12/12/2025
TXA: 2g IV si trauma crânien
Optimal dose of tranexamic acid in traumatic brain injury: Systematic review and network meta-analysis of randomized controlled trials
Shu U et Al Journal of Trauma and Acute Care Surgery 98(5):p 816-823, May 2025.
BACKGROUND
Tranexamic acid (TXA) has been used to treat traumatic brain injury (TBI); however, no definitive conclusions have been drawn regarding its effectiveness or dosage. This study evaluated the optimal TXA dose for treating TBI using a network meta-analysis (NMA).
METHODS
Five databases were searched for peer-reviewed randomized controlled trials (RCTs) published from inception to May 2024. The inclusion criteria were as follows: (1) RCTs, (2) patients older than 1 month with TBI, (3) interventions of TXA and control, (4) primary outcomes of mortality and poor neurological outcomes and secondary outcomes of vascular occlusive events, and (5) full-text peer-reviewed articles. Two reviewers independently screened and extracted the data and assessed the risk of bias. Frequency-based NMA was performed using the Grading of Recommendations, Assessment, Development, and Evaluation working-group approach.
RESULTS
We included 10 RCTs comprising 11,237 patients with TBI. Placebo showed higher mortality compared with that of a 2-g bolus of TXA (risk ratio, 1.53; 95% confidence interval, 1.08–2.17). Higher mortality was observed with a 1-g bolus of TXA followed by 1-g maintenance TXA compared with that of a 2-g bolus of TXA (risk ratio, 1.44; 95% confidence interval, 1.02–2.03). No significant differences in poor neurological outcomes or vascular occlusive events were observed between the treatment groups.

CONCLUSION
Placebo and a 1-g bolus followed by 1-g maintenance TXA were associated with higher mortality rates than those of a 2-g bolus of TXA. No difference in vascular occlusive events was observed with either treatment, indicating that our NMA recommends 2 g of TXA. However, the data for the 2-g bolus of TXA were from a single study, and further research is needed to draw definitive conclusions.
12/08/2019
Evolution de la psychiatrie militaire
01/08/2016
La guerre, et après ?
| Tags : ptsd
26/11/2015
Kétamine pour le PTSD: Oui!
Efficacy of Intravenous Ketamine for Treatment of Chronic Posttraumatic Stress Disorder. A Randomized Clinical Trial
Feder A. et Al. JAMA Psychiatry. 2014 Jun;71(6):681-8. doi: 10.1001/jamapsychiatry.2014.62
Importance Few pharmacotherapies have demonstrated sufficient efficacy in the treatment of posttraumatic stress disorder (PTSD), a chronic and disabling condition.
Objective To test the efficacy and safety of a single intravenous subanesthetic dose of ketamine for the treatment of PTSD and associated depressive symptoms in patients with chronic PTSD.
Design, Setting, and Participants Proof-of-concept, randomized, double-blind, crossover trial comparing ketamine with an active placebo control, midazolam, conducted at a single site (Icahn School of Medicine at Mount Sinai, New York, New York). Forty-one patients with chronic PTSD related to a range of trauma exposures were recruited via advertisements.
Interventions Intravenous infusion of ketamine hydrochloride (0.5 mg/kg) and midazolam (0.045 mg/kg).
Main Outcomes and Measures The primary outcome measure was change in PTSD symptom severity, measured using the Impact of Event Scale–Revised. Secondary outcome measures included the Montgomery-Asberg Depression Rating Scale, the Clinical Global Impression–Severity and –Improvement scales, and adverse effect measures, including the Clinician-Administered Dissociative States Scale, the Brief Psychiatric Rating Scale, and the Young Mania Rating Scale.
Results Ketamine infusion was associated with significant and rapid reduction in PTSD symptom severity, compared with midazolam, when assessed 24 hours after infusion (mean difference in Impact of Event Scale–Revised score, 12.7 [95% CI, 2.5-22.8]; P = .02). Greater reduction of PTSD symptoms following treatment with ketamine was evident in both crossover and first-period analyses, and remained significant after adjusting for baseline and 24-hour depressive symptom severity. Ketamine was also associated with reduction in comorbid depressive symptoms and with improvement in overall clinical presentation. Ketamine was generally well tolerated without clinically significant persistent dissociative symptoms.

Conclusions and Relevance This study provides the first evidence for rapid reduction in symptom severity following ketamine infusion in patients with chronic PTSD. If replicated, these findings may lead to novel approaches to the pharmacologic treatment of patients with this disabling condition.
| Tags : ptsd
20/07/2015
Intervention médico-psychologique: Revue
Soutien médico-psychologique en situation de crise dans une unité : l'exemple de l’intervention suite au décès de trois militaires dans un accident de la voie publique
Moroge S. et Al. Médecine et Armées, 2014, 42, 2, 155-162
Le décès de trois militaires d'une base de défense du sud de la France, alors qu'ils rejoignaient un autre régiment avant d'être projetés au Mali dans le cadre de l'opération « Serval », a saisi la communauté militaire. La soudaineté de ces décès dans un accident de la voie publique, en métropole, à la veille d'un départ en opération extérieure, a été particulièrement marquante. Nous évoquerons ici l'intervention médico-psychologique afin de souligner les réactions psychiatriques observées. Nous détaillerons ensuite toutes les modalités d'intervention possibles suite à un évènement grave, afin d’éclairer le médecin d’unité sur la nature des soins post-immédiats à apporter aux militaires.
07/12/2014
Soutien psychologique durant les phases de déploiement : Guide du chef militaire
RTO-TR-HFM-081 - Stress and Psychological Support in Modern Military Operations
08/12/2013
PTSD et armée anglaise: Touchée comme tout le monde
PTSD in the armed forces: What have we learned from the recent cohort studies of Iraq/Afghanistan?
Goodwin L. et Al. Journal of Mental Health, 2013; 22(5): 397–401
L'armée anglaise semblait préservée du PTSD dans son expérience irakienne: Pas plus de PTSD que dans les troupes non déployées (1). Les explications semblaient se situer au niveau d'une organisation différente (taux d'encadrement, soldats plus âgés, et mission plus courtes). Les choses ont bien changées et actuellement nos alliées sont confrontés aux même problème que nous (2). Il est constaté un taux de PTSD double chez les réservistes engagés (3), par ailleurs ces troubles apparaissent plus tôt et chez des combattants plus jeunes que dans les conflits précédents (4) Le travail présenté fait le point de l'expérience actuelle en la matière des psychiatres militaires anglais
----------------------------------------------
In conclusion, the developments in military epidemiology have allowed cohort studies to confirm that combat experience is temporally related to PTSD. Yet, the majority of those who are deployed seem to be resilient. Across studies there are other common prospective vulnerability factors for PTSD, including psychiatric co-morbidity, alcohol misuse and lack of support. Whilst cross-sectional studies have found evidence to suggest that events outside of the military are important risks for PTSD, this needs to be investigated further in longitudinal research. Delayed-onset PTSD and other symptom trajectories which increase following deployment may be most important from a military perspective, but there is a need to further understand the reasons for the observed heterogeneity of PTSD trajectories.
----------------------------------------------
| Tags : ptsd
02/10/2013
Mental health following traumatic physical injury: An integrative literature review
Mental health following traumatic physical injury: An integrative literature review
Wiseman T et All. Injury, Int. J. Care Injured 44 (2013) 1383–1390
A B S T R A C T
Aim: To investigate the state of knowledge on the relationship between physical trauma and mental health in patients admitted to hospital with traumatic physical injury.
Background: Adults who sustain traumatic physical injury can experience a range of mental health problems related to the injury and subsequent changes in physical health and function. However earlyscreening and identification of mental health problems after traumatic physical injury is inconsistent and not routine during the hospital admission process for the physically injured patient.
Methods:
Integrative review methods were used. Data were sourced for the period 1995–2010 fromEMBASE, CINAHL, MEDLINE and PsycINFO and hand searching of key references. Abstracts were screened by 3 researchers against inclusion/exclusion criteria. Forty-one papers met the inclusion criteria. Data were retrieved, appraised for quality, analysed, and synthesised into 5 main categories.
Results: Forty-one primary research papers on the relationship between mental health and traumatic physical injury were reviewed. Studies showed that post-traumatic stress disorder, depression and anxiety were frequent sequelae associated with traumatic physical injury. However, these conditions were poorly identified and treated in the acute hospital phase despite their effect on physical health.
Conclusion: There is limited understanding of the experience of traumatic physical injury, particularly in relation to mental health. Greater translation of research findings to practice is needed in order to promote routine screening, early identification and referral to treatment for mental health problems in this patient group.
| Tags : psychiatrie, ptsd
13/09/2013
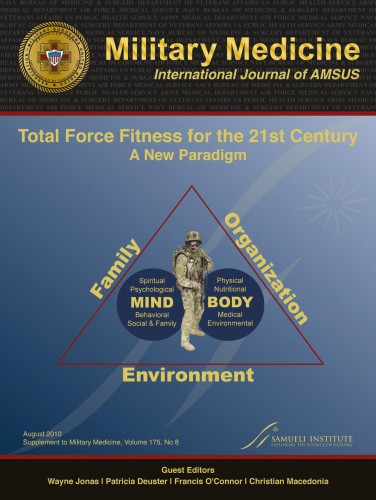
Physical fitness: Une nécessité ?
Psychological Health and Traumatic Brain Injury
04/09/2013
Prévention du suicide dans les armées
| Tags : psychiatrie, suicide
21/04/2013
Enjeux de la psychiatrie militaire en opération
| Tags : psychiatrie, ptsd
18/02/2013
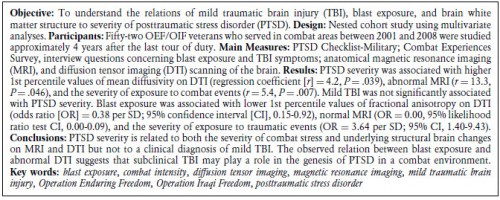
PTSD et Mild TBI: Convergence à l'IRM
The Relation Between Posttraumatic Stress Disorder and Mild Traumatic Brain Injury Acquired During Operations Enduring Freedom and Iraqi Freedom
| Tags : ptsd, psychiatrie
13/09/2012
Trauma crânien et psychologique: Le point US
| Tags : ptsd, tbi, psychiatrie
06/07/2012
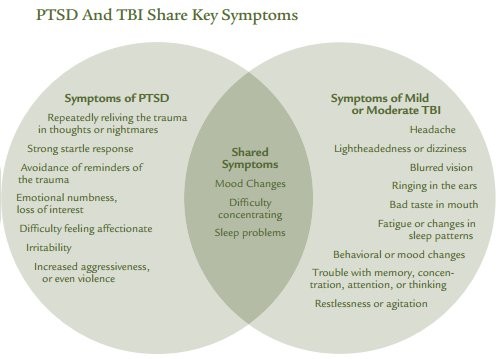
PTSD an TBI Share Hey Symptoms
Invisible Wounds Psychological and Neurological Injuries. Confront a New Generation of Veterans
| Tags : ptsd
28/04/2012
The injured mind in the UK Armed Forces
The mental health of the UK Armed Forces is a topic much debated by healthcare professionals, politicians and the media.While the current operations in Afghanistan, and the recent conflict in Iraq, are relevant to this debate, much of what is known about the effects of war upon the psyche still derives from the two World Wars. This paper will examine the historical and contemporary evidence about why it is that some Service personnel suffer psychological injuries during their military service and others do not. The paper will also consider some of the strategies that today’s Armed Forces have put in place to mitigate the effects of sending military personnel into danger.
http://rstb.royalsocietypublishing.org/content/366/1562/2...
| Tags : psychiatrie, ptsd
15/04/2012
Battle mind training: Le système
| Tags : ptsd, psychiatrie
Battle mind training: Bien comprendre
| Tags : ptsd, psychiatrie
Battlemind training: La famille aussi !
| Tags : ptsd, psychiatrie
Batlle mind training: Une fois rentré ?
| Tags : ptsd, psychiatrie