24/10/2019
Trauma airways: Une revue
Airway trauma: a review on epidemiology, mechanisms of injury, diagnosis and treatment.
Prokakis C et Al. J Cardiothorac Surg. 2014 Jun 30;9:117.
Airway injuries are life threatening conditions. A very little number of patients suffering air injuries are transferred live at the hospital. The diagnosis requires a high index of suspicion based on the presence of non-specific for these injuries symptoms and signs and a thorough knowledge of the mechanisms of injury. Bronchoscopy and chest computed tomography with MPR and 3D reconstruction of the airway represent the procedures of choice for the definitive diagnosis. Endotracheal intubation under bronchoscopic guidance is the key point to gain airway control and appropriate ventilation. Primary repair with direct suture or resection and an end to end anastomosis is the treatment of choice for patients suffering from tracheobronchial injuries (TBI). The surgical approach to the injured airway depends on its location. Selected patients, mainly with iatrogenic injuries, can be treated conservatively as long as the injury is small (<2 cm), a secure and patent airway and adequate ventilation are achieved, and there are no signs of sepsis. Patients with delayed presentation airway injuries should be referred for surgical treatment. Intraoperative evaluation of the viability of the lung parenchyma beyond the site of stenosis/obstruction is mandatory to avoid unnecessary lung resection.
| Tags : airway
14/10/2019
Pansements compressifs: Le test de la NAMRU
Pas nouveau mais instructif dans le contexte de bataille commerciale entre les industriels
08/10/2019
Bloc ilio-fascial: Docteur ou IDE, Faites en !
Efficacy of Prehospital Analgesia with Fascia Iliaca Compartment Block for Femoral Bone Fractures: A Systematic Review.
INTRODUCTION:
Femoral fractures are painful injuries frequently encountered by prehospital practitioners. Systemic opioids are commonly used to manage the pain after a femoral fracture; however, regional techniques for providing analgesia may provide superior targeted pain relief and reduce opioid requirements. Fascia Iliaca Compartment Block (FICB) has been described as inexpensive and does not require special skills or equipment to perform, giving it the potential to be a suitable prehospital intervention. ProblemThe purpose of this systematic review is to summarize published evidence on the prehospital use of FICB in patients of any age suffering femoral fractures; in particular, to investigate the effects of a prehospital FICB on pain scores and patient satisfaction, and to assess the feasibility and safety of a prehospital FICB, including the success rates, any delays to scene time, and any documented adverse effects.
METHODS:
A literature search of MEDLINE/PubMED, Embase, OVID, Scopus, the Cochrane Database, and Web of Science was conducted from January 1, 1989 through February 1, 2017. In addition, reference lists of review articles were reviewed and the contents pages of the British Journal of Anaesthesia (The Royal College of Anaesthetists [London, UK]; The College of Anaesthetists of Ireland [Dublin, Ireland]; and The Hong Kong College of Anaesthesiologists [Aberdeen, Hong Kong]) 2016 along with the journal Prehospital Emergency Care (National Association of Emergency Medical Service Physicians [Overland Park, Kansas USA]; National Association of State Emergency Medical Service Officials [Falls Church, Virginia USA]; National Association of Emergency Medical Service Educators [Pittsburgh, Pennsylvania USA]; and the National Association of Emergency Medical Technicians [Clinton, Mississippi USA]) 2016 were hand searched. Each study was evaluated for its quality and its validity and was assigned a level of evidence according to the Oxford Centre for Evidence-Based Medicine (OCEBM; Oxford, UK).
RESULTS:
Seven studies involving 699 patients were included (one randomized controlled trial [RCT], four prospective observational studies, one retrospective observational study, and one case report). Pain scores reduced after prehospital FICB across all studies, and some achieved a level of significance to support this. Out of a total of 254 prehospital FICBs, there was a success rate of 90% and only one adverse effect reported.
--------
"Across all studies, a total of 256 FICBs were performed in a prehospital environment by a variety of practitioners (145 by physicians, 100 by nurses, and 11 by paramedics)"
--------
Few studies have investigated the effects of prehospital FICB on patient satisfaction or scene time delays.
CONCLUSIONS AND RELEVANCE:
The FICB is suitable for use in the prehospital environment for the management of femoral fractures. It has few adverse effects and can be performed with a high success rate by practitioners of any background. Studies suggest that FICB is a useful analgesic technique, although further research is required to investigate its effectiveness compared to systemic opioids..
Exsufflation: 14G de 5 cm c'est bon
Needle Thoracostomy: Does Changing Needle Length and Location Change Patient Outcome?
BACKGROUND:
Needle thoracostomy (NT) is a common prehospital intervention for patients in extremis or cardiac arrest due to trauma. The purpose of this study is to compare outcomes, efficacy, and complications after a change in policy related to NT in a four-county Emergency Medical Services (EMS) system with a catchment area of greater than 1.6 million people.
