30/12/2018
HEXACYL: Oui , mais attention à la MTE
Tranexamic acid administration is associated with an increased risk of posttraumatic venous thromboembolism.
BACKGROUND:
Tranexamic acid (TXA) is used as a hemostatic adjunct for hemorrhage control in the injured patient and reduces early preventable death. However, the risk of venous thromboembolism (VTE) has been incompletely explored. Previous studies investigating the effect of TXA on VTE vary in their findings. We performed a propensity matched analysis to investigate the association between TXA and VTE following trauma, hypothesizing that TXA is an independent risk factor for VTE.
METHODS:
This retrospective study queried trauma patients presenting to a single Level I trauma center from 2012 to 2016. Our primary outcome was composite pulmonary embolism or deep vein thrombosis. Mortality, transfusion, intensive care unit and hospital lengths of stay were secondary outcomes. Propensity matched mixed effects multivariate logistic regression was used to determine adjusted odds ratio (aOR) and 95% confidence intervals (95% CI) of TXA on outcomes of interest, adjusting for prespecified confounders. Competing risks regression assessed subdistribution hazard ratio of VTE after accounting for mortality.
RESULTS:
Of 21,931 patients, 189 pairs were well matched across propensity score variables (standardized differences <0.2). Median Injury Severity Score was 19 (interquartile range, 12-27) and 14 (interquartile range, 8-22) in TXA and non-TXA groups, respectively (p = 0.19). Tranexamic acid was associated with more than threefold increase in the odds of VTE (aOR, 3.3; 95% CI, 1.3-9.1; p = 0.02).
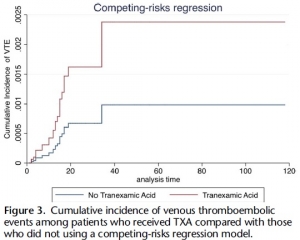
Tranexamic acid was not significantly associated with survival (aOR, 0.86; 95% CI, 0.23-3.25; p = 0.83). Risk of VTE remained elevated in the TXA cohort despite accounting for mortality (subdistribution hazard ratio, 2.42; 95% CI, 1.11-5.29; p = 0.03).
CONCLUSION:
Tranexamic acid may be an independent risk factor for VTE. Future investigation is needed to identify which patients benefit most from TXA, especially given the risks of this intervention to allow a more individualized treatment approach that maximizes benefits and mitigates potential harms.
| Tags : coagulopathie
15/12/2018
Hydroxocobalamine: Pour la coagulopathie et la pression
Intravenous Hydroxocobalamin Versus Hextend Versus Control for Class III Hemorrhage Resuscitation in a Prehospital Swine Model
Bebarta VS et Al. Mil Med. 2018 Nov 5;183(11-12):e721-e729.
Background: Hydroxyethyl starch (Hextend) has been used for hemorrhagic shock resuscitation, however, hydroxyethyl starch may be associated with adverse outcomes.
Objective: To compare systolic blood pressure (sBP) in animals that had 30% of their blood volume removed and treated with intravenous hydroxocobalamin, hydroxyethyl starch, or no fluid.
Methods: Twenty-eight swine (45-55 kg) were anesthetized and instrumented with continuous femoral and pulmonary artery pressure monitoring. Animals were hemorrhaged 20 mL/kg over 20 minutes and then administered 150 mg/kg IV hydroxocobalamin in 180 mL saline, 500 mL hydroxyethyl starch, or no fluid and monitored for 60 minutes. Data were modeled using repeated measures multivariate analysis of variance.
Results: There were no significant differences before treatment. At 20 minutes after hemorrhage, there was no significant difference in mean sBP between treated groups, however, control animals displayed significantly lower mean sBP (p < 0.001). Mean arterial pressure and heart rate improved in the treated groups but not in the control group (p < 0.02). Prothrombin time was longer and platelet counts were lower in the Hextend group (p < 0.05). Moreover, thromboelastography analysis showed longer clotting (K) times (p < 0.05) for the hydroxyethyl starch-treated group.
Conclusion: Hydroxocobalamin restored blood pressure more effectively than no treatment and as effectively as hydroxyethyl starch but did not adversely affect coagulation.
13/12/2018
Rétrospective sur les missions du SSA
A lire pour avoir une image actualisée du SSA. Certes peine à la peine mais, fidèle à ses traditions, n'a manifestement pas chômé ses dernières années
Clic sur l'image pour accéder à la publication
12/12/2018
Tueries massives: Une distribution différente des blessures de guerre
Fatal Wounding Pattern and Causes of Potentially Preventable Death Following the Pulse Night Club Shooting Event.
