31/05/2019
Hémorragie du tronc non compressible: MEDEVAC COURTE
Impact of prehospital medical evacuation (MEDEVAC) transport time on combat mortality in patients with non-compressible torso injury and traumatic amputations: a retrospective study
BACKGROUND:
In combat operations, patients with traumatic injuries require expeditious evacuation to improve survival. Studies have shown that long transport times are associated with increased morbidity and mortality. Limited data exist on the influence of transport time on patient outcomes with specific injury types. The objective of this study was to determine the impact of the duration of time from the initial request for medical evacuation to arrival at a medical treatment facility on morbidity and mortality in casualties with traumatic extremity amputation and non-compressible torso injury (NCTI).
METHODS:
We completed a retrospective review of MEDEVAC patient care records for United States military personnel who sustained traumatic amputations and NCTI during Operation Enduring Freedom between January 2011 and March 2014. We grouped patients as traumatic amputation and NCTI (AMP+NCTI), traumatic amputation only (AMP), and neither AMP nor NCTI (Non-AMP/NCTI). Analysis was performed using chi-squared tests, Fisher's exact tests, Cochran-Armitage Trend tests, Shapiro-Wilks tests, Wilcoxon and Kruskal-Wallis techniques and Cox proportional hazards regression modeling.
RESULTS:
We reviewed 1267 records, of which 669 had an injury severity score (ISS) of 10 or greater and were included in the analysis. In the study population, 15.5% sustained only amputation injuries (n=104, AMP only), 10.8% sustained amputation and NCTI (n=72, AMP+NCTI), and 73.7% did not sustain either an amputation or an NCTI (n=493, Non-AMP/NCTI). AMP+NCTI had the highest mortality (16.7%) with transport time greater than 60 min. While the
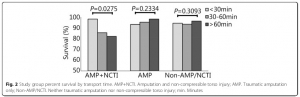
AMP+NCTI group had decreasing survival with longer transport times, AMP and Non-AMP/NCTI did not exhibit the same trend.
CONCLUSIONS:
A decreased transport time from the point of injury to a medical treatment facility was associated with decreased mortality in patients who suffered a combination of amputation injury and NCTI. No significant association between transport time and outcomes was found in patients who did not sustain NCTI. Priority for rapid evacuation of combat casualties should be given to those with NCTI.
29/05/2019
Procédure EVDG du sauvetage au comba
| Tags : procédure, evdg, procedure evdg
19/05/2019
Frères de sang, petite histoire de la transfusion
Émile Jeanbrau, Georges Dehelly, Maurice Guillot, Albert Hustin, Bruce et Oswald Robertson
Jean Baptiste Denis (1635 - 1704) réalise la première transfusion de sang chez l'Homme le 15 juin 1667. Le patient est un jeune homme de 15-16 ans, atteint de fièvre depuis deux mois, et déjà traité par plus de 20 saignées ! Il présente une perte de mémoire et une incapacité à produire le moindre effort, signes attribués par Denis à l'effet des saignées. Le traitement transfusionnel consiste en fait en l'échange de 3 onces (environ 100 mL) de sang du patient contre 9 onces (environ 300 mL) de sang de mouton. Le suivi à court terme montre une amélioration clinique très rapide, avec reprise de l'activité.
C'est le 27 mars 1914 qu'est réussie dans l'Histoire la première transfusion sanguine par poche, réalisée en BELGIQUE par Albert HUSTIN sur un patient anémié par des hémorragies coliques de longue durée. Au PAYS BASQUE, le 16 octobre 1914 a eu lieu, à l'Hôpital de BIARRITZ, la première transfusion sanguine directe de la première Guerre Mondiale : Isidore COLAS, un soldat breton (né à BANNALEC) en convalescence à la suite d'une blessure à la jambe, sauve par le don de son sang le Caporal Henri LEGRAIN (origine de LAON dans l'Aisne) du 45ème d'Infanterie, arrivé exsangue du Front. Leurs sangs devaient être compatibles puisque l'opération réussit. "Je le vis peu à peu se recolore et renaître à la vie" expliqua un des médecins
"On a rapporté récemment un cas de transfusion effectué avec plein de succès à Montpellier par le docter Jeanbrau et le professeur Hedon. Notre photographe représente les deux frères d'armes, devenus frères de sang, vingt-cinq jours après la transfusion qui sauva l'un grâce au sacrifice de l'autre: à gauche, le soldat réserviste Créchet, du 68e de ligne, amputé après une terrible hémorragie; à droite, le "donneur", Emile Barthélémy, du 81e de ligne, légèrement blessé à Gerbeviller" source
Tout ceci a été rendu possible dans les armées françaises grâce à l'investissement du Pr Jeanbrau, pionner de la transfusion en France.
