16/02/2022
Triage en cas d'attaque terroriste: Des limites
Triage in Complex, Coordinated Terrorist Attacks
Pepper M et Al. Prehosp Disaster Med. 2019 Aug;34(4):442-448.
Introduction:
Terror attacks have increased in frequency, and tactics utilized have evolved. This creates significant challenges for first responders providing life-saving medical care in their immediate aftermath. The use of coordinated and multi-site attack modalities exacerbates these challenges. The use of triage is not well-validated in mass-casualty settings, and in the setting of intentional mass violence, new and innovative approaches are needed.
Methods:
Literature sourced from gray and peer-reviewed sources was used to perform a comparative analysis on the application of triage during the 2011 Oslo/Utoya Island (Norway), 2015 Paris (France), and 2015 San Bernardino (California USA) terrorist attacks. A thematic narrative identifies strengths and weaknesses of current triage systems in the setting of complex, coordinated terrorist attacks (CCTAs).
Discussion:
Triage systems were either not utilized, not available, or adapted and improvised to the tactical setting. The complexity of working with large numbers of patients, sensory deprived environments, high physiological stress, and dynamic threat profiles created significant barriers to the implementation of triage systems designed around flow charts, physiological variables, and the use of tags. Issues were identified around patient movement and "tactical triage."
Conclusion:
Current triage tools are inadequate for use in insecure environments, such as the response to CCTAs. Further research and validation are required for novel approaches that simplify tactical triage and support its effective application. Simple solutions exist in tactical triage, patient movement, and tag use, and should be considered as part of an overall triage system.
| Tags : triage
14/02/2022
IO: Attention Embolie graisseuse ?
Intraosseous fluid resuscitation causes systemic fat emboli in a porcine hemorrhagic shock model
Kristiansen S. et Al. Scand J Trauma Resusc Emerg Med . 2021 Dec 20;29(1):172.
Background: Intraosseous cannulation can be life-saving when intravenous access cannot be readily achieved. However, it has been shown that the procedure may cause fat emboli to the lungs and brain. Fat embolization may cause serious respiratory failure and fat embolism syndrome. We investigated whether intraosseous fluid resuscitation in pigs in hemorrhagic shock caused pulmonary or systemic embolization to the heart, brain, or kidneys and if this was enhanced by open chest conditions.
Methods: We induced hemorrhagic shock in anesthetized pigs followed by fluid-resuscitation through bilaterally placed tibial (hind leg) intraosseous cannulas. The fluid-resuscitation was limited to intraosseous or i.v. fluid therapy, and did not involve cardiopulmonary resuscitation or other interventions. A subgroup underwent median sternotomy with pericardiectomy and pleurotomy before hemorrhagic shock was induced. We used invasive hemodynamic and respiratory monitoring including Swan Ganz pulmonary artery catheter and transesophageal echocardiography and obtained biopsies from the lungs, heart, brain, and left kidney postmortem.
Results: All pigs exposed to intraosseous infusion had pulmonary fat emboli in postmortem biopsies. Additionally, seven of twenty-one pigs had coronary fat emboli. None of the pigs with open chest had fat emboli in postmortem lung, heart, or kidney biopsies. During intraosseous fluid-resuscitation, three pigs developed significant ST-elevations on ECG; all of these animals had coronary fat emboli on postmortem biopsies.
Conclusions: Systemic fat embolism occurred in the form of coronary fat emboli in a third of the animals who underwent intraosseous fluid resuscitation. Open chest conditions did not increase the incidence of systemic fat embolization.
| Tags : intraosseux
Kétamine: Stable longtemps quand il fait très chaud
Ketamine Stability over Six Months of Exposure to Moderate and High Temperature Environments
Foertsch MJ et Al. Prehosp Emerg Care. 2021 Jun 21;1-6.
Background:
All medications should be stored within temperature ranges defined by manufacturers, but logistical and operational challenges of prehospital and military settings complicate adherence to these recommendations. Lorazepam and succinylcholine experience clinically relevant heat-related degradation, whereas midazolam does not. Because ketamine's stability when stored outside manufacturer recommendations is unknown, we evaluated the heat-related degradation of ketamine exposed to several temperature ranges.
Methods: One hundred twenty vials of ketamine (50 mg/mL labeled concentration) from the same manufacturer lot were equally distributed and stored for six months in five environments: an active EMS unit in southwest Ohio (May-October 2019); heat chamber at constant 120 °F (C1); heat chamber fluctuating over 24 hours from 86 °F-120 °F (C2); heat chamber fluctuating over 24 hours from 40 °F-120 °F (C3); heat chamber kept at constant 70 °F (manufacturer recommended room temperature, C4). Four ketamine vials were removed every 30 days from each environment and sent to an FDA-accredited commercial lab for high performance liquid chromatography testing. Data loggers and thermistors allowed temperature recording every minute for all environments. Cumulative heat exposure was quantified by mean kinetic temperature (MKT), which accounts for additional heat-stress over time caused by temperature fluctuations and is a superior measure than simple ambient temperature. MKT was calculated for each environment at the time of ketamine removal. Descriptive statistics were used to describe the concentration changes at each time point.
Results: The MKT ranged from 73.6 °F-80.7 °F in the active EMS unit and stayed constant for each chamber (C1 MKT: 120 °F, C2 MKT: 107.3 °F, C3 MKT: 96.5 °F, C4 MKT: 70 °F). No significant absolute ketamine degradation, or trends in degradation, occurred in any environment at any time point. The lowest median concentration occurred in the EMS-stored samples removed after 6 months [48.2 mg/mL (47.75, 48.35)], or 96.4% relative strength to labeled concentration.
Conclusion: Ketamine samples exhibited limited degradation after 6 months of exposure to real world and simulated extreme high temperature environments exceeding manufacturer recommendations. Future studies are necessary to evaluate ketamine stability beyond 6 months.
| Tags : kétamine
09/02/2022
Efficacité et sécurité de la kétamine pour l'analgésie préhospitalière du blessé de guerre
07/02/2022
Catalogue ADS
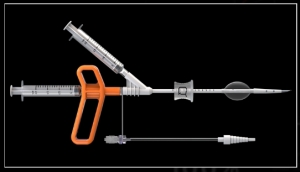
QUICK CHEST TUBE KIT