--------------------------------
BACKGROUND:
Mortality following shooting is related to time to provision of initial and definitive care. An understanding of the wounding pattern, opportunities for rescue, and incidence of possibly preventable death is needed to achieve the goal of zero preventable deaths following trauma.
METHODS:
A retrospective study of autopsy reports for all victims involved in the Pulse Nightclub Shooting was performed. The site of injury, probable site of fatal injury, and presence of potentially survivable injury (defined as survival if prehospital care is provided within 10 minutes and trauma center care within 60 minutes of injury) was determined independently by each author. Wounds were considered fatal if they involved penetration of the heart, injury to any non-extremity major blood vessel, or bihemispheric, mid-brain, or brainstem injury.
RESULTS:
There were an average of 6.9 wounds per patient. Ninety percent had a gunshot to an extremity, 78% to the chest, 47% to the abdomen/pelvis, and 39% to the head. Sixteen patients (32%) had potentially survivable wounds, 9 (56%) of whom had torso injuries. Four patients had extremity injuries, 2 involved femoral vessels and 2 involved the axilla. No patients had documented tourniquets or wound packing prior to arrival to the hospital. One patient had an isolated C6 injury and 2 victims had unihemispheric gunshots to the head.
CONCLUSIONS:
A comprehensive strategy starting with civilian providers to provide care at the point of wounding along with a coordinated public safety approach to rapidly evacuate the wounded may increase survival in future events.
10/12/2018
Bilan US de 10 ans d'urgences en Irak/AFG
An analysis of casualties presenting to military emergency departments in Iraq and Afghanistan.
BACKGROUND:
During the past 17 years of conflict the deployed US military health care system has found new and innovative ways to reduce combat mortality down to the lowest case fatality rate in US history. There is currently a data dearth of emergency department (ED) care delivered in this setting. We seek to describe ED interventions in this setting.
METHODS:
We used a series of ED procedure codes to identify subjects within the Department of Defense Trauma Registry from January 2007 to August 2016.
RESULTS:
During this time, 28,222 met inclusion criteria. The median age of causalities in this dataset was 25 years and most (96.9%) were male, US military (41.3%), and part of Operation Enduring Freedom (66.9%). The majority survived to hospital discharge (95.5%). Most subjects sustained injuries by explosives (55.3%) and gunshot wound (GSW). The majority of subjects had an injury severity score that was considered minor (74.1%), while the preponderance of critically injured casualties sustained injuries by explosive (0.7%). Based on AIS, the most frequently seriously injured body region was the extremities (23.9%). The bulk of administered blood products were packed red blood cells (PRBC, 26.4%). Endotracheal intubation was the most commonly performed critical procedure (11.9%). X-ray (79.9%) was the most frequently performed imaging study.
CONCLUSIONS:
US military personnel comprised the largest proportion of combat casualties and most were injured by explosive. Within this dataset, ED providers most frequently performed endotracheal intubation, administered blood products, and obtained diagnostic imaging studies.
09/12/2018
Délivrance du sang: Merci les TAP
BACKGROUND:
Haemorrhagic shock remains the leading cause of preventable death in overseas and austere settings. Transfusion of blood components is critical in the management of this kind of injury. For French naval and ground military units, this supply often takes too long considering the short shelf-life of red blood cell concentrates (RBCs) and the limited duration of transport in cooling containers (five to six days). Air-drop supply could be an alternative to overcome these difficulties on the condition that air-drop does not cause damage to blood units.
METHODS:
After a period of study and technical development of packaging, four air-drops at medium and high altitudes were performed with an aircraft of the French Air Force. After this, one air-drop was carried out at medium altitude with 10 RBCs and 10 French lyophilised plasma (FLYP). A second air-drop was performed with a soldier carrying one FLYP unit at 12 000 feet. For these air-drops real blood products were used, and quality control testing and temperature monitoring were performed.
RESULTS:
The temperatures inside the containers were within the normal ranges. Visual inspection indicated that transfusion packaging and dumped products did not undergo deterioration. The quality control data on RBCs and FLYP, including haemostasis, suggested no difference before and after air-drop.
DISCUSSION:
The operational implementation of the air-drop of blood products seems to be one of the solutions for the supply of blood products in military austere settings or far forward on battlefield, allowing safe and early transfusion.
TCCC Update May 2018
Tuerie massive: Les 30 premières min.
