts and proceedings of scientific meetings. We attempted to identify unpublished or ongoing studies by contacting companies and experts in the field, and we searched trial registers. We reran the search in August 2014. We will deal with any studies of interest when we update the review.
SELECTION CRITERIA:
Randomized and quasi-randomized controlled trials comparing two-dimensional ultrasound or Doppler ultrasound versusan anatomical 'landmark' technique during insertion of subclavian or femoral venous catheters in both adults and children.
DATA COLLECTION AND ANALYSIS:
Three review authors independently extracted data on methodological quality, participants, interventions and outcomes of interest using a standardized form. We performed a priori subgroup analyses.
MAIN RESULTS:
Altogether 13 studies enrolling 2341 participants (and involving 2360 procedures) fulfilled the inclusion criteria. The quality of evidence was very low (subclavian vein N = 3) or low (subclavian vein N = 4, femoral vein N = 2) for most outcomes, moderate for one outcome (femoral vein) and high at best for two outcomes (subclavian vein N = 1, femoral vein N = 1). Most of the trials had unclear risk of bias across the six domains, and heterogeneity among the studies was significant. For the subclavian vein (nine studies, 2030 participants, 2049 procedures), two-dimensional ultrasound reduced the risk of inadvertent arterial puncture (three trials, 498 participants, risk ratio (RR) 0.21, 95% confidence interval (CI) 0.06 to 0.82; P value 0.02, I² = 0%) and haematoma formation (three trials, 498 participants, RR 0.26, 95% CI 0.09 to 0.76; P value 0.01, I² = 0%). No evidence was found of a difference in total or other complications (together, US, USD), overall (together, US, USD), number of attempts until success (US) or first-time (US) success rates or time taken to insert the catheter (US). For the femoral vein, fewer data were available for analysis (four studies, 311 participants, 311 procedures). No evidence was found of a difference in inadvertent arterial puncture or other complications. However, success on the first attempt was more likely with ultrasound (three trials, 224 participants, RR 1.73, 95% CI 1.34 to 2.22; P value < 0.0001, I² = 31%), and a small increase in the overall success rate was noted (RR 1.11, 95% CI 1.00 to 1.23; P value 0.06, I² = 50%). No data on mortality or participant-reported outcomes were provided.
AUTHORS' CONCLUSIONS:
On the basis of available data, we conclude that two-dimensional ultrasound offers small gains in safety and quality when compared with an anatomical landmark technique for subclavian (arterial puncture, haematoma formation) or femoral vein (success on the first attempt) cannulation for central vein catheterization. Data on insertion by inexperienced or experienced users, or on patients at high risk for complications, are lacking. The results for Doppler ultrasound techniques versus anatomical landmark techniques are uncertain.
07/08/2015
Intraosseux: Une place réelle à la guerre
Saving the critically injured trauma patient: a retrospective analysis of 1000 uses of intraosseous access
Lewis P et Al. Emerg Med J. 2015 Jun;32(6):463-7
OBJECTIVE:
Intraosseous access (IO) is becoming increasingly accepted in adult populations as an alternative to peripheral vascular access; however, there is still insufficient evidence in large patient groups supporting its use.
METHODS:
Retrospective review. This paper reports on the use of IO devices over a 7-year period from August 2006 to August 2013 during combat operations in Afghanistan. A database search of the Joint Theatre Trauma Registry (JTTR) was carried out looking for all the incidences of IO access use during this time. Excel (Microsoft) was used to manage the dataset and perform descriptive statistics on the patient demographics, injuries, treatments and complications that were retrieved.
RESULTS:
1014 IO devices were used in 830 adult patients with no major complications. The rate of minor complications, the majority of which were device failure, was 1.38%. 5124 separate infusions of blood products or fluids occurred via IO access, with 36% being of packed red cells. On average, each casualty received 6.95 different infusions of blood products and fluids, and 3.28 separate infusions of drugs through IO access. 32 different drugs were infused to 367 patients via IO, the most frequent being anaesthetic agents. IO access was used in the prehospital environment, during tactical helicopter evacuation and within hospitals.