Natif d’Alès, il étudie la médecine à Montpellier, jusqu’au doctorat en 1898 ; il devient chirurgien et s’oriente vers l’urologie. En 1914 il est mobilisé comme chirurgien à l’hôpital d’évacuation de Biarritz. Le 16 octobre, il transfuse parla technique de la canule d’Elsberg le soldat Henri Legrain, blessé le 28 septembre, amputé de la cuisse droite. Le donneur est un éclopé, le soldat Isidore Colas (on appelait “éclopé”, dans le langage de la médecine militaire, un blessé léger, convalescent). Henri Legrain guérit ; il mourut en 1987, à l’âge de 97 ans ! Émile Jeanbrau pratiqua quelques autres transfusions à l’aide de la canule d’Elsberg.
Mais, jugeant l’opération “trop difficile, trop minutieuse et trop longue pour entrer dans la pratique d’urgence”, il passa au tube de Kimpton-Brown paraffiné, qu’il améliora progressivement dans les années suivantes (modifications de forme, de volume, du système d’aspiration et d’insufflation, introduction de 25 à 30 ml d’une solution de citrate de sodium). Il était alors, près du front, chirurgien-chef de l’ambulance automobile chirurgicale (“Autochir”) n°13.
Du début du conflit jusqu’à la fin de 1914, on estime à 50, tout au plus, les transfusions sanguines pratiquées sur des blessés de l’armée française, et par Émile Jeanbrau, Georges Dehelly et Maurice Guillot pour la plupart.
Georges Dehelly s’était formé à la transfusion sanguine, avant-guerre, lors d’un stage de perfectionnement auprès de Crile aux États-Unis. Il fut l’auteur, avec Maurice Guillot etLouis Morel d’un d es premiers ouvrages français sur la transfusion sanguine .
Un point anecdotique de la transfusion sanguine dans la période 1914-1916 concerne un vieux général français. Au printemps de 1916, épuisé par la maladie, il démissionne de son poste de ministre de la Guerre. Le 18 mai, il est opéré de la prostate dans une clinique de Versailles. Après une hématurie massive il est transfusé, le donneur étant son chirurgien lui-même ! Il décède néanmoins, le lendemain 27 mai : Joseph Simon Gallieni (1849-1916), gouverneur militaire de Paris en août 1914, l’homme des “taxis de la Marne”, est donc très vraisemblablement le premier général de l’armée française à recevoir une transfusion sanguine. source
Lire: La transfusion sanguine pendant la Grande Guerre (1914 - 1918).
Salé 7,5%: Ne pas dépasser 500 ml
The effects of hypertonic saline solution (7.5%) on coagulation and fibrinolysis: an in vitro assessment using thromboelastography.
-----------------------------------
Ce travail met en avant le caractère dose-dépendant des effets des solutions hypertoniques salines sur la coagulation. Elle confirme des travaux plus anciens (1) et milite au moins pour une utilisation raisonnée, limitée à deux administrations. Ceci est cohérent avec la proposition faite par la procédure du sauvetage au combat.
-----------------------------------
We studied the effects of hypertonic (7.5%) and normal saline on coagulation and fibrinolysis in an in vitro model using thromboelastography of human whole blood. Reaction times increased and alpha angles decreased with hypertonic saline replacement at 7.5% blood volume compared with similar dilution with normal saline.
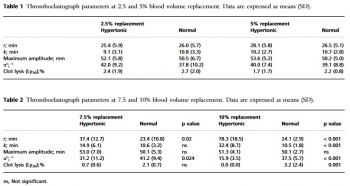
At 10% blood volume replacement with hypertonic saline, reaction and coagulation times were significantly increased and alpha angles were decreased. Clot lysis at 30 min was also significantly reduced. We conclude that 7.5% hypertonic saline solution has anticoagulant effects if it replaces 7.5% or more of blood volume.