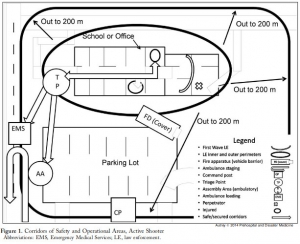
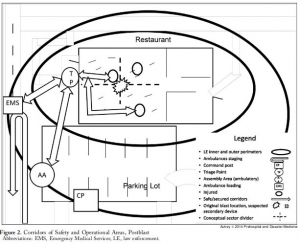
3 Echo: concept of operations for early care and evacuation of victims of mass violence
This report describes the successful use of a simple 3-phase approach that guides the initial 30 minutes of a response to blast and active shooter events with casualties: Enter, Evaluate, and Evacuate (3 Echo) in a mass-shooting event occurring in Minneapolis, Minnesota USA, on September 27, 2012. Early coordination between law enforcement (LE) and rescue was emphasized, including establishment of unified command, a common operating picture, determination of evacuation corridors, swift victim evaluation, basic treatment, and rapid evacuation utilizing an approach developed collaboratively over the four years prior to the event. Field implementation of 3 Echo requires multi-disciplinary (Emergency Medical Services (EMS), fire and LE) training to optimize performance.
This report details the mass-shooting event, the framework created to support the response, and also describes important aspects of the concepts of operation and curriculum evolved through years of collaboration between multiple disciplines to arrive at unprecedented EMS transport times in response to the event.
07/12/2018
K comme Killer ?
-----------------------------
K comme Killer ? Peut être pas, mais en tous cas plus fréquent que l'on croit.
-----------------------------
OBJECTIVE:
Fixed facilities and rapid global evacuation ensured that delayed complications of trauma, such as hyperkalemia, occurred late in the evacuation chain where renal replacement therapies were available. However, future conflicts or humanitarian disasters may involve prolonged evacuation times. We sought to quantify one potential risk of delayed evacuation by assessing hyperkalemia in combat casualties.
METHODS:
Retrospective study of military members admitted to intensive care units in Iraq and Afghanistan from February 1, 2002, to February 1, 2011. This study was approved by the U.S. Army Medical Research and Materiel Command Institutional Review Board. Demographics, injury severity score, burn injury, mechanism of injury, vital signs, creatinine, and potassium were collected. Logistic regression models were used to identify incidence and risk factors for hyperkalemia.
RESULTS:
Of 6,011 patient records, 1,472 had sufficient data to be included for analysis. Hyperkalemia occurred in 5.8% of patients. Those with hyperkalemia had higher injury severity scores, higher shock index, were more likely to have acute kidney injury, and were more likely to die. On multivariate analysis, acute kidney injury and shock index were significantly associated with the development of hyperkalemia. In a subgroup of patients with data on creatine kinase, rhabdomyolysis was associated with hyperkalemia in the univariate model, but was not significant after adjustment.
CONCLUSION:
Hyperkalemia occurred in 5.8% of patients in our cohort of critically injured combat casualties. The development of hyperkalemia was independently associated with acute kidney injury and shock index. In future conflicts, with prolonged evacuation times, mitigation strategies should be developed to treat hyperkalemia in casualties before arrival at definitive care.
Zone de confort: En sortir pour progresser ?
Biological Response to Stress During Battlefield Trauma Training: Live Tissue Versus High-Fidelity Patient Simulator.
INTRODUCTION:
Tactical Combat Casualty Care (TCCC) training imposes psychophysiological stress on medics. It is unclear whether these stress levels vary with the training modalities selected. It is also unclear how stress levels could have an impact on medical performance and skill uptake.
MATERIALS AND METHODS:
We conducted a pilot study to compare the effects of live tissue (LT) with a high-fidelity patient simulator (SIM) on the level of stress elicited, performance, and skill uptake during battlefield trauma training course in an operating room (OR) and in a simulated battlefield scenario (field). In the report, we studied the effects of training modalities and their changes on stress levels by measuring different biomarkers (salivary amylase, plasma catecholamines, and neuropeptide Y) at various time points during the trauma training course.
RESULTS:
We found that the training resulted in significant psychophysiological stress as indicated by elevated levels of various biomarkers relative to baseline immediately after both OR and field assessment (p < 0.05). Compared with pre-OR levels, the LT training in the OR resulted in significant increases in the plasma levels of epinephrine, norepinephrine, and neuropeptide (p = 0.013, 0.023, 0.004, respectively), whereas the SIM training in the OR resulted in significant increases in the plasma levels of norepinephrine and neuropeptide (p = 0.003 and 0.008). Compared with pre-field levels, we found significant increases in plasma epinephrine concentration in the SIM group (p = 0.016), plasma norepinephrine concentration in the LT group (p = 0.015), and plasma neuropeptide Y concentration in both LT (p = 0.006) and SIM groups (p = 0.029). No differences in the changes of biomarker levels were found between LT and SIM groups in the OR and field. Compared with pre-field levels, the testing on the same modality as that in the OR in the simulated battlefield resulted in significant increases in norepinephrine and neuropeptide levels (p = 0.013 and 0.015), whereas the testing on different modalities resulted in significant increases in amylase, epinephrine, and neuropeptide levels (p = 0.016, 0.05, 0.018, respectively). There was a significantly larger increase in plasma norepinephrine concentration (p = 0.031) and a trend toward a greater increase in the salivary amylase level (p = 0.052) when the field testing involved a different modality than the OR compared with when OR and field testing involved the same modality. Although most of the biomarkers returned to baseline levels after 24 h, plasma norepinephrine levels remained significantly higher regardless of whether field testing occurred on the same or different modality compared with OR (p = 0.040 and 0.002).