CONCLUSIONS:
IO access can be used to administer a wide variety of life-saving medications quickly, easily and with low-complication rates. This highlights its valuable role as an alternative method of obtaining vascular access, vital when resuscitating the critically injured trauma patient.
| Tags : intraosseux
Intraosseux tibial: Pas l'idéal !
Intraosseous infusion rates under high pressure: a cadaveric comparison of anatomic sites
Pasley J et al. J Trauma Acute Care Surg 2015;78(2):295-9.
-------------------------------------------------
Dans notre pratique le choix d'un abord tibial est le plus fréquent mais certainement pas le plus pertinent chez l'adulte. Le taux de succès de 1ère pose, le débit atteint les les aléas de perfusion font qu'un abord huméral ou sternal sont un meilleur choix. C'est ce laisse supposer ce document.
-------------------------------------------------
BACKGROUND:
When traditional vascular access methods fail, emergency access through the intraosseous (IO) route can be lifesaving. Fluids, medications, and blood components have all been delivered through these devices. We sought to compare the performance of IO devices placed in the sternum, humeral head, and proximal tibia using a fresh human cadaver model.
METHODS:
Commercially available IO infusion devices were placed into fresh human cadavers: sternum (FAST-1), humeral head (EZ-IO), and proximal tibia (EZ-IO). Sequentially, the volume of 0.9% saline infused into each site under 300 mm Hg pressure over 5 minutes was measured. Rates of successful initial IO device placement and subjective observations related to the devices were also recorded.
RESULTS:
For 16 cadavers over a 5-minute bolus infusion, the total volume of fluid infused at the three IO access sites was 469 (190) mL for the sternum, 286 (218) mL for the humerus, and 154 (94) mL for the tibia. Thus, the mean (SD) flow rate infused at each site was as follows: (1) sternum, 93.7 (37.9) mL/min; (2) humerus, 57.1 (43.5) mL/min; and (3) tibia, 30.7 (18.7) mL/min. The tibial site had the greatest number of insertion difficulties.
CONCLUSION:
This is the first study comparing the rate of flow at the three most clinically used adult IO infusion sites in an adult human cadaver model. Our results showed that the sternal site for IO access provided the most consistent and highest flow rate compared with the humeral and tibial insertion sites. The average flow rate in the sternum was 1.6 times greater than in the humerus and 3.1 times greater than in the tibia.
| Tags : intraosseux
Intraosseux = Embolie graisseuse
Fat Intravasation from Intraosseous Flush and Infusion Procedures
Rubal BJ et Al. Prehosp Emerg Care. 2015 Jul-Sep;19(3):376-90
----------------------------------
On s'en doutait mais cela est objectivé: Le recours à la perfusion intraosseuse est responsable d'embolie graisseuse. La survenue d'une telle complication est moindre quand la procédure de flush ne dépasse pas 300mmHg et que le débit est lent. Dont acte au moins pour le flush.
----------------------------------
STUDY HYPOTHESIS:
The primary study objective was to delineate the procedural aspects of intraosseous (IO) infusions responsible for fatintravasation by testing the hypothesis that the fat content of effluent blood increases during IO infusions.
METHODS:
IO cannulas were inserted into the proximal tibiae of 35 anesthetized swine (Sus scrofa, 50.1 ± 3.5 kg) and intravasated fat was assessed using a lipophilic fluoroprobe (Nile red) and by vascular ultrasound imaging. Effluent blood bone marrow fat was assessed at baseline, during flush, and with regimens of controlled infusion pressures (73-300 mmHg) and infusion flow rates (0.3-3.0 mL per second). Fat intravasation was also assessed with IO infusions at different tibial cannulation sites and in the distal femur. In 7 animals, the lipid uptake of alveolar macrophages and lung tissue assessed for fat embolic burden using oil red O stain 24 hours post infusion. Additionally, bone marrow shear-strain was assessed radiographically with IO infusions.
RESULTS:
Fat intravasation was observed during all IO infusion regimens, with subclinical pulmonary fat emboli persisting 24 hours post infusion. It was noted that initial flush was a significant factor in fat intravasation, low levels of intravasation occurred with infusions ≤300 mmHg, fat intravasationand bone marrow shear-strain increased with IO infusion rates, and intravasation was influenced by cannula insertion site. Ultrasound findings suggest that echogenic particles consistent with fat emboli are carried in fast and slow venous blood flow fields. Echo reflective densities were observed to rise to the nondependent endovascular margins and coalesce in accordance with Stoke's law. In addition, ultrasound findings suggested that intravasated bone marrow fat was thrombogenic.
