10/06/2018
Exsufflation: 5 cm antérieur survie = 9 latéral
BACKGROUND:
Needle thoracostomy (NT) is a common prehospital intervention for patients in extremis or cardiac arrest due to trauma. The purpose of this study is to compare outcomes, efficacy, and complications after a change in policy related to NT in a four-county Emergency Medical Services (EMS) system with a catchment area of greater than 1.6 million people.
METHODS:
This is a before and after observational study of all patients who had NT performed in the Central California (USA) EMS system. The before, anterior midclavicular line (MCL) group consisted of all patients who underwent NT from May 7, 2007 through February 28, 2013. The after, midaxillary line (MAL) axillary group consisted of all patients who underwent NT from March 1, 2013 through January 30, 2016, after policy revisions changed the timing, needle size, and placement location for NT. All prehospital and hospital records where NT was performed were queried for demographics, mechanism of injury, initial status and post-NT clinical change, reported complications, and final outcome. The trauma registry was accessed to obtain Injury Severity Scores (ISS). Information was manually abstracted by study investigators and examined utilizing univariate and multivariate analyses.
RESULTS:
Three-hundred and five trauma patients treated with NT were included in this study, of which, 169 patients (the MCL group) were treated with a 14-gauge intravenous (IV) catheter at least 5.0-cm long at the second intercostal space (ICS), MCL after being placed in the ambulance; and 136 patients (the MAL group) were treated with a 10-gauge IV catheter at least 9.5-cm long at the fifth ICS, MAL on scene. The mean ISS was lower in the MAL cohort (64.5 versus 69.2; P=.007). The mortality rate was 79% in both groups.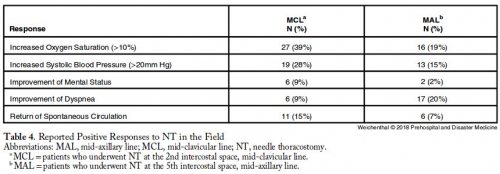
CONCLUSIONS:
Changing the timing, length of needle, and location of placement did not change mortality in patients requiring NT. Needle thoracostomy was used more frequently after the change in policy, and the MAL cohort was less injured. No increase in reported complications was noted.| Tags : exsufflation, pneumothorax
06/06/2018
Médecin de marine et petites urgences
March: Aussi chez les chinois
Expert consensus on the evaluation and diagnosis of combat injuries of the Chinese People’s Liberation Army
03/06/2018
Proectection antivectorielle: Bonnes pratiques
01/06/2018
Curare pour intuber: Oui, mais aussi !
Effects of avoidance or use of neuromuscular blocking agents on outcomes in tracheal intubation: a Cochrane systematic review.
Il est communément admis que l'emploi de curares facilite l'intubation et réduit les complications liées à ce geste. C'est bien ce que confirme cette publication. Mais cette dernière conclue également à l'importance de peser le risque bénéfice risque. Dans les conditions extrêmes d'isolement et de prise en charge de trauma maxillo-faciaux/cranien ballistique l'objectif principal doit rester l'oxygénation des blessés/accidentés. Si l'induction en séquence rapide reste la référence, l'éventualité d'une intubation sans curare sous anesthésie locale doit être évoquée en cas de risque d'impossibilité de ventilation manuelle ou spontanée et de difficulté d'intubation. Dans tous les cas il reste nécessaire de pouvoir réaliser un abord chirurgical des voies aériennes.
Lire ici les recommandations de la SFAR: Intubation difficile en anesthésie, en réanimation
---------------------------------------------
Cohort studies have indicated that avoidance of neuromuscular blocking agents (NMBA) is a risk factor for difficult tracheal intubation. However, the impact of avoiding NMBA on tracheal intubation, possible adverse effects, and postoperative discomfort has not been evaluated in a systematic review of randomised trials. We searched several databases for trials published until January 2017. We included randomised controlled trials comparing the effect of avoiding vs using NMBA. Two independent authors assessed risk of bias and extracted data. The risk of random errors was assessed by trial sequential analysis (TSA). We included 34 trials (3565 participants). In the four trials judged to have low risk of bias, there was an increased risk of difficult tracheal intubation with no use of NMBA [random-effects model, risk ratio (RR) 13.27, 95% confidence interval (CI) 8.19-21.49, P<0.00001, TSA-adjusted CI 1.85-95.04]. The result was confirmed when including all trials, (RR 5.00, 95% CI 3.49-7.15, P<0.00001, TSA-adjusted CI 1.20-20.77). There was a significant risk of upper airway discomfort or injury by avoiding NMBA (RR=1.37, 95% CI 1.09-1.74, P=0.008, TSA-adjusted CI 1.00-1.86). None of the trials reported mortality. Avoiding NMBA was significantly associated with difficult laryngoscopy, (RR 2.54, 95% CI 1.53-4.21, P=0.0003, TSA-adjusted CI 0.27-21.75). In a clinical context, one must balance arguments for using NMBA when performing tracheal intubation.