30/09/2018
US: Mieux que la main pour la conio
A multicentre prospective cohort study of the accuracy of conventional landmark technique for cricoid localisation using ultrasound scanning
Cricoid pressure is employed during rapid sequence induction to reduce the risk of pulmonary aspiration. Correct application of cricoid pressure depends on knowledge of neck anatomy and precise identification of surface landmarks. Inaccurate localisation of the cricoid cartilage during rapid sequence induction risks incomplete oesophageal occlusion, with potential for pulmonary aspiration of gastric contents. It may also compromise the laryngeal view for the anaesthetist. Accurate localisation of the cricoid cartilage therefore has relevance for the safe conduct of rapid sequence induction.
We conducted a multicentre, prospective cohort study to determine the accuracy of cricoid cartilage identification in 100 patients. The cranio‐caudal midpoint of the cricoid cartilage was identified by a qualified anaesthetic assistant using the conventional landmark technique and marked. While maintaining the patient in the same position, a second mark was made by identifying the midpoint of the cricoid cartilage using ultrasound scanning.
The mean (SD) distance between the two marks was 2.07 (8.49) mm. In 41% of patients the midpoint was incorrectly identified by a margin greater than 5 mm. This error was uniformly distributed both above and below the midpoint of the cricoid cartilage. The Pearson correlation coefficient of this error with respect to body mass index was 0.062 (p = 0.539) and with age was −0.020 (p = 0.843). There were also no significant differences in error between male and female patients.
Identification of cricoid position using a landmark technique has a high degree of variability and has little correlation with age, sex or body mass index. These findings have significant implications for the safe application of cricoid pressure in the context of rapid sequence induction.
| Tags : airway, coniotomie
27/09/2018
Exsufflation: Gros et grand KT ? Pas sûr
Needle Thoracostomy: Does Changing Needle Length and Location Change Patient Outcome?
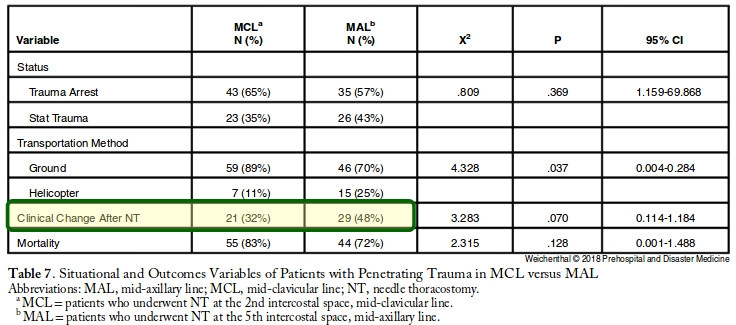
Weichenthal, L. et Al. Prehospital and Disaster Medicine 2018, 33(3), 237-244.
Needle thoracostomy (NT) is a common prehospital intervention for patients in extremis or cardiac arrest due to trauma. The purpose of this study is to compare outcomes, efficacy, and complications after a change in policy related to NT in a four-county Emergency Medical Services (EMS) system with a catchment area of greater than 1.6 million people.
This is a before and after observational study of all patients who had NT performed in the Central California (USA) EMS system. The before, anterior midclavicular line (MCL) group consisted of all patients who underwent NT from May 7, 2007 through February 28, 2013. The after, midaxillary line (MAL) axillary group consisted of all patients who underwent NT from March 1, 2013 through January 30, 2016, after policy revisions changed the timing, needle size, and placement location for NT. All prehospital and hospital records where NT was performed were queried for demographics, mechanism of injury, initial status and post-NT clinical change, reported complications, and final outcome. The trauma registry was accessed to obtain Injury Severity Scores (ISS). Information was manually abstracted by study investigators and examined utilizing univariate and multivariate analyses.
Three-hundred and five trauma patients treated with NT were included in this study, of which, 169 patients (the MCL group) were treated with a 14-guage intravenous (IV) catheter at least 5.0-cm long at the second intercostal space (ICS), MCL after being placed in the ambulance; and 136 patients (the MAL group) were treated with a 10-guage IV catheter at least 9.5-cm long at the fifth ICS, MAL on scene.
The mean ISS was lower in the MAL cohort (64.5 versus 69.2; P=.007). The mortality rate was 79% in both groups. The multivariate model with regard to survival supported that a lower ISS (P<.001) and reported clinical change after NT (P=.003) were significant indicators of survival. No complications from NT were reported.
Changing the timing, length of needle, and location of placement did not change mortality in patients requiring NT. Needle thoracostomy was used more frequently after the change in policy, and the MAL cohort was less injured. No increase in reported complications was noted.
| Tags : exsufflation
25/09/2018
Intervenir sur une tuerie massive: Un savoir faire à acquérir
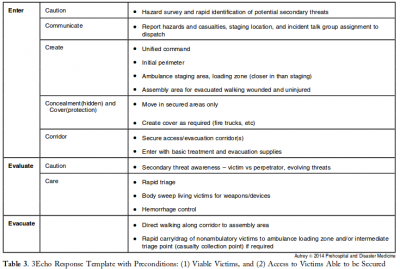
This report describes the successful use of a simple 3-phase approach that guides the initial 30 minutes of a response to blast and active shooter events with casualties: Enter, Evaluate, and Evacuate (3 Echo) in a mass-shooting event occurring in Minneapolis, Minnesota USA, on September 27, 2012. Early coordination between law enforcement (LE) and rescue was emphasized, including establishment of unified command, a common operating picture, determination of evacuation corridors, swift victim evaluation, basic treatment, and rapid evacuation utilizing an approach developed collaboratively over the four years prior to the event. Field implementation of 3 Echo requires multi-disciplinary (Emergency Medical Services (EMS), fire and LE) training to optimize performance.