METHODS:
This is a before and after observational study of all patients who had NT performed in the Central California (USA) EMS system. The before, anterior midclavicular line (MCL) group consisted of all patients who underwent NT from May 7, 2007 through February 28, 2013. The after, midaxillary line (MAL) axillary group consisted of all patients who underwent NT from March 1, 2013 through January 30, 2016, after policy revisions changed the timing, needle size, and placement location for NT. All prehospital and hospital records where NT was performed were queried for demographics, mechanism of injury, initial status and post-NT clinical change, reported complications, and final outcome. The trauma registry was accessed to obtain Injury Severity Scores (ISS). Information was manually abstracted by study investigators and examined utilizing univariate and multivariate analyses.
RESULTS:
Three-hundred and five trauma patients treated with NT were included in this study, of which, 169 patients (the MCL group) were treated with a 14-guage intravenous (IV) catheter at least 5.0-cm long at the second intercostal space (ICS), MCL after being placed in the ambulance; and 136 patients (the MAL group) were treated with a 10-guage IV catheter at least 9.5-cm long at the fifth ICS, MAL on scene. The mean ISS was lower in the MAL cohort (64.5 versus 69.2; P=.007). The mortality rate was 79% in both groups.
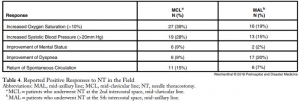
The multivariate model with regard to survival supported that a lower ISS (P<.001) and reported clinical change after NT (P=.003) were significant indicators of survival. No complications from NT were reported.
CONCLUSIONS:
Changing the timing, length of needle, and location of placement did not change mortality in patients requiring NT. Needle thoracostomy was used more frequently after the change in policy, and the MAL cohort was less injured. No increase in reported complications was noted.
| Tags : exsufflation
IT Clamp: Pas convaincant !
External Soft-Tissue Hemostatic Clamp Compared to a Compression Tourniquet as Primary Hemorrhage Control Device in Pilot Flow Model Study.
INTRODUCTION:
Acute blood loss represents a leading cause of death in both civilian and battlefield trauma, despite the prioritization of massive hemorrhage control by well-adopted trauma guidelines. Current Tactical Combat Casualty Care (TCCC) and Tactical Emergency Casualty Care (TECC) guidelines recommend the application of a tourniquet to treat life-threatening extremity hemorrhages. While extremely effective at controlling blood loss, the proper application of a tourniquet is associated with severe pain and could lead to transient loss of limb function impeding the ability to self-extricate or effectively employ weapons systems. As a potential alternative, Innovative Trauma Care (San Antonio, Texas USA) has developed an external soft-tissue hemostatic clamp that could potentially provide effective hemorrhage control without the aforementioned complications and loss of limb function. Thus, this study sought to investigate the effectiveness of blood loss control by an external soft-tissue hemostatic clamp versus a compression tourniquet.
HYPOTHESIS:
The external soft-tissue hemostatic clamp would be non-inferior at controlling intravascular fluid loss after damage to the femoral and popliteal arteries in a normotensive, coagulopathic, cadaveric lower-extremity flow model using an inert blood analogue, as compared to a compression tourniquet.
METHODS:
Using a fresh cadaveric model with simulated vascular flow, this study sought to compare the effectiveness of the external soft-tissue hemostatic clamp versus the compression tourniquet to control fluid loss in simulated trauma resulting in femoral and posterior tibial artery lacerations using a coagulopathic, normotensive, cadaveric-extremity flow model. A sample of 16 fresh, un-embalmed, human cadaver lower extremities was used in this randomized, balanced two-treatment, two-period, two-sequence, crossover design. Statistical significance of the treatment comparisons was assessed with paired t-tests. Results were expressed as the mean and standard deviation (SD).
RESULTS:
Mean intravascular fluid loss was increased from simulated arterial wounds with the external soft-tissue hemostatic clamp as compared to the compression tourniquet at the lower leg (119.8mL versus 15.9mL; P <.001) and in the thigh (103.1mL versus 5.2mL; P <.001).
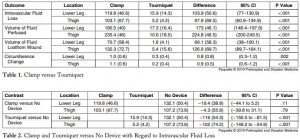
CONCLUSION:
In this hemorrhagic, coagulopathic, cadaveric-extremity experimental flow model, the use of the external soft-tissue hemostatic clamp as a hasty hemostatic adjunct was associated with statistically significant greater fluid loss than with the use of the compression tourniquet.
Formation au Tourniquet: Il faut mieux faire
High Tourniquet Failure Rates Among Non-Medical Personnel Do Not Improve with Tourniquet Training, Including Combat Stress Inoculation: A Randomized Controlled Trial.
BACKGROUND:
The rate of failing to apply a tourniquet remains high.