CONCLUSION:
Results suggest that in swine the intravasation of bone marrow fat is a common consequence of IO infusion procedures and that its magnitude is influenced by the site of cannulation and infusion forces. Although the efficacy and benefits of IO infusions for emergent care are well established, emergency care providers also should be cognizant that infusion procedures affect bone marrow fat intravasation.
| Tags : intraosseux
03/08/2015
Accès veineux: Vision israélienne
Intravenous access in the prehospital settings: What can be learned from point-of-injury experience
Nadler R et Al. J Trauma Acute Care Surg. 2015;79: 221-226
-----------------------------------
La réalisation d'un abord vasculaire est un des gestes le plus souvent pratiqué. On rappelle qu'il s'agit là de pouvoir injecter certains médicaments (morphine, adrénaline, TXA, antibiotiques), d'initier un remplissage vasculaire raisonné voire d'administrer des dérives sanguins ou fractions coagulantes. Un document intéressant qui émane de l'armée israélienne fait le point sur cette pratique. Dans cette dernière (qui on le rappelle est assez spécifique compte tenu de la grande proximité des zones de combat et des structures hospitalières), il apparaît qu'il ne faille pas aller au delà de deux tentatives de pose de VVP au risque de retarder la prise en charge chirurgicale des blessés. Par ailleurs les taux de succès des médecins, combat medics et paramédics (pour nous nos infirmiers) soit superposable. Enfin la médiocre performance de l'accès intra-osseux doit interpeller.
-----------------------------------
BACKGROUND:
Intravenous (IV) access has an essential role in the care provided for trauma patients, allowing for transfusion of blood products, fluids, and drugs. Decisions should be made regarding the necessity of IV access while considering cost-benefit of the procedure in terms of delayed evacuation times.
METHODS:
A retrospective review of all trauma patients in whom at least one attempt at IVaccess was performed were reviewed. Data were abstracted from the Israeli Defense Force Trauma Registry.
RESULTS:
Of 7,476 patients, 1,082 patients who had at least one documented attempt at IV access between January 1997 and April 2013 were included in this study. Overall cumulative success rate at IV access was 82%. Success rates for IVaccess were 86%, 68%, 63%, 50%, 20% for the first, second, third, fourth, and fifth attempts, respectively. The first and second attempts accounted for 96% of the successful procedures. Mortality in patients for whom IV access was successful was 13%; mortality in patients for whom IV access was not successful was 35%.
CONCLUSION:
The success rate of IV access declined with each subsequent attempt. There was minimal improvement of overall success rate seen after the second attempt. Our findings suggest that the inability to obtain peripheral venous access is associated with severe injuries. These finding support a policy of limiting the number of venous access attempts to two attempts, followed by a reevaluation of need for parenteral access. Improved training of combat medics and paramedics might marginally increase the success rates of IVaccess. Point-of-injury data, used for ongoing learning and research, form the ground for improving combat casualty care and thus help saving lives.
| Tags : perfusion
26/11/2014
Intraosseux: Pourquoi pas la mandibule ?
Intraosseous Vascular Access through the Anterior Mandible – A Cadaver Model Pilot Study
Goldschalt C. et Al. PLoS One. 2014; 9(11): e112686.
-----------------------------------------------------
L'anesthésie intraosseuse est bien connue des chirurgiens dentistes. Pour autant s'agit il d'une voie potentielle d'abord vasculaire ? Peut être, sous réserve de respecter la zone de ponction et éviter le nerf dentaire inférieur.
-----------------------------------------------------
Background
Several insertion sites have been described for intraosseous puncture in cases of emergencies when a conventional vascular access cannot be established. This pilot study has been designed to evaluate the feasibility of the mandibular bone for the use of an intraosseous vascular access in a cadaver model.
