27/11/2018
Adolphe Diagne

Adolphe Diagne est né le 17 octobre 1907 à Paris. Son père est un homme politique français d'origine sénégalaise. Il entre en 1927 à l'école principale du Service de Santé de la Marine et des troupes coloniales (Ecole de Santé Navale). Il obtient son doctorat et sert comme médecin-lieutenant dans les troupes coloniales en Mauritanie. Promu médecin-capitaine en 1936, il est affecté au Sénégal puis au Tchad.
Le 26 août 1940, lors du ralliement du Tchad auquel il participe activement, il s'engage dans les Forces françaises libres à Fort Lamy et participe à l'ensemble des combats de la seconde guerre mondiale. Compagnon de la libération, Il termine la guerre avec le grade de médecin-commandant. En 1946, il fut nommé médecin-chef au service d’Hygiène de Dakar, puis promu médecin-lieutenant-colonel en 1949. Il devint ensuite premier conseiller du du haut-commissaire auprès de la République du Sénégal en 1959 et, enfin, chargé de mission auprès du ministre de la Coopération en 1962. Il a occupé des postes à haute responsabilité au sein du SSA avant d'être nommé inspecteur du Service de Santé pour l'Armée de Terre en 1969.
Adolphe Diagne est décédé le 28 février 1985 à l'hôpital du val de Grâce à Paris. Il est inhumé à Lourmarin (Vaucluse).
- Commandeur de la Légion d'Honneur
- Compagnon de la Libération - décret du 18 janvier 1946
- Grand Officier de l'Ordre National du Mérite
- Croix de guerre 39/45 (3 citations)
- Médaille de la Résistance avec Rosette
- Médaille Coloniale avec agrafes "AFL", "Fezzan"
- Médaille Commémorative 39/45 avec agrafe "Afrique-Libération"
- Officier de la Santé Publique
- Officier de l'Etoile Noire du Bénin
- Officier de l'Etoile Noire d'Anjouan
20/11/2018
The MARCH belt
De quoi avoir sur soi et sans ouvrir son sac pour réaliser le MARCH

CRO MARCH Belt (CROMEDICALGEAR.COM)
09/11/2018
Tourniquet abdominal: OK pour 60 min mais max 240 min
Abdominal Aortic and Junctional Tourniquet release after 240 minutes is survivable and associated with small intestine and liver ischemia after porcine class II hemorrhage.
Uncontrolled hemorrhage is a leading cause of tactical trauma-related deaths. Hemorrhage from the pelvis and junctional regions are particularly difficult to control due to the inability of focal compression. The Abdominal Aortic and Junctional Tourniquet (AAJT) occludes aortic blood flow by compression of the abdomen. The survivability of tourniquet release beyond 120 minutes is unknown and fluid requirements to maintain sufficient blood pressure during prolonged application are undetermined. We therefore compared 60-minute and 240-minute applications and release of the AAJT for 30 minutes, with crystalloid fluid therapy, after a Class II hemorrhage.
METHODS:
Sixty-kilogram anesthetized pigs were subjected to 900-mL hemorrhage and AAJT application for 60 minutes (n = 5), 240 minutes (n = 5), and fluid therapy only for 240 minutes (n = 5) and reperfusion for 30 minutes.
RESULTS:
The AAJT application was hemodynamically and respiratory tolerable for 60 minutes and 240 minutes. Cumulative fluid requirements decreased by 64%, comparable to 3000 mL of crystalloids. Mechanical ventilation was impaired. AAJT increased the core temperature by 0.9°C compared with fluid therapy. Reperfusion consequences were reversible after 60 minutes but not after 240 minutes. A 240-minute application resulted in small intestine and liver ischemia, persisting hyperkalemia, metabolic acidosis, and myoglobinemia, suggesting rhabdomyolysis.
CONCLUSION:
The AAJT application for 240 minutes with reperfusion was survivable in an intensive care setting and associated with abdominal organ damage. Long time consequences and spinal cord effects was not assessed. We propose an application time limit within 60 minutes to 240 minutes, though further studies are needed to increase the temporal resolution. The AAJT application may be considered as a rescue option to maintain central blood pressure and core temperature in cases of hemorrhagic shock from extremity bleedings, if fluid therapy is unavailable or if the supply is limited.
08/11/2018
Tourniquet abdominal: Le - longtemps possible
Long-term consequences of abdominal aortic and junctional tourniquet for hemorrhage control
Kheirabadi BS et Al. J Surg Res. 2018 Nov;231:99-108.
BACKGROUND:
Specialized tourniquets have been deployed to the battlefield for the control of junctional/pelvic hemorrhage despite limited knowledge concerning their safety and duration of use. This study investigated long-term effects of abdominal application of the abdominal aortic and junctionaltourniquet (AAJT) in a swine survival model.
METHODS:
Anesthetized spontaneously air-breathing swine were subjected to bilateral femoral artery injuries and subsequent 40% hemorrhage. Further hemorrhage was controlled by applying the AAJT on the lower abdomen for 0 h (n = 2, controls), 1 h (n = 6), 1.5 h (n = 6), or 2 h (n = 3). Before tourniquet release, arterial injuries were repaired, and mechanical ventilation and rapid crystalloid fluid were provided for at least 5 min. Additional fluid and 500 mL autologous blood were transfused after restoring blood flow. Animals were recovered and their mobility and health monitored up to 2 wk.
RESULTS:
AAJT application occluded the infrarenal abdominal aorta and stopped bilateral groin hemorrhage with rapid reversal of hemorrhagic shock and improved cranial blood pressure. All animals including controls recovered overnight but regaining hind leg function varied among AAJT-treated groups.
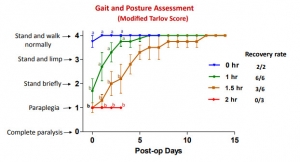
In contrast to 1 h AAJT-treated swine that recovered full mobility in 1 wk, 2 h animals developed persistent hind leg paraplegia concurrent with urinary retention and ischemic necrosis of lumber muscles and had to be euthanized 3 d after surgery. Half of the 1.5-h group also had to be euthanized early due to paraplegia, whereas the other half recovered motor function within 2 wk.
CONCLUSIONS:
The results of this animal study indicated that ischemic reperfusion injuries associated with abdominal application of the AAJT were time-dependent. To avoid permanent injuries, AAJT application on the abdomen to control a groin hemorrhage could not be longer than 1 h. This was consistent with recent instructions for application of this tourniquet on the abdomen in patients
Tourniquet abdominal = REBOA Zone 3
Comparison of zone 3 Resuscitative Endovascular Balloon Occlusion of the Aorta and the Abdominal Aortic and Junctional Tourniquet in a model of junctional hemorrhage in swine
BACKGROUND:
Traumatic injuries to the pelvis and high junctional injuries are difficult to treat in the field; however, Resuscitative EndovascularBalloon Occlusion of the Aorta (REBOA) and the Abdominal Aortic and Junctional Tourniquet (AAJT) constitute two promising treatment modalities. The aim of this study is to use a large animal model of pelvic hemorrhage to compare the survival, hemostatic, hemodynamic, and metabolic profile of both techniques.
METHODS:
Yorkshire swine (n = 10, 70-90 kg) underwent general anesthesia, instrumentation, and surgical isolation of the femoral artery. Uncontrolled hemorrhage was initiated by an arteriotomy. Animals were randomly allocated to either REBOA or AAJT. Following completion of device application, both groups received a 500 mL Hextend bolus. After 1 hour, the injured femoral artery was ligated to simulate definitive hemostasis followed by a second Hextend bolus and device removal. Animals were observed for two more hours. Physiological data were collected throughout the experiments and compared between groups.
RESULTS:
Both techniques achieved 100% hemostasis, and all animals survived the entire experiment except one in the REBOA group. During the hour treatment phase, the AAJT group had a higher mean arterial pressure than the REBOA group (59.9 ± 16.1 versus 44.6 ± 9.8 mm Hg, respectively; P < 0.05). The AAJT-treated group had higher lactate levels than the REBOA-treated group (4.5 ± 2.0 versus 3.2 ± 1.3 mg/dL, respectively; P < 0.05).
CONCLUSIONS:
Despite their mechanistic differences, both techniques achieved a similar hemostatic, hemodynamic, and metabolic profile. Some differences do exist including lactate levels and blood pressure.
Transport du sang en opex: Loin d'être anodin !
Bringing Packed Red Blood Cells to the Point of Combat Injury: Are We There Yet?
Ünlü et Al.Turk J Haematol. 2018 Aug 3;35(3):185-191.
-------------------------------
Transfuser le plus tôt possible serait un facteur de survie chez le blessé de guerre. Encore faut il disposer de sang et donc d'en transporter. On connaît les règles imposées en métropole. Les conditions de transport en opérations 'ont rien à voir avec celles de métropole. C'est bien ce que décrit cet article qui incite à la prudence. Seules 13% de poches récentes soumises à des vibrations intenses peuvent être transfusées après 06h d'exposition à des vibrations intenses.
-------------------------------
OBJECTIVE:
Hemorrhage is the leading cause of injury-related prehospital mortality. We investigated worst-case scenarios and possible requirements of the Turkish military. As we plan to use blood resources during casualty transport, the impact of transport-related mechanical stress on packed red blood cells (PRBCs) was analyzed.
MATERIALS AND METHODS:
The in vitro experiment was performed in the environmental test laboratories of ASELSAN®. Operational vibrations of potential casualty transport mediums such as Sikorsky helicopters, Kirpi® armored vehicles, and the NATO vibration standard MIL-STD-810G software program were recorded. The most powerful mechanical stress, which was created by the NATO standard, was applied to 15 units of fresh (≤7 days) and 10 units of old (>7 days) PRBCs in a blood cooler box. The vibrations were simulated with a TDS v895 Medium-Force Shaker Device. On-site blood samples were analyzed at 0, 6, and 24 h for biochemical and biomechanical analyses.
RESULTS:
The mean (±standard deviation) age of fresh and old PRBCs was 4.9±2.2 and 32.8±11.8 days, respectively. Six-hour mechanical damage of fresh PRBCs was demonstrated by increased erythrocyte fragmentation rates (p=0.015), hemolysis rates (p=0.003), and supernatant potassium levels (p=0.003) and decreased hematocrit levels (p=0.015). Old PRBC hemolysis rates (p=0.015), supernatant potassium levels (p=0.015), and supernatant hemoglobin (p=0.015) were increased and hematocrit levels were decreased (p=0.015) within 6 h.

Two (13%) units of fresh PRBCs and none of the old PRBCs were eligible for transfusion after 6 h of mechanical stress.
CONCLUSION:
When an austere combat environment was simulated for 24 h, fresh and old PRBC hemolysis rates were above the quality criteria. Currently, the technology to overcome this mechanical damage does not seem to exist. In light of the above data, a new national project is being performed.
02/11/2018
Blessés admis en role 2: Le bilan afghan
A Review of Casualties Transported to Role 2 Medical Treatment Facilities in Afghanistan.
---------------------------------------
Ce document met en évidence tout l'apport d'une chaine coordonnée de prise en charge du traumatisé par des équipes entraînées appliquant une stratégie médico-chirurgicale moderne.
---------------------------------------
Critically injured trauma patients benefit from timely transport and care. Accordingly, the provision of rapid transport and effective treatment capabilities in appropriately close proximity to the point of injury will optimize time and survival. Pre-transport tactical combat casualty care, rapid transport with en route casualty care, and advanced damage control resuscitation and surgery delivered early by small, mobile, forward-positioned Role 2 medical treatment facilities have potential to reduce morbidity and mortality from trauma. This retrospective review and descriptive analysis of trauma patients transported from Role 1 entities to Role 2 facilities in Afghanistan from 2008 to 2014 found casualties to be diverse in affiliation and delivered by various types and modes of transport. Air medical evacuation provided transport for most patients, while the shortest transport time was seen with air casualty evacuation. Although relatively little data were collected for air casualty evacuation, this rapid mode of transport remains an operationally important method of transport on the battlefield. For prehospital care provided before and during transport, continued leadership and training emphasis should be placed on the administration and documentation of tactical combat casualty care as delivered by both medical and non-medical first responders.
01/11/2018
Combat urbain: Problématique