16/05/2019
Penthrox: Peut-être MAIS l'hyperthermie maligne ?
Penthrox: a breath of PHEC air for the military?
----------------------------------------
Le penthrox est souvent présenté comme une nouveauté. Il s'agit d'un agent d'anesthésie ancien dont l'emploi a cessé du fait, entre autres, d'une nephrotoxicité importante. Comme tous les agents anesthésiques halogénés, il possède une activité analgésique vraie. Il est aussi potentiellement un agent déclenchant d'hyperthermie maligne anesthésique. Les auteurs font une présentation de ce produit en omettant d'aborder ce problème potentiel dont on sait qu'il touche (délai et doses déclenchantes) de manière diverse tous les halogénés (1)
----------------------------------------
Prehospital analgesia is vital to good clinical care and inhaled methoxyflurane (Penthrox) would be a valuable addition to the armed forces medical armoury. Penthrox would provide strong, fast-acting, self-administered and safe analgesia to patients with moderate to severe injuries. In addition, it would provide an option for strong analgesia which would not be subject to the regulations that govern controlled or accountable drugs which gives it a unique position as the military moves its focus from large enduring operations to small short-term training teams supported by lone combat medics in remote locations across the globe.
PST hémostatiques: Equivalents mais bases scientifiques pauvres
Systematic review of prehospital haemostatic dressings.
INTRODUCTION:
Haemorrhage is one of the leading causes of battlefield and prehospital death. Haemostatic dressings are an effective method of limiting the extent of bleeding and are used by military forces extensively. A systematic review was conducted with the aim of collating the evidence on current haemostatic products and to assess whether one product was more effective than others.
METHODS:
A systematic search and assessment of the literature was conducted using 13 health research databases including MEDLINE and CINAHL, and a grey literature search. Two assessors independently screened the studies for eligibility and quality. English language studies using current-generation haemostatic dressings were included. Surgical studies, studies that did not include survival, initial haemostasis or rebleeding and those investigating products without prehospital potential were excluded.
RESULTS:
232 studies were initially found and, after applying exclusion criteria, 42 were included in the review. These studies included 31 animal studies and 11 clinical studies. The outcomes assessed were subject survival, initial haemostasis and rebleeding. A number of products were shown to be effective in stopping haemorrhage, with Celox, QuikClot Combat Gauze and HemCon being the most commonly used, and with no demonstrable difference in effectiveness.
CONCLUSIONS:
There was a lack of high-quality clinical evidence with the majority of studies being conducted using a swine haemorrhage model. Iterations of three haemostatic dressings, Celox, HemCon and QuikClot, dominated the studies, probably because of their use by international military forces and all were shown to be effective in the arrest of haemorrhage.
Hémorragie: Garrot, mais aussi COMPRESSION
Bleeding control in combat fields with extreme transfer time

| Tags : tourniquet
12/05/2019
Réchauffeur: M Warmer, the best ?
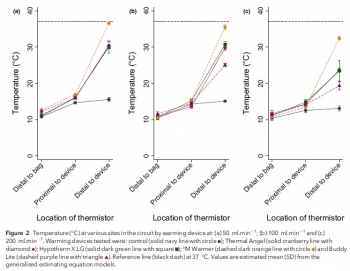
Comparison of portable blood-warming devices under simulated pre-hospital conditions: a randomised in-vitro blood circuit study.
---------------------------------------------
Lire aussi cet article qui met en avant la performance du Qiflow warmer
---------------------------------------------
Pre-hospital transfusion of blood products is a vital component of many advanced pre-hospital systems. Portable fluid warmers may be utilised to help prevent hypothermia, but the limits defined by manufacturers often do not reflect their clinical use. The primary aim of this randomised in-vitro study was to assess the warming performance of four portable blood warming devices (Thermal Angel, Hypotherm X LG, °M Warmer, Buddy Lite) against control at different clinically-relevant flow rates. The secondary aim was to assess haemolysis rates between devices at different flow rates. We assessed each of the four devices and the control, at flow rates of 50 ml.min-1 , 100 ml.min-1 and 200 ml.min-1 , using a controlled perfusion circuit with multisite temperature monitoring. Free haemoglobin concentration, a marker of haemolysis, was measured at multiple points during each initial study run with spectrophotometry. At all flow rates, the four devices provided superior warming performance compared with the control (p < 0.001). Only the °M Warmer provided a substantial change in temperature at all flow rates (mean (95%CI) temperature change of 21.1 (19.8-22.4) °C, 20.4 (19.1-21.8) °C and 19.4 (17.7-21.1) °C at 50 ml.min-1 , 100 ml.min-1 and 200 ml.min-1 , respectively).