Methodology/Principal Findings
17 dentistry and 16 medical students participating in a voluntary course received a short introduction into the method and subsequently used the battery powered EZ-IO system with a 15 mm cannula for a puncture of the anterior mandible in 33 cadavers. The time needed to perform each procedure was evaluated. India ink was injected into the accesses and during the anatomy course cadavers were dissected to retrace the success or failure of the puncture. Dental students needed 25.5±18.9(mean±standard deviation)s and medical students 33±20.4 s for the procedure (p=0.18). Floor of mouth extravasation occurred in both groups in 3 cases. Success rates were 82 and 75% (p=0.93).

Conclusions/Significance
Despite floor of mouth extravasation of injected fluid into a mandibular intraosseous access might severely complicate this procedure, the anterior mandible may be helpful as an alternative to other intraosseous and intravenous insertion sites when these are not available in medical emergencies.
| Tags : intraosseux
BIG: Pas si évident !
The israeli defense force experience with intraosseous access
Nadler R.et All. Mil Med. 2014 Nov;179(11):1254-7
----------------------------------------------------------------------
La réalisation d'un abord vasculaire peut faire appel à la voie intraosseuse. Trois dispositifs sont prévus par la procédure du sauvetage au combat: le trocard de mallarmé, le BIG et l'EZ_IO. Si les études expérimentales sont en faveur de cette pratique, la réalité ne semble pas suivre notamment pour le BIG. Relativement peu de dispositifs ont eu un emploi enregistré avec un taux de succès faible. Peut être un problème de stratégie d'emploi ?
----------------------------------------------------------------------
INTRODUCTION:
Obtaining vascular access is of paramount importance in trauma care. When peripheral venous access is indicated but cannot be obtained, the intraosseous route represents an alternative. The Bone Injection Gun (BIG) is the device used for intraosseous access by the Israeli Defense Force (IDF). The purpose of this study is to assess the success rate of intraosseous access using this device.
METHOD:
The IDF Trauma Registry from 1999 to 2012 was searched for patients for whom at least 1 attempt at intraosseous access was made.
RESULTS:
37 attempts at intraosseous access were identified in 30 patients. Overall success rate was 50%. No differences in success rates were identified between different care givers. Overall mortality was 87%.
CONCLUSION:
The use of BIG in the IDF was associated with a low success rate at obtaining intraosseous access. Although inability to achieve peripheral venous access can be considered an indicator for poor prognosis, the high mortality rate for patients treated with BIG can also stand for the provider's low confidence in using this tool, making its usemaking its use a last resort. This study serves as an example to ongoing learning process that includes data collection, analysis, and improvement, constantly taking place in the IDF
| Tags : intraosseux
27/10/2014
Perfuser + vite: Pas n'importe comment !
Novel rapid infusion device for patients in emergency situations
Kapoor DJ et Al. Scand J Trauma Resusc Emerg Med. 2011 Jun 10;19:35
Il peut être nécessaire d'accélérer le débit d'une perfusion. Pour cela il peut être fait appel à une manchette à pression, une tubulure de type 'blood pump", un système "robinet 3 voies ", plus rarement un système à compression par lame voire une pompe électrique.
Le document présenté fait appel à l'injection d'air dans le corps du soluté utilisé. La sécurité de cette manière de faire interpelle quelque peu. En effet les auteurs estiment que le filtre 15µ présent dans la tubulure a un effet barrière anti air suffisant pour éviter tout risque d'embolie gazeuse.
 Ce type de pratique est associé à une prise de risque du fait du concept même de la méthode, des conditions d'hygiène non respectées et des conditions de surveillance non optimales en conditions extrême.
Ce type de pratique est associé à une prise de risque du fait du concept même de la méthode, des conditions d'hygiène non respectées et des conditions de surveillance non optimales en conditions extrême.
04/02/2014
L'intraosseux: La vraie vie
Complication with Intraosseous Access: Scandinavian Users’ Experience
Hallas P. et All. West J Emerg Med. 2013;14(5):440–443
Pas si idyllique que cela
| Tags : intraosseux
26/10/2013
L'intraosseuse: Pas adaptée au dammage control resuscitation?
What is the evidence of utility for intraosseous blood transfusion in damage-control resuscitation ?