HYPOTHESIS:
The study objective was to examine whether early advanced training under conditions that approximate combat conditions and provide stress inoculation improve competency, compared to the current educational program of non-medical personnel.
METHODS:
This was a randomized controlled trial. Male recruits of the armored corps were included in the study. During Combat Lifesaver training, recruits apply The Tourniquet 12 times. This educational program was used as the control group. The combat stress inoculation (CSI) group also included 12 tourniquet applications, albeit some of them in combat conditions such as low light and physical exertion. Three parameters defined success, and these parameters were measured by The Simulator: (1) applied pressure ≥ 200mmHg; (2) time to stop bleeding ≤ 60 seconds; and (3) placement up to 7.5cm above the amputation.
RESULTS:
Out of the participants, 138 were assigned to the control group and 167 were assigned to the CSI group. The overall failure rate was 80.33% (81.90% in the control group versus 79.00% in the CSI group; P value = .565; 95% confidence interval, 0.677 to 2.122). Differences in pressure, time to stop bleeding, or placement were not significant (95% confidence intervals, -17.283 to 23.404, -1.792 to 6.105, and 0.932 to 2.387, respectively).
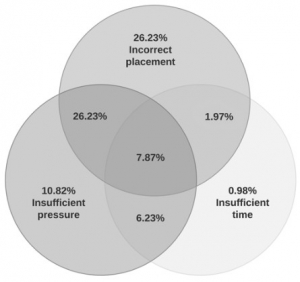
Tourniquet placement was incorrect in most of the applications (62.30%).
CONCLUSIONS:
This study found high rates of failure in tourniquet application immediately after successful completion of tourniquet training. These rates did not improve with tourniquet training, including CSI. The results may indicate that better tourniquet training methods should be pursued.
| Tags : tourniquet
07/10/2019
Membrane cricoïdienne à (0.13xP kg) + 0.86 mm
Depth to the airway lumen at the level of the cricothyroid membrane measured by ultrasound.
BACKGROUND:
Knowing the likely depth to the airway before emergency cricothyroidotomy may improve success in cases where it cannot be measured. Our aim was to measure the depth to the airway at the cricothyroid membrane by ultrasound in a large group of adult patients.
METHOD:
Prospective, observational study in two centres, Oxford and Gloucester. Patients presenting for a large variety of surgical operations were studied. Patients under 18 years old; pregnant; critically ill; had a history of neck surgery not included. Ultrasound examination was performed pre-operatively while participants lay supine with their head and neck extended, with light transducer pressure. We measured depth to the airway lumen in mm; age; weight; height and sex.
RESULTS:
In total 352 patients were studied. We found that depth to the airway lumen strongly correlated with weight (r=0.855, p<0.001) and to a lesser extent body mass index (r=0.781, p<0.001) but did not correlate to sex. Statistical analysis produced an equation to predict upper 95% CI of depth to the airway from the patient's weight: Depth to the airway lumen in mm = (0.13 x weight in kg) + 0.86.
CONCLUSIONS:
If ultrasound measurement is not possible before emergency cricothyroidotomy, the clinician could use our results to predict the depth to the airway by using the patient's weight. If the upper 95% CI were used as the depth of incision, it would enter the airway in 39 out of 40 patients of that weight, without damage to posterior structures in those with a shallower airway.
04/10/2019
Aide cognitive: Intérêt pour le sauvetage au combat
02/10/2019
Les soirées des JET HEH Lyon
01/10/2019
Préparation mentale: Soyez pratiquants +++
Mental Skills in Surgery: Lessons Learned from Virtuosos, Olympians, and Navy Seals.
----------------------------------------
Les techniques de préparation mentale ont fait leurs preuves dans le domaine du sport. Elles commencent à être utilisées dans le domaine médical ET CELA MARCHE. Le document proposé fait le point sur son intérêt.
----------------------------------------
OBJECTIVE:
The present study investigated the role of mental skills in surgery through the unique lens of current surgeons who had previously served as Olympic athletes, elite musicians, or expert military personnel.
BACKGROUND:
Recent work has demonstrated great potential for mental skills training in surgery. However, as a field, we lag far behind other high-performance domains that explicitly train and practice mental skills to promote optimal performance. Surgery stands to benefit from this work. First, there is a need to identify which mental skills might be most useful in surgery and how they might be best employed.
METHODS:
Using a constructivist grounded theory approach, semi-structured interviews were conducted with 17 surgeons across the United States and Canada who had previously performed at an elite level in sport, music, or the military.
RESULTS:
Mental skills were used both to optimize performance in the moment and longitudinally. In the moment, skills were used proactively to enter an ideal performance state, and responsively to address unwanted thoughts or emotions to re-enter an acceptable performance zone. Longitudinally, participants used skills to build expertise and maintain wellness.
CONCLUSIONS:
Establishing a taxonomy for mental skills in surgery may help in the development of robust mental skills training programs to promote optimal surgeon wellness and performance.