11/05/2018
Groupe O: Plus de mortalité ?
The impact of blood type O on mortality of severe trauma patients: a retrospective observational study.
BACKGROUND:
Recent studies have implicated the differences in the ABO blood system as a potential risk for various diseases, including hemostatic disorders and hemorrhage. In this study, we evaluated the impact of the difference in the ABO blood type on mortality in patients with severe trauma.
METHODS:
A retrospective observational study was conducted in two tertiary emergency critical care medical centers in Japan. Patients with trauma with an Injury Severity Score (ISS) > 15 were included. The association between the different blood types (type O versus other blood types) and the outcomes of all-cause mortality, cause-specific mortalities (exsanguination, traumatic brain injury, and others), ventilator-free days (VFD), and total transfusion volume were evaluated using univariate and multivariate competing-risk regression models. Moreover, the impact of blood type O on the outcomes was assessed using regression coefficients in the multivariate analysis adjusted for age, ISS, and the Revised Trauma Score (RTS).
RESULTS:
A total of 901 patients were included in this study. The study population was divided based on the ABO blood type: type O, 284 (32%); type A, 285 (32%); type B, 209 (23%); and type AB, 123 (13%). Blood type O was associated with high mortality (28% in patients with blood type O versus 11% in patients with other blood types; p < 0.001). Moreover, this association was observed in a multivariate model (adjusted odds ratio = 2.86, 95% confidence interval 1.84-4.46; p < 0.001). The impact of blood type O on all-cause in-hospital mortality was comparable to 12 increases in the ISS, 1.5 decreases in the RTS, and 26 increases in age.
The comparison of characteristics and outcomes between blood type O and other blood types
| Type O n = 284 |
Non-O type n = 617 |
p value | |
|---|---|---|---|
| Characteristics | |||
| Age, years (SD) | 57.3 (20.0) | 56.2 (19.4) | 0.442 |
| Female, n (%) | 64 (22.5) | 142 (23) | 0.873 |
| Charlson Comorbidity Index, median (IQR) | 0 (0–2) | 0 (0–1) | 0.829 |
| Uncrossmatched type O RBC transfusion, n (%) | 28 (9.9) | 37 (6) | 0.051 |
| RTS, (SD) | 6.85 (1.4) | 7.13 (1.2) | 0.003 |
| ISS, median (IQR) | 18 (16–25) | 19 (16–25) | 0.160 |
| AIS head, median (IQR) | 4 (3–4) | 4 (3–4) | 0.582 |
| AIS face, median (IQR) | 0 (0–0) | 0 (0–0) | 0.783 |
| AIS chest, median (IQR) | 0 (0–2) | 0 (0–3) | 0.342 |
| AIS abdomen, median (IQR) | 0 (0–0) | 0 (0–0) | 0.561 |
| AIS extremities, median (IQR) | 0 (0–2) | 0 (0–2) | 0.443 |
| AIS surface, median (IQR) | 0 (0–0) | 0 (0–0) | 0.652 |
| Outcomes | |||
| In-hospital mortality, n (%) | 80 (28.2) | 71 (11.5) | < 0.001 |
| Death due to exsanguination, n (%) | 23 (8.1) | 15 (2.4) | < 0.001 |
| Death due to TBI, n (%) | 43 (15.1) | 44 (7.1) | < 0.001 |
| Death due to other causes, n (%) | 15 (1.8) | 11 (5.3) | 0.005 |
| Ventilator-free days, mean (SD) | 18.7 (12.2) | 23.1 (9.4) | < 0.001 |
| Units of RBCs administered within 24 h, mean (SD) | 3 (9) | 2 (7) | 0.112 |
Categorical variables are expressed as numbers (%); continuous variables are presented as medians (25–75 percentiles = interquartile range (IQR))
AIS Abbreviated Injury Scale; ISS Injury Severity Score; RBC red blood cell; RTS Revised Trauma Score; SD standard deviation; TBI traumatic brain injury
Furthermore, blood type O was significantly associated with higher cause-specific mortalities and shorter VFD compared with the other blood types; however, a significant difference was not observed in the transfusion volume between the two groups.
CONCLUSIONS:
Blood type O was significantly associated with high mortality in severe trauma patients and might have a great impact on outcomes. Further studies elucidating the mechanism underlying this association are warranted to develop the appropriate intervention.
Plasma lyophilisé: Utile et mieux que PFC ?
French lyophilized plasma versus fresh frozen plasma for the initial management of trauma-induced coagulopathy: a randomized open-label trial
Garrigue D et AL; J Thromb Haemost. 2018 Mar;16(3):481-489
--------------------------
Le plasma lyophilisé retrouve d'évidence, en matière de réanimation transfusionnelle notamment celle du traumatisé, toute la place qu'il avait perdu dans les années 1980. Son atout majeur est sa disponibilité qui permet un apport bien plus précoce que le PFC. Ce travail en montre tout l'intérêt. On peut néanmoins dans ce document se poser la question de la similarité des groupes étudiés et des critères d'évaluation de la coagulopathie ?
--------------------------
Essentials
- An immediate supply of plasma in case of trauma-induced coagulopathy is required.
- The Traucc trial compared French Lyophilised Plasma (FLyP) and Fresh Frozen Plasma (FFP)
- FLyP achieved higher fibrinogen concentrations compared with FFP.
- FLyP led to a more rapid coagulopathy improvement than FFP.
Background
Guidelines recommend beginning hemostatic resuscitation immediately in trauma patients. We aimed to investigate if French lyophilized plasma (FLyP) was more effective than fresh frozen plasma (FFP) for the initial management of trauma-induced coagulopathy.
Methods In an open-label, phase 3, randomized trial (NCT02750150), we enrolled adult trauma patients requiring an emergency pack of 4 plasma units within 6 h of injury. We randomly assigned patients to receive 4-FLyP units or 4-FFP units. The primary endpoint was fibrinogen concentration at 45 min after randomization. Secondary outcomes included time to transfusion, changes in hemostatic parameters at different time-points, blood product requirements and 30-day in-hospital mortality.
Results
Forty-eight patients were randomized (FLyP, n = 24; FFP, n = 24). FLyP reduced the time from randomization to transfusion of first plasma unit compared with FFP (median[IQR],14[5-30] vs. 77[64-90] min). FLyP achieved a higher fibrinogen concentration 45 min after randomization compared with FFP (baseline-adjusted mean difference, 0.29 g L-1 ; 95% confidence interval [CI], 0.08-0.49) and a greater improvement in prothrombin time ratio, factor V and factor II. The between-group differences in coagulation parameters remained significant at 6 h. FLyP reduced fibrinogen concentrate requirements. Thirty-day in-hospital mortality rate was 22% with FLyP and 29% with FFP.
Conclusion FLyP led to a more rapid, pronounced and extended increase in fibrinogen concentrations and coagulopathy improvement compared with FFP in the initial management of trauma patients. FLyP represents an attractive option for trauma management, especially when facing logistical issues such as combat casualties or mass casualties related to terror attacks or disasters.
01/05/2018
Tourniquet: Une vieille histoire
A brief history of the tourniquet
Welling DR et Al. Vasc Surg 2012;55:286-90
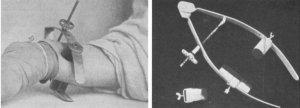
Le compresseur de Matas
| Tags : tourniquet