Harris M et all. J Trauma Acute Care Surg. 2013 Nov;75(5):904-6
« The scientific and clinical evidence for the use of IO access is voluminous, as evidenced by the Scientific Bibliography provided by VidaCare,6 one of the large manufacturers of IO devices, and available in any routine literature search. However direct scientific and/or clinical data to support the use of IO access for the purpose of blood transfusion in adult humans are very limited to anecdotal reports.
the absence of good evidence supporting the use of IO access for the very critical function of blood transfusion in DCR places existing recommendations for its use in question. This lack of evidence is compounded by the clinical experience of the lead author. Multiple attempts to use IO access for blood transfusion, both in the civilian adult emergency setting and in combat casualty care, have repeatedly been unsuccessful »
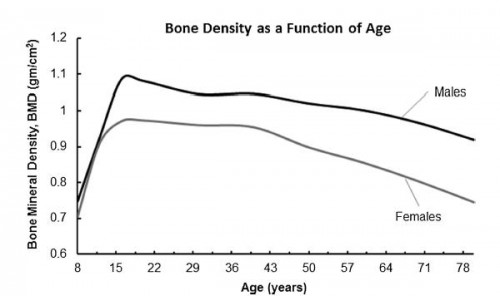
1. La densité osseuse dépend de l'âge
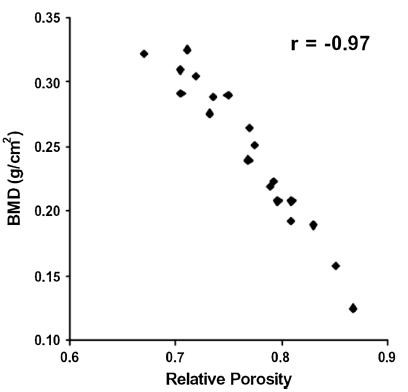
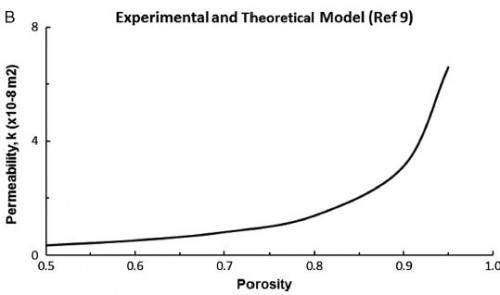
2. La porosité osseuse dépend de la densité osseuse
 77
77
3. La perméabilité osseuse dépend de la porosité
« The bone mineral density increases with age up to a peak density occurring in the early 20s. The soldier population is aged right at the peak of bone density for all races and sex.
the viscosity of pRBCs used in DCR is estimated to be greater than 10 cP.12 Since pRBCs are 10+ times more viscous than crystalloid solutions, it will require at least 10+ times the pressure to obtain the same flow rate as crystalloid in IO infusion.
Based on the Darcy’s Law, the only parameter a medical practitioner has to adjust to increase flow rate in an IO system in DCR is pressure. Increases in pressure not only strain the connections in the infusion system itself but also increase shearing forces in the fluid. Shearing forces may cause hemolysis of the transfused blood, loss of oxygen carrying capacity, and consequent development of rhabdomyolysis
we postulate that maximum flow rates attainable for transfusion of blood products used in DCR via the IO route are simply inadequate for successful resuscitation »
| Tags : intraosseux

 Initially she was treated conservatively but then was taken emergently for a fasciotomy. After confirming the diagnosis with compartment pressures, a 2-incision approach was employed and a large hematoma was evacuated from the inferior margin of the anterior deltoid. The rest of the deltoid was inspected and debrided to healthy bleeding tissue. Her fasciotomy wounds were left open to heal on their own due to her tenuous clinical condition. At most recent follow-up, she had full range of motion in her shoulder and no residual pain. Our unique case study is the first documented incidence of upper extremity compartment syndrome after
Initially she was treated conservatively but then was taken emergently for a fasciotomy. After confirming the diagnosis with compartment pressures, a 2-incision approach was employed and a large hematoma was evacuated from the inferior margin of the anterior deltoid. The rest of the deltoid was inspected and debrided to healthy bleeding tissue. Her fasciotomy wounds were left open to heal on their own due to her tenuous clinical condition. At most recent follow-up, she had full range of motion in her shoulder and no residual pain. Our unique case study is the first documented incidence of upper extremity compartment syndrome after