There was no association between warming and haemolysis with any device (p = 0.949) or flow rate (p = 0.169). Practical issues, which may be relevant to clinical use, also emerged during testing. Our results suggest that there were significant differences in the performance of portable blood warming devices used at flow rates encountered in clinical practice.
05/05/2019
Pour savoir, se ets'in/former
The effectiveness of educational methods for cricothyroid membrane identification by dental students: A prospective study using neck photographs and tracheotomy trainers.
Goto T et Al. Clin Exp Dent Res. 2019 Mar 4;5(2):170-177.
The purpose of this study was to evaluate the accurate identification of the cricothyroid membrane (CTM) by fifth grade dental students, before undergoing the relevant anesthesiology practicum. Moreover, we aimed to determine the educational effectiveness of the cricothyrotomy practicum in anesthesiology.
Before the lecture and without prior notification, 119 students were provided with a photograph of a man's neck and instructed to attach a blue sticker to the cricothyrotomy puncture site and to a palpable tracheotomy trainer, after applying sufficient palpation. After this, students attended a 60-min lecture on the emergency airway management method. Two and 16 days after the lecture and practicum, students were presented with a new neck photograph and the tracheotomy trainer and asked again to place stickers (red stickers: at 2 days; green stickers: at 16 days) on the cricothyrotomy penetration site. The data were analyzed with an image processing software, by superimposing the 119 stickers on the neck photographs and tracheotomy trainers, to visually examine the accuracy of CTM identification.
The rate of correct sticker placement in the neck photographs was 41.2% before the lecture, 80.7% 2 days after the lecture, and 77.3% 16 days after the lecture (before vs. 2 and 16 days after, p value < 0.01). For the tracheotomy trainer, the rate was 36.1% before the lecture, 97.5% 2 days after the lecture, and 94.1% 16 days after the lecture (before vs. 2 and 16 days after, p value < 0.01).
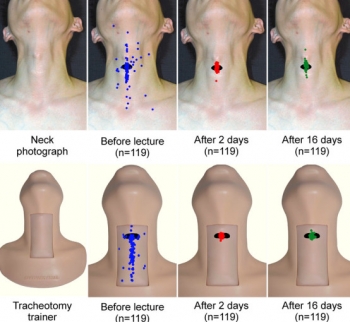
Furthermore, the proportion of students with mistakes above and below the CTM was higher than that of students with mistakes to the right or left. In conclusion, the rate of accurate CTM identification among dental students was low before they underwent the relevant practicum, but most students were able to identify the CTM accurately after the lecture and practicum in a small class.
02/05/2019
Tourniquet gonflable: Un nouveau venu
Rescue Bandage TQ Inflatable Tourniquet

Un garrot développé dans le cadre de la campagne STOP THE BLEED.
Apprendre à poser un garrot: En fait, pas si simple
Can they stop the bleed? Evaluation of tourniquet application by individuals with varying levels of prior self-reported training.
McCarty et Al. Injury. 2019 Jan;50(1):10-15. doi: 10.1016/j.injury.2018.09.041.
1 garrot sur 3 posé correctement malgré une formation ad-hoc.
--------------------------------------------------------
BACKGROUND:
Application of extremity tourniquets is a central tenet of multiple national initiatives to empower laypersons to provide hemorrhage control (HC). However, the efficacy of the general population who self-report prior first-aid (FA) or HC training on individual's ability to control bleeding with a tourniquet remains unknown. Therefore, the objective of this study was to assess the effectiveness of laypeople with self-reported prior FA or HC training to control bleeding with a tourniquet.
STUDY DESIGN:
Employees of a stadium were assessed via simulation in their ability to apply a Combat Application Tourniquet. As a subgroup analysis of a larger study, participants who self-reported: 1) No prior training, 2) FA training only or 2) FA + HC training were compared. Logistic regression adjusting for age, gender, education, willingness-to-assist, and comfort level in HC was performed.