CONCLUSION:
TCCC training led to significant increase in psychophysiological stress, as indicated by elevated levels of various biomarkers. The training modalities did not result in any differences in stress levels, whereas the switch in training modalities appeared to elicit greater stress as evidenced by changes in specific biomarkers (amylase and norepinephrine). A comparative study with a larger sample size is warranted.
05/12/2018
Crico: Manque d'expérience/Entraînement
Emergency front-of-neck airway by ENT surgeons and residents: A dutch national survey
----------------------------
Ce travail hollandais met en avant le caractère non anecdotique des accès chirurgicaux aux voies aériennes. Pour les chirurgiens ORL hollandais, il s'agit essentiellement de trachéotomies. Le faible recours à la coniotomie s'explique surtout par le manque d'entraînement et d'équipements spécifiques. L'article souligne l'importance des démarches d'acquisition et de maintien des compétences, ce qui ne doit pas nous étonner. Comme pour les chirurgiens ORL le besoin d'un programme structuré de formations à l'accès aux voies aériennes en condition de combat est un impératif.
----------------------------
Objectives:
ENT surgeons and anesthesiologists work closely together in managing challenging airway cases. Sharing knowledge, experiences, and expectations interdisciplinary is essential in order to facilitate decision-making and adequate management in emergency front-of-neck airway cases.
Methods:
A survey was performed, to analyze level of experience, technique of preference, training, knowledge of material and protocols, and self-efficacy scores of Dutch ENT surgeons and residents in performing an urgent or emergency front-of-neck airway.
Results:
Within one year (January 2014-2015), 25.7% of the 257 respondents had performed an urgent or emergency front-of-neck airway. Of all reported emergency front-of-neck airways (N = 30), 80% were managed by tracheotomy. In future emergency front-of-neck airway cases, 74% stated cricothyrotomy would be their technique of preference. The majority would choose an uncuffed large-bore cannula technique. Post-academic hands-on training was attended by 42% of respondents. Self-efficacy scores were highest for surgical tracheotomy, and higher when trained or experienced. In case of an emergency scenario, 8.6% would not perform a front-of-neck airway themselves.


The main reasons for reluctance to start in general were lack of experience and lack of training. Reported items for improvement were mainly the development of a protocol and training.
Conclusion:
The chance of encountering an airway emergency scenario requiring front-of-neck airway is realistic. There is inconsistency between advised technique, technique of preference and technique actually performed by ENT surgeons. This study shows that there is both a need and desire for improvement in training and organization of care. Interdisciplinary guidelines and education is needed and could eventually safe lives.
| Tags : airway
02/12/2018
Crico: Incisez VERTICAL et LARGE
Emergency cricothyroidotomy: an observational study to estimate optimal incision position and length
Background
A vertical incision is recommended for cricothyroidotomy when the anatomy is impalpable, but no evidence-based guideline exists regarding optimum site or length. The Difficult Airway Society guidelines, which are based on expert opinion, recommend an 80–100 mm vertical caudad to cephalad incision in the extended neck position. However, the guidelines do not advise the incision commencement point. We sought to determine the minimum incision length and commencement point above the suprasternal notch required to ensure that the cricothyroid membrane would be accessible within its margins.
Methods
We measured using ultrasound, in 80 subjects (40 males and 40 females) without airway pathology, the distance between the suprasternal notch and the cricothyroid membrane, in the neutral and extended neck positions. We assessed the inclusion of the cricothyroid membrane within theoretical incisions of 0–100 mm in length made at 10 mm intervals above the suprasternal notch.
Results
In 80 subjects (40 males and 40 females), the distance ranged from 27 to 105 mm. Movement of the cricothyroid membrane on transition from the neutral to extended neck position varied from 15 mm caudad to 27 mm cephalad.
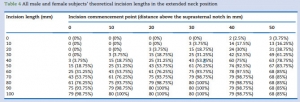
The minimum incision required in the extended position was 70 mm in males and 80 mm in females, commencing 30 mm above the suprasternal notch.
Conclusions
An 80 mm incision commencing 30 mm above the suprasternal notch would include all cricothyroid membrane locations in the extended position in patients without airway pathology, which is in keeping with the Difficult Airway Society guidelines recommended incision length.
| Tags : airway