This report details the mass-shooting event, the framework created to support the response, and also describes important aspects of the concepts of operation and curriculum evolved through years of collaboration between multiple disciplines to arrive at unprecedented EMS transport times in response to the event.
23/09/2018
ISR par des non médecins: Oui possible
Prehospital Rapid Sequence Intubation by Intensive Care Flight Paramedics.
OBJECTIVE:
Rapid sequence intubation (RSI) is an advanced airway procedure for critically ill or injured patients. Paramedic-performed RSI in the prehospital setting remains controversial, as unsuccessful or poorly conducted RSI is known to result in significant complications. In Victoria, intensive care flight paramedics (ICFPs) have a broad scope of practice including RSI in both the adult and pediatric population. We sought to describe the success rates and characteristics of patients undergoing RSI by ICFPs in Victoria, Australia.
METHODS:
A retrospective data review was conducted of adult (≥ 16 years) patients who underwent RSI by an ICFP between January 1, 2011, and December 31, 2016. Data were sourced from the Ambulance Victoria data warehouse.
RESULTS:
A total of 795 cases were included in analyses, with a mean age of 45 (standard deviation = 19.6) years. The majority of cases involved trauma (71.7%), and most patients were male (70.1%). Neurological pathologies were the most common clinical indication for RSI (68.3%). The first pass success rate of intubation was 89.4%, and the overall success rate was 99.4%. Of the 5 failed intubations (0.6%), all patients were safely returned to spontaneous respiration. Two patients were returned via bag/valve/mask (BVM) support alone, two with BVM and oropharyngeal airway, and one via supraglottic airway. No surgical airways were required. Overall, we observed transient cases of hypotension (5.2%), hypoxemia (1.3%), or both (0.1%) in 6.6% of cases during the RSI procedure.
CONCLUSION:
A very high RSI procedural success rate was observed across the study period. This supports the growing recognition that appropriately trained paramedics can perform RSI safely in the prehospital environment.
| Tags : airway
22/09/2018
Echo pour l'intubation
Integration of Point-of-care Ultrasound during Rapid Sequence Intubation in Trauma Resuscitation.
Introduction:
Airway and breathing management play critical role in trauma resuscitation. Early identification of esophageal intubation and detection of fatal events is critical. Authors studied the utility of integration of point-of-care ultrasound (POCUS) during different phases of rapid sequence intubation (RSI) in trauma resuscitation.
Methods:
It was prospective, randomized single-centered study conducted at the Emergency Department of a level one trauma center. Patients were divided into ultrasonography (USG) and clinical examination (CE) arm. The objectives were to study the utility of POCUS in endotracheal tube placement and confirmations and identification of potentially fatal conditions as tracheal injury, midline vessels, paratracheal hematoma, vocal cord pathology, pneumothorax, and others during RSI. Patient >1 year of age were included. Time taken for procedure, number of incorrect intubations, and pathologies detected were noted. The data were collected in Microsoft Excel spread sheets and analyzed using Stata (version 11.2, Stata Corp, Texas, U. S. A) software.
Results:
One hundred and six patients were recruited. The mean time for primary survey USG versus CE arm was (20 ± 10.01 vs. 18 ± 11.03) seconds. USG detected four pneumothorax, one tracheal injury, and one paratracheal hematoma. The mean procedure time USG versus CE arm was (37.3 ± 21.92 vs. 58 ± 32.04) seconds. Eight esophageal intubations were identified in USG arm by POCUS and two in CE arm by EtCO2 values.
Conclusion:
Integration of POCUS was useful in all three phases of RSI. It identified paratracheal hematoma, tracheal injury, and pneumothorax. It also identified esophageal intubation and confirmed main stem tracheal intubation in less time compared to five-point auscultation and capnography.
| Tags : airway
21/09/2018
Coniotomie: Control-Cric pas optimal
A Randomized Comparative Assessment of Three Surgical Cricothyrotomy Devices on Airway Mannequins.
Dorsam J et Al. Prehosp Emerg Care. 2018 Sep 1:1-30
-------------
La réalisation d'une coniotomie peut se faire par voie percutanée avec mandrin souple ou chirurgical, aidée ou pas d'une bougie. L'armée américaine recommande dans sa dernière révision du TCCC le recours à un dispositif appelé control-kit. Les données sur lesquelles reposent une telle proposition sont minces. Ce travail n'est clairement pas en sa faveur, du moins sur le modèle de moulage utilisé pour l'étude. La référence reste donc la technique chirurgicale.
-------------
BACKGROUND:
Airway obstruction is the second leading cause of preventable battlefield death, at least in part because surgical cricothyrotomy (SC) failure rates remain unacceptably high. Ideally, SC should be a rapid, simple, easily-learned, and reliably-performed procedure. Currently, Tactical Combat Casualty Care (TCCC) has approved three SC devices: The Tactical CricKit® (TCK), Control-Cric™(CC), and Bougie-assisted Technique (BAT). However, no previous studies have compared these devices in application time, application success, user ratings, and user preference.
METHODS:
United States Navy Corpsmen (N = 25) were provided 15 minutes of standardized instruction, followed by hands-on practice with each device on airway mannequins. Participants then performed SC with each of the three devices in a randomly assigned sequence. In this within-subjects design, application time, application success, participant ratings, and participant preference data were analyzed using repeated-measures ANOVA, regression, and non-parametric statistics at p < 0.05.
RESULTS:
Application time