RESULTS:
317 participants were included. Compared to participants with no prior training (14.4%,n = 16/111), those with FA training only (25.2%,n = 35/139) had a 2.12-higher odds (95%CI:1.07-4.18) of correct tourniquet application while those with FA + HC (35.8%,n = 24/67) had a 3.50-higher odds (95%CI:1.59-7.72) of correct application. Participants with prior FA + HC were more willing-to-assist and comfortable performing HC than those without prior training (p < 0.05).
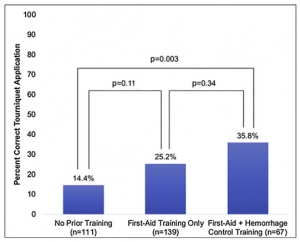
However, reporting being very willing-to-assist [OR0.83,95%CI:0.43-1.60] or very comfortable [OR1.11,95%CI:0.55-2.25] was not associated with correct tourniquet application.
CONCLUSION:
Self-reported prior FA + HC training, while associated with increased likelihood to correctly apply a tourniquet, results in only 1/3 of individuals correctly performing the skill. As work continues in empowering and training laypeople to act as immediate responders, these findings highlight the importance of effective layperson education techniques.
| Tags : tourniquet
01/05/2019
TCCC: Quoi de réalisé en réalité ?
Prehospital Interventions Performed in Afghanistan Between November 2009 and March 2014.
Lairet J et l Mil Med. 2019 Mar 1;184(Supplement_1):133-137. doi: 10.1093/milmed/usy311.
----------------------------
Le bilan des gestes réalisés par les US en afghanistan. Ces chiffres montrent l'importance tant de l'acquisition de pratiques gestuelles que et surtout du maintien des avoirs faire. La gestion des voies aériennes et les gestes de décompression thoracique représentent un enjeu majeur de performance bien plus importan que la maîtrise par quelques uns de techniques d'occlusion endovasculaire préhospitalière.
----------------------------
OBJECTIVE: Care provided to a casualty in the prehospital combat setting can influence subsequent medical interactions and impact patient outcomes; therefore, we aimed to describe the incidence of specific prehospital interventions (lifesaving interventions (LSIs)) performed during the resuscitation and transport of combat casualties.
METHODS: We performed a prospective observational, IRB approved study between November 2009 and March 2014. Casualties were enrolled as they were cared for at nine U.S. military medical facilities in Afghanistan. Data were collected using a standardized collection form. Determination if a prehospital intervention was performed correctly, performed incorrectly, or was necessary but was not performed (missed LSIs) was made by the receiving facility's medical provider.
RESULTS: Two thousand one hundred and six patients met inclusion criteria. The mean age was 25 years and 98% were male. The most common mechanism of injury was explosion 57%. There were 236 airway interventions attempted, 183 chest procedures, 1,673 hemorrhage control, 1,698 vascular access, and 1,066 hypothermia preventions implemented.
Incorrectly Performed Interventions Comparison of First 1,003 Patients to Second 1,103 Patients
| Overall Data | Interima (n = 1,003) | Post-Interim (1,103) | p-Valueb | |
|---|---|---|---|---|
| Airway Interventions | 8.9% | 8.6% | 9.0% | 0.9165 |
| Chest Procedures | 5.5% | 6.7% | 5.2% | 0.6726 |
| Vascular Access | 4.1% | 8.0% | 2.9% | <0.0001 |
| Hypothermia Prevention | 0.6% | 0.7% | 0.5% | 0.6860 |
| Hemorrhage Control | 2.1% | 2.2% | 2% | 0.8643 |
| Missed LSIs | |||
|---|---|---|---|
| Number of Missed LSIs | Total Number of Interventions + Missed Opportunities | Percentage of Missed LSIs | |
| Airway interventions | 56 | 292 | 19.2 |
| Chest procedures | 24 | 207 | 11.6 |
| Vascular access | 160 | 1,858 | 8.6 |
| Hypothermia prevention | 63 | 1,129 | 5.6 |
| Hemorrhage control | 57 | 1,730 | 3.3 |
There were 142 incorrectly performed interventions and 360 were missed.
CONCLUSIONS: In our study, the most commonly performed prehospital LSI in a combat setting were for vascular access and hemorrhage control. The most common incorrectly performed and missed interventions were airway interventions and chest procedures respectively.
Vidéos du TCCC
| Tags : tccc