04/02/2026
Exsufflation: KT trop longs ? Attention à gauche
Meta-analysis of the optimal needle length and decompression site for tension pneumothorax and consensus recommendations on current ATLS and ETC guidelines
Ahmad SJS et Al. World J Emerg Surg. 2025 May 19;20(1):39
-------------------------
Un bémol sur l'emploi non discerné des cathéters actuellement proposés par l'industrie. Comme toujours primum non nocere
-------------------------
Background
Tension pneumothorax (TP) is a life-threatening condition. The immediate recommended management is needle decompression (ND), followed by the insertion of an intercostal chest drain. The European Trauma Course (ETC) and the Advanced Trauma Life Support (ATLS) guidelines differ on needle size and decompression site, creating clinical uncertainty. This meta-analysis aims to explore the optimal approach for emergency needle decompression in TP.
Methods
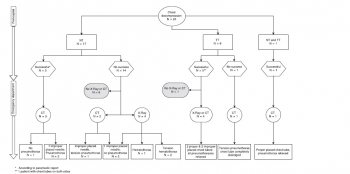
This meta-analysis followed the PRISMA 2020 guidelines. It included English-language RCTs, cohort, case–control, cross-sectional studies, and case series with more than six patients. Studies on adults undergoing needle decompression therapy for TP or with chest wall thickness measurements were included. Ovid MEDLINE, Embase, and Web of Science databases were searched until May 31, 2024. Data were extracted, assessed for quality using OCEBM and GRADE, and analyzed using SPSS and OpenMeta with random-effects models. Primary outcome: needle decompression failure rate. Secondary outcomes: patient demographics, cannula size, and chest wall thickness comparisons.
Results
This review analyzed 51 studies on needle decompression for TP, with a weighted mean patient age of 36.67 years. Radiological data from 24 studies (n = 8046) indicated a 32.84% failure rate for needle penetration into the pleural cavity (I2: 99.72%). Increased needle length reduced failure rates by 7.76% per cm. No significant differences in chest wall thickness between genders were observed (T-test, p = 0.77), but thickness at the 5th anterior axillary line (5AAL) and 5th midaxillary line (5MAL) was less than at the 2nd midclavicular line (2MCL). Injury rates were higher at 5AAL than 5MAL, with strong positive correlations between needle length and injury at these sites (0.88, 0.91).
Conclusion
Based on our meta-analysis, a 7 cm needle may be appropriate for decompression of right-sided tension pneumothorax at either the 5th intercostal space along the midaxillary line or the 2nd intercostal space along the midclavicular line. For left-sided cases, given the potential risk of cardiac injury, the 2nd midclavicular line is a safer option. However, these recommendations should be interpreted with caution due to considerable heterogeneity among the included studies, potential risk of bias, and variability in measurement techniques. Clinical decisions should always be individualized, taking into account patient-specific factors.
18/04/2023
Exsufflation: Attention , éviter le péricarde !
Risk of Harm in Needle Decompression for Tension Pneumothorax
Thompson P et Al. J Spec Oper Med. 2023 Apr 10;ZU1D-3DL9. doi: 10.55460/ZU1D-3DL9
-------------------------------------
Les recommendations américaines sont parfois un peu hâtives. C'est le cas de celles portant sur la longueur préconisée du cathéter d'exsufflation.
-------------------------------------
Comme quoi le "suivisme" évoqué récemment par un homme politique françias n'est pas toujours bon.
Introduction: Tension pneumothorax (TPX) is the third most common cause of preventable death in trauma. Needle decompression at the fifth intercostal space at anterior axillary line (5th ICS AAL) is recommended by Tactical Combat Casualty Care (TCCC) with an 83-mm needle catheter unit (NCU). We sought to determine the risk of cardiac injury at this site.
Methods: Institutional data sets from two trauma centers were queried for 200 patients with CT chest. Inclusion criteria include body mass index of =30 and age 18-40 years. Measurements were taken at 2nd ICS mid clavicular line (MCL), 5th ICS AAL and distance from the skin to pericardium at 5th ICS AAL. Groups were compared using Mann-Whitney U and chi-squared tests.
Results: The median age was 27 years with median BMI of 23.8 kg/m2. The cohort was 69.5% male. Mean chest wall thickness at 2nd ICS MCL was 38-mm (interquartile range (IQR) 32-45). At 5th ICS AAL, the median chest wall thickness was 30-mm (IQR 21-40) and the distance from skin to pericardium was 66-mm (IQR 54-79).
Conclusion: The distance from skin to pericardium for 75% of patients falls within the length of the recommended needle catheter unit (83-mm). The current TCCC recommendation to "hub" the 83mm needle catheter unit has potential risk of cardiac injury.
| Tags : exsufflation
16/01/2023
Poser un drain thoracique: Le Reactor ?
Comparing a Novel Hand-Held Device for Chest Tube Insertion to the Traditional Open Tube Thoracostomy for Simple Pneumothorax in a Porcine Model
Dilday J. et Al. J Spec Oper Med. 2022 Dec 16;22(4):41-45.
------------------------------------------------------------------
Ce genre de dispositif parait être plutôt adapté à des personnels peu habitué à ce geste et surtout nécessite un équipement supplémentaire
------------------------------------------------------------------
Background: Tube thoracostomy is the most effective treatment for pneumothorax, and on the battlefield, is lifesaving. In combat, far-forward adoption of open thoracostomy has not been successful. Therefore, the ability to safely and reliably perform chest tube insertion in the far-forward combat theatre would be of significant value. The Reactor is a hand-held device for tube thoracostomy that has been validated for tension pneumothorax compared to needle decompression. Here we investigate whether the Reactor has potential for simple pneumothorax compared to open thoracostomy. Treatment of pneumothorax before tension physiology ensues is critical.
Methods: Simple pneumothoraces were created in 5 in-vivo swine models and confirmed with x-ray. Interventions were randomized to open technique (OT, n = 25) and Reactor (RT, n = 25). Post-procedure radiography was used to confirm tube placement and pneumothorax resolution. Video Assisted Thoracoscopic Surgery (VATS) was used to evaluate for iatrogenic injuries. 50 chest tubes were placed, with 25 per group.
Results: There were no statistical differences between the groups for insertion time, pneumothorax resolution, or estimated blood loss (p = .91 and .83). Injury rates between groups varied, with 28% (n = 7) in the Reactor group and 8% (n = 2) the control group (p = .06). The most common injury was violation of visceral pleura (10%, n = 5, both groups) and violation of the mediastinum (8%, n = 4, both groups).
Conclusion: The Reactor device was equal compared to open thoracostomy for insertion time, pneumothorax resolution, and injury rates. The device required smaller incisions compared to tube thoracostomy and may be useful adjunct in simple pneumothorax management.
| Tags : pneumothorax
07/02/2022
QUICK CHEST TUBE KIT
18/01/2022
Echo Pleurale: ??
Not so FAST-Chest ultrasound underdiagnoses traumatic pneumothorax
Santorelli JE et Al.
J Trauma Acute Care Surg. 2022 Jan 1;92(1):44-48.
-----------------------------------------------------------
Le fait de ne rien voir à l'échographie ne signifie pas qu'il n'y a rien. Cette étude prend le contre-pied de l'outil miracle que l'échographie représente pour certains.
-----------------------------------------------------------
Background: Ultrasonography for trauma is a widely used tool in the initial evaluation of trauma patients with complete ultrasonography of trauma (CUST) demonstrating equivalence to computed tomography (CT) for detecting clinically significant abdominal hemorrhage. Initial reports demonstrated high sensitivity of CUST for the bedside diagnosis of pneumothorax. We hypothesized that the sensitivity of CUST would be greater than initial supine chest radiograph (CXR) for detecting pneumothorax.
Methods: A retrospective analysis of patients diagnosed with pneumothorax from 2018 through 2020 at a Level I trauma center was performed. Patients included had routine supine CXR and CUST performed prior to intervention as well as confirmatory CT imaging. All CUST were performed during the initial evaluation in the trauma bay by a registered sonographer. All imaging was evaluated by an attending radiologist. Subgroup analysis was performed after excluding occult pneumothorax. Immediate tube thoracostomy was defined as tube placement with confirmatory CXR within 8 hours of admission.
Results: There were 568 patients screened with a diagnosis of pneumothorax, identifying 362 patients with a confirmed pneumothorax in addition to CXR, CUST, and confirmatory CT imaging. The population was 83% male, had a mean age of 45 years, with 85% presenting due to blunt trauma. Sensitivity of CXR for detecting pneumothorax was 43%, while the sensitivity of CUST was 35%. After removal of occult pneumothorax (n = 171), CXR was 78% sensitive, while CUST was 65% sensitive (p < 0.01). In this subgroup, CUST had a false-negative rate of 36% (n = 62). Of those patients with a false-negative CUST, 50% (n = 31) underwent tube thoracostomy, with 85% requiring immediate placement.
Conclusion: Complete ultrasonography of trauma performed on initial trauma evaluation had lower sensitivity than CXR for identification of pneumothorax including clinically significant pneumothorax requiring tube thoracostomy. Using CUST as the primary imaging modality in the initial evaluation of chest trauma should be considered with caution.
14/11/2021
Décompression thoracique: 7 cm !
Prehospital Decompression of Pneumothorax: A Systematic Review of Recent Evidence
Robitaille-Fortin M et Al. Prehosp Disaster Med. 2021 Aug;36(4):450-459.
Introduction:
Pneumothorax remains an important cause of preventable trauma death. The aim of this systematic review is to synthesize the recent evidence on the efficacy, patient outcomes, and adverse events of different chest decompression approaches relevant to the out-of-hospital setting.
Methods:
A comprehensive literature search was performed using five databases (from January 1, 2014 through June 15, 2020). To be considered eligible, studies required to report original data on decompression of suspected or proven traumatic pneumothorax and be considered relevant to the prehospital context. They also required to be conducted mostly on an adult population (expected more than ≥80% of the population ≥16 years old) of patients. Needle chest decompression (NCD), finger thoracostomy (FT), and tube thoracostomy were considered. No meta-analysis was performed. Level of evidence was assigned using the Harbour and Miller system.
Results:
A total of 1,420 citations were obtained by the search strategy, of which 20 studies were included. Overall, the level of evidence was low. Eleven studies reported on the efficacy and patient outcomes following chest decompression. The most studied technique was NCD (n = 7), followed by FT (n = 5). Definitions of a successful chest decompression were heterogeneous. Subjective improvement following NCD ranged between 18% and 86% (n = 6). Successful FT was reported for between 9.7% and 32.0% of interventions following a traumatic cardiac arrest. Adverse events were infrequently reported. Nine studies presented only on anatomical measures with predicted failure and success. The mean anterior chest wall thickness (CWT) was larger than the lateral CWT in all studies except one. The predicted success rate of NCD ranged between 90% and 100% when using needle >7cm (n = 7) both for the lateral and anterior approaches. The reported risk of iatrogenic injuries was higher for the lateral approach, mostly on the left side because of the proximity with the heart.
Conclusions:
Based on observational studies with a low level of evidence, prehospital NCD should be performed using a needle >7cm length with either a lateral or anterior approach. While FT is an interesting diagnostic and therapeutic approach, evidence on the success rates and complications is limited. High-quality studies are required to determine the optimal chest decompression approach applicable in the out-of-hospital setting.
| Tags : décompression
29/11/2020
Pneumothorax: Votre doigt compte
08/10/2019
Exsufflation: 14G de 5 cm c'est bon
Needle Thoracostomy: Does Changing Needle Length and Location Change Patient Outcome?
BACKGROUND:
Needle thoracostomy (NT) is a common prehospital intervention for patients in extremis or cardiac arrest due to trauma. The purpose of this study is to compare outcomes, efficacy, and complications after a change in policy related to NT in a four-county Emergency Medical Services (EMS) system with a catchment area of greater than 1.6 million people.
METHODS:
This is a before and after observational study of all patients who had NT performed in the Central California (USA) EMS system. The before, anterior midclavicular line (MCL) group consisted of all patients who underwent NT from May 7, 2007 through February 28, 2013. The after, midaxillary line (MAL) axillary group consisted of all patients who underwent NT from March 1, 2013 through January 30, 2016, after policy revisions changed the timing, needle size, and placement location for NT. All prehospital and hospital records where NT was performed were queried for demographics, mechanism of injury, initial status and post-NT clinical change, reported complications, and final outcome. The trauma registry was accessed to obtain Injury Severity Scores (ISS). Information was manually abstracted by study investigators and examined utilizing univariate and multivariate analyses.
RESULTS:
Three-hundred and five trauma patients treated with NT were included in this study, of which, 169 patients (the MCL group) were treated with a 14-guage intravenous (IV) catheter at least 5.0-cm long at the second intercostal space (ICS), MCL after being placed in the ambulance; and 136 patients (the MAL group) were treated with a 10-guage IV catheter at least 9.5-cm long at the fifth ICS, MAL on scene. The mean ISS was lower in the MAL cohort (64.5 versus 69.2; P=.007). The mortality rate was 79% in both groups.
The multivariate model with regard to survival supported that a lower ISS (P<.001) and reported clinical change after NT (P=.003) were significant indicators of survival. No complications from NT were reported.
CONCLUSIONS:
Changing the timing, length of needle, and location of placement did not change mortality in patients requiring NT. Needle thoracostomy was used more frequently after the change in policy, and the MAL cohort was less injured. No increase in reported complications was noted.
| Tags : exsufflation
21/09/2019
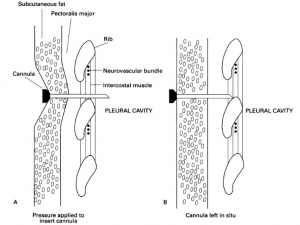
Exsufflation: Maintenir et pousser le cathéter
L'épaisseur de la paroi thoracique peut entraver l'exsufflation d'un pneumothorax compressif avec des cathéters de moins de 5 cm. Plusieurs publications se sont intéressées à cette problématique dont la connaissance n'est pourtant pas nouvelle. C'est ce qu'exprime l'image qui suit. Les auteurs donnaient un conseil de bon sens: Maintenez l'aiguille enfoncée dans le tissu sous-cutané pour pénétrer l'espace pleural. Dans l'observation présentée une fois cette pression interrompue, l'extrémité du cathéter ne se trouvant plus dans l'espace pleural, le geste devenait inéfficace avec pour corollaire une exsufflation incomplète.
Clic sur l'image pour accéder au document
17/07/2019
The pre-hospital management of life-threatening chest injuries: A consensus statement from the Faculty of Pre-Hospital Care
| Tags : thorax
16/07/2019
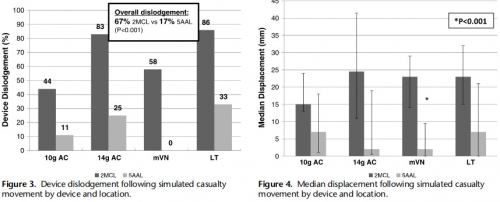
Exsuflation: Plus stable par voie axillaire
Relative device stability of anterior versus axillary needle decompression for tension pneumothorax during casualty movement: Preliminary analysis of a human cadaver model.
-------------------------------
L'étude porte sur la stabilité des cathéters d'exsufflation posés par voie antérieure versus par voie axillaire. Cette dernière voie est associée à un bien moindre risque de délogement pendant un transport que la voie antérieure. Ceci milite pour faire de la voie axillaire la voie de référence, et ce malgré la constatation de lésions parenchymateuses minimes.
-------------------------------
BACKGROUND:
Tension pneumothorax (tPTX) remains a significant cause of potentially preventable death in military and civilian settings. The current prehospital standard of care for tPTX is immediate decompression with a 14-gauge 8-cm angiocatheter; however, failure rates may be as high as 17% to 60%. Alternative devices, such as 10-gauge angiocatheter, modified Veress needle, and laparoscopic trocar, have shown to be potentially more effective in animal models; however, little is known about the relative insertional safety or mechanical stability during casualty movement.
METHODS:
Seven soft-embalmed cadavers were intubated and mechanically ventilated. Chest wall thickness was measured at the second intercostal space at the midclavicular line (2MCL) and the fifth intercostal space along the anterior axillary line (5AAL). CO2 insufflation created a PTX, and needle decompression was then performed with a randomized device. Insertional depth was measured between hub and skin before and after simulated casualty transport. Thoracoscopy was used to evaluate for intrapleural placement and/or injury during insertion and after movement. Cadaver demographics, device displacement, device dislodgment, and injuries were recorded. Three decompressions were performed at each site (2MCL/5AAL), totaling 12 events per cadaver.
RESULTS:
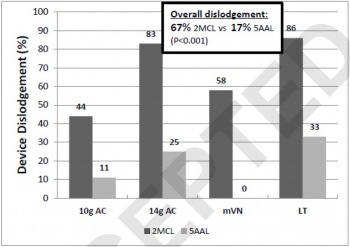
Eighty-four decompressions were performed. Average cadaver age was 59 years, and body mass index was 24 kg/m. The CWT varied between cadavers because of subcutaneous emphysema, but the average was 39 mm at the 2MCL and 31 mm at the 5AAL. Following movement, the 2MCL site was more likely to become dislodged than the 5AAL (67% vs. 17%, p = 0.001).
Median displacement also differed between 2MCL and 5AAL (23 vs. 2 mm, p = 0.001). No significant differences were noted in dislodgement or displacement between devices. Five minor lung injuries were noted at the 5AAL position.
CONCLUSION:
Preliminary results from this human cadaver study suggest the 5AAL position is a more stable and reliable location for thoracic decompression of tPTX during combat casualty transport.
| Tags : exsufflation
13/07/2019
Exsuffler au bon endroit: Avec un gabarit ?
ThoraSite: A device to improve accuracy of lateral decompression needle and chest tube placement.
BACKGROUND:
Multiple reports have detailed an unacceptably high error rate in the siting of decompression needles and tubes and describe associated iatrogenic injuries. The objective of the current study was to measure the accuracy of the novel ThoraSite template for identifying an acceptable intercostal space (ICS) for lateral needle or tube thoracostomy.
METHODS:
Two trained operators used the ThoraSite to place radiopaque needles in the left and right lateral chests of 12 cadavers. An independent radiologist reviewed fluoroscopy images to determine the primary outcome: the ICS in which each needle was placed. Secondary outcomes were ICS's palpable through ThoraSite's Safe Zone; needle placement relative to the anterior axillary line (AAL) and midaxillary line (MAL); and percent correct placement (defined as the third, fourth, or fifth ICS from 1 cm anterior to the AAL to 1 cm posterior to the MAL).
RESULTS:
The six female and six male cadavers spanned 4 ft and 11 inches (150 cm) to 6 ft and 7 inches (201 cm), 80 lb (36 kg) to 350 lb (159 kg), and 16 kg/m to 42 kg/m body mass index. All 24 needles were placed in either the third (4 [17%] of 24 needles), fourth (10 [42%] of 24 needles), or fifth ICS (10 [42%] of 24 needles). In 10 (42%) of 24 assessments, two ICSs were palpable in ThoraSite's Safe Zone. All palpable ICSs were either the third (8 [24%] of 34), fourth (15 [44%] of 34); or fifth ICS (11 [32%] of 34).
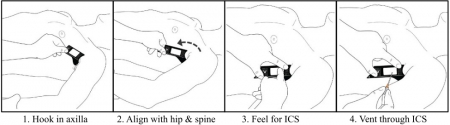
Twenty-three (96%) of 24 needles were inserted from 1 cm anterior to the AAL to 1 cm posterior to the MAL. Twenty-three (96%) of 24 needle placements were correct.
CONCLUSION:
ThoraSite use was associated with needle placement in the third, fourth, or fifth ICS in an area roughly spanning the AAL to MAL in anatomically diverse cadavers. By facilitating appropriate needle/tube placement, ThoraSite use may decrease iatrogenic injuries. Future study involving representative users may be useful to further evaluate ThoraSite accuracy.
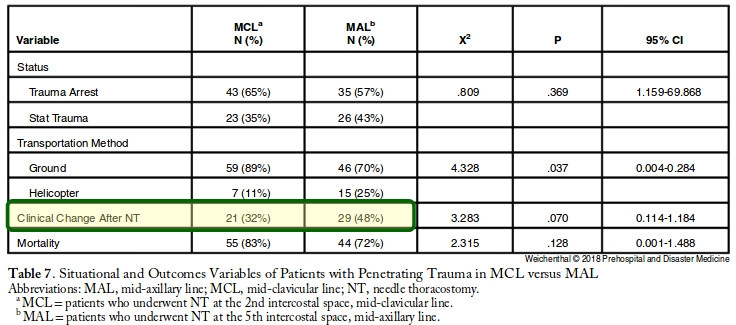
27/09/2018
Exsufflation: Gros et grand KT ? Pas sûr
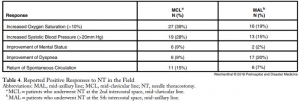
Needle Thoracostomy: Does Changing Needle Length and Location Change Patient Outcome?
Weichenthal, L. et Al. Prehospital and Disaster Medicine 2018, 33(3), 237-244.
Needle thoracostomy (NT) is a common prehospital intervention for patients in extremis or cardiac arrest due to trauma. The purpose of this study is to compare outcomes, efficacy, and complications after a change in policy related to NT in a four-county Emergency Medical Services (EMS) system with a catchment area of greater than 1.6 million people.
This is a before and after observational study of all patients who had NT performed in the Central California (USA) EMS system. The before, anterior midclavicular line (MCL) group consisted of all patients who underwent NT from May 7, 2007 through February 28, 2013. The after, midaxillary line (MAL) axillary group consisted of all patients who underwent NT from March 1, 2013 through January 30, 2016, after policy revisions changed the timing, needle size, and placement location for NT. All prehospital and hospital records where NT was performed were queried for demographics, mechanism of injury, initial status and post-NT clinical change, reported complications, and final outcome. The trauma registry was accessed to obtain Injury Severity Scores (ISS). Information was manually abstracted by study investigators and examined utilizing univariate and multivariate analyses.
Three-hundred and five trauma patients treated with NT were included in this study, of which, 169 patients (the MCL group) were treated with a 14-guage intravenous (IV) catheter at least 5.0-cm long at the second intercostal space (ICS), MCL after being placed in the ambulance; and 136 patients (the MAL group) were treated with a 10-guage IV catheter at least 9.5-cm long at the fifth ICS, MAL on scene.
The mean ISS was lower in the MAL cohort (64.5 versus 69.2; P=.007). The mortality rate was 79% in both groups. The multivariate model with regard to survival supported that a lower ISS (P<.001) and reported clinical change after NT (P=.003) were significant indicators of survival. No complications from NT were reported.
Changing the timing, length of needle, and location of placement did not change mortality in patients requiring NT. Needle thoracostomy was used more frequently after the change in policy, and the MAL cohort was less injured. No increase in reported complications was noted.
| Tags : exsufflation
10/06/2018
Exsufflation: 5 cm antérieur survie = 9 latéral
BACKGROUND:
Needle thoracostomy (NT) is a common prehospital intervention for patients in extremis or cardiac arrest due to trauma. The purpose of this study is to compare outcomes, efficacy, and complications after a change in policy related to NT in a four-county Emergency Medical Services (EMS) system with a catchment area of greater than 1.6 million people.
METHODS:
This is a before and after observational study of all patients who had NT performed in the Central California (USA) EMS system. The before, anterior midclavicular line (MCL) group consisted of all patients who underwent NT from May 7, 2007 through February 28, 2013. The after, midaxillary line (MAL) axillary group consisted of all patients who underwent NT from March 1, 2013 through January 30, 2016, after policy revisions changed the timing, needle size, and placement location for NT. All prehospital and hospital records where NT was performed were queried for demographics, mechanism of injury, initial status and post-NT clinical change, reported complications, and final outcome. The trauma registry was accessed to obtain Injury Severity Scores (ISS). Information was manually abstracted by study investigators and examined utilizing univariate and multivariate analyses.
RESULTS:
Three-hundred and five trauma patients treated with NT were included in this study, of which, 169 patients (the MCL group) were treated with a 14-gauge intravenous (IV) catheter at least 5.0-cm long at the second intercostal space (ICS), MCL after being placed in the ambulance; and 136 patients (the MAL group) were treated with a 10-gauge IV catheter at least 9.5-cm long at the fifth ICS, MAL on scene. The mean ISS was lower in the MAL cohort (64.5 versus 69.2; P=.007). The mortality rate was 79% in both groups.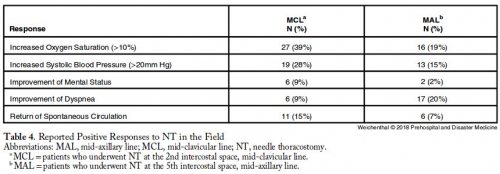
CONCLUSIONS:
Changing the timing, length of needle, and location of placement did not change mortality in patients requiring NT. Needle thoracostomy was used more frequently after the change in policy, and the MAL cohort was less injured. No increase in reported complications was noted.| Tags : exsufflation, pneumothorax
09/01/2018
A lire
Prolonged Field Care of a Casualty With Penetrating Chest Trauma Case Report
Barnhart G. et Al. J Spec Oper Med. Winter 2016;16(4):99-101
As Special Operations mission sets shift to regions with less coalition medical infrastructure, the need for quality long-term field care has increased. More and more, Special Operations Medics will be expected to maintain casualties in the field well past the "golden hour" with limited resources and other tactical limitations. This case report describes an extended-care scenario (>12 hours) of a casualty with a chest wound, from point of injury to eventual casualty evacuation and hand off at a Role II facility. This case demonstrates the importance of long-term tactical medical considerations and the effectiveness of minimal fluid resuscitation in treating penetrating thoracic trauma.
Histoire à lire
A Case of Prehospital Traumatic Arrest in a US Special Operations Soldier: Care From Point of Injury to Full Recovery
During an assault on an extremely remote target, a US Special Operations Soldier sustained multiple gunshot and fragmentation wounds to the thorax, resulting in a traumatic arrest and subsequent survival. His care, including care under fire, tactical field care, tactical evacuation care, and Role III, IV, and V care, is presented. The case is used to illustrate the complex dynamics of Special Operations care on the modern battlefield and the exceptional outcomes possible when evidence-based medicine is taken to the warfighter with effective,
01/10/2017
Exsufflation axillaire: Plus sûre
Relative device stability of anterior versus axillary needle decompression for tension pneumothorax during casualty movement: Preliminary analysis of a human cadaver model
BACKGROUND:
Tension pneumothorax (tPTX) remains a significant cause of potentially preventable death in military and civilian settings. The current prehospital standard of care for tPTX is immediate decompression with a 14-gauge 8-cm angiocatheter; however, failure rates may be as high as 17% to 60%. Alternative devices, such as 10-gauge angiocatheter, modified Veress needle, and laparoscopic trocar, have shown to be potentially more effective in animal models; however, little is known about the relative insertional safety or mechanical stability during casualty movement.
METHODS:
Seven soft-embalmed cadavers were intubated and mechanically ventilated. Chest wall thickness was measured at the second intercostal space at the midclavicular line (2MCL) and the fifth intercostal space along the anterior axillary line (5AAL). CO2 insufflation created a PTX, and needle decompression was then performed with a randomized device. Insertional depth was measured between hub and skin before and after simulated casualty transport. Thoracoscopy was used to evaluate for intrapleural placement and/or injury during insertion and after movement. Cadaver demographics, device displacement, device dislodgment, and injuries were recorded. Three decompressions were performed at each site (2MCL/5AAL), totaling 12 events per cadaver.
RESULTS:
Eighty-four decompressions were performed. Average cadaver age was 59 years, and body mass index was 24 kg/m. The CWT varied between cadavers because of subcutaneous emphysema, but the average was 39 mm at the 2MCL and 31 mm at the 5AAL. Following movement, the 2MCL site was more likely to become dislodged than the 5AAL (67% vs. 17%, p = 0.001). Median displacement also differed between 2MCL and 5AAL (23 vs. 2 mm, p = 0.001). No significant differences were noted in dislodgement or displacement between devices. Five minor lung injuries were noted at the 5AAL position.
CONCLUSION:
Preliminary results from this human cadaver study suggest the 5AAL position is a more stable and reliable location for thoracic decompression of tPTX during combat casualty transport.
| Tags : pneumothorax
22/04/2017
3 côtés: Non occlusif ? Pas tous égaux
Do vented chest seals differ in efficacy? An experimental evaluation using a swine hemopneumothorax model
--------------------------------
Un travail très pratique qui fait le point sur la performance des pansements 3 côtés non occlusifs. Plusieurs sont disponibles sur le marché. Mais qu'en est il des divers dispositifs proposés sur le marché. On dispose déjà de données concernant les propriétés "adhésives" de ces dispositifs (1). Avec ce travail, on a en plus une idée sur la capacité de ces pansements à permettre l'écoulement de saignement intra-thoraciques. L'historique valve d'asherman doit être considérée comme obsolète.
--------------------------------
OBJECTIVE:
Hemopneumothorax (HPTX) is the second leading cause of potentially preventable death among combat casualties. We investigated the ability of five FDA-approved non-occlusive chest seals (CSs) to seal a bleeding chest wound and prevent tension HPTX in a swine model.
METHODS:
Following instrumentation, an open chest wound was created in the left thorax of spontaneously air-breathing anesthetized pigs (n=26, 43 Kg). Autologous fresh blood (226 mL) was then infused into the pleural cavity to produce HPTX. The chest wounds were then sealed with CSs. The sealant strength and venting function of CSs were challenged by infusion of 50 mL more blood directly into the chest wound and incremental air injections into the pleural cavity. Tension HPTX was defined as intrapleural (IP) pressure ≥ +1 mmHg and >20% deviation in physiological measurements.
RESULTS:
An open chest wound with HPTX raised IP pressure (~ -0.7 mmHg) and caused labored breathing and reductions in PaO2 and SvO2 (P<0.01). Sealing the wounds with the CSs restored IP pressure, and improved breathing and oxygenation. Subsequent blood infusion into the wound and IP air injections produced CS-dependent responses.
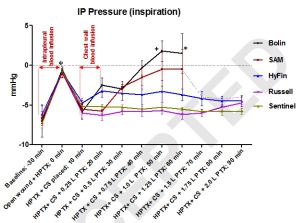
CSs with one-way valves (Bolin and SAM) did not evacuate the blood efficiently; pooled blood either detached the CSs from skin and leaked out (75%), or clotted and clogged the valve and led to tension HPTX (25%). Conversely, CSs with laminar venting channels allowed escape of blood and air from the pleural cavity and maintained IP pressure and oxygenation near normal levels. Success rates were 100% for Sentinel and Russell (6/6); 67% for HyFin (4/6); 25% for SAM (1/4); and 0% for Bolin (0/4) CSs (p=0.002).
CONCLUSION:
The sealant and valve function of vented CS differed widely in the presence of bleeding chest wounds. Medics should be equipped with more effective CSs for treating HPTX in the field.
| Tags : pneumothorax
18/01/2017
Décompression pleurale: Dur, dur...
Failure rate of prehospital chest decompression after severe thoracic trauma.
Kaserer A. et Al Am J Emerg Med. 2016 Nov 30. pii: S0735-6757(16)30892-0
-----------------------------------------------------
Une publication qui émane de nos collègues suisses et qui interpelle quelque peu. La décompression thoracique apparat être un geste dont la maîtrise est largement insuffisante y compris quand elle est réalisée au sein d'un système mature. Une raison de plus pour s'intéresser à la maîtrise effective des gestes censés participer à la mise en condition de survie des blessés. On rappelle l'intérêt de la thoracostomie au doigt (1), doigt dont la longueur est en général suffisante pour entrer dans un thorax.
-----------------------------------------------------
INTRODUCTION:
Chest decompression can be performed by different techniques, like needle thoracocentesis (NT), lateral thoracostomy (LT), or tube thoracostomy (TT). The aim of this study was to report the incidence of prehospital chest decompression and to analyse the effectiveness of these techniques.
MATERIAL AND METHODS:
In this retrospective case series study, all medical records of adult trauma patients undergoing prehospital chest decompression and admitted to the resuscitation area of a level-1 trauma center between 2009 and 2015 were reviewed and analysed. Only descriptive statistics were applied.
RESULTS:
In a 6-year period 24 of 2261 (1.1%) trauma patients had prehospital chest decompression. Seventeen patients had NT, six patients TT, one patient NT as well as TT, and no patients had LT. Prehospital successful release of a tension pneumothorax was reported by the paramedics in 83% (5/6) with TT, whereas NT was effective in 18% only (3/17). In five CT scans all thoracocentesis needles were either removed or extrapleural, one patient had a tension pneumothorax, and two patients had no pneumothorax. No NT or TT related complications were reported during hospitalization.
CONCLUSION:
Prehospital NT or TT is infrequently attempted in trauma patients. Especially NT is associated with a high failure rate of more than 80%, potentially due to an inadequate ratio between chest wall thickness and catheter length as previously published as well as a possible different pathophysiological cause of respiratory distress. Therefore, TT may be considered already in the prehospital setting to retain sufficient pleural decompression upon admission.
| Tags : pneumothorax
05/06/2016
Adhérence des pansements 3 côtés: Pas tous équivalents
Adherence Evaluation of Vented Chest Seals in a Swine Skin model
Arnaud F. et Al. Injury doi:10.1016/j.injury.2016.05.041
----------------------------------
L'adhérence cutanée est une caractéristique importante des pansements 3 côtés industriels. A l'évidence il existe des différences. C'est ce que démontre ce travail particulièrement intéressant car il napporte également quelques informations sur les effets de la température de stockage sur ces dispositifs. Une remarque: la peau est celle de cochons (lire aussi ce travail non publié)
----------------------------------
Objectives
Perforation of the chest (open pneumothorax) with and without lung injury can cause air accumulation in the chest, positive intrapleural pressure and lead to tension pneumothorax if untreated. The performance of chest seals to prevent tension physiology depends partially on their ability to adhere to the skin and seal the chest wound. Novel non-occlusive vented chest seals were assessed for their adhesiveness on skin of live swine under normal and extreme environmental conditions to simulate austere battlefield conditions.
Methods
Chest seals were applied on the back of the swine on skin that was soiled by various environmental contaminants to represent battlefield situations. A peeling (horizontal rim peeling) and detachment and breaching (vertical pulling) techniques were used to quantify the adhesive performance of vented chest seals. Among eight initially selected vented seals, five (Bolin, Russell, Fast breathe, Hyfin and SAM) were further down-selected based on their superior adherence scores at ambient temperatures. The adherence of these seals was then assessed after approximately 17 h storage at extreme cold (-19.5 °C) and hot (71.5 °C) temperatures.
Results
Adherence scores for peeling (above 90%) and detachment scores (less than 25%) were comparable for four vented chest seals when tested at ambient temperature, except for the Bolin seal which had higher breaching. Under extreme storage temperatures, adherence peeling scores were comparable to those at ambient temperatures for four chest seals.
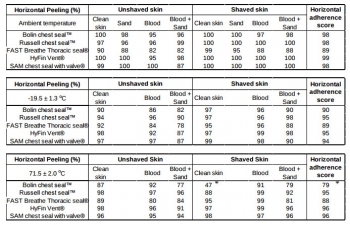
Scores were significantly lower for the Bolin seal at extreme temperatures. This seal also had the highest detachment and breaching scores. In contrast, the Russell, Fast breathe, Hyfin and SAM seals showed similar ability to stay air tight without breaching after hot storage.
Conclusion
No significant difference was found in skin adherence of the five vented chest seals at ambient temperature and the four seals (Russell, Fast breathe, Hyfin and SAM) maintained superior adherence even after exposure to extreme temperatures compared to the Bolin. To select the most effective product from the 5 selected vented chest seals, further functional evaluation of the valve of these chest seals on a chest wound with the potential for tension in the pneumothorax or hemopneumothorax is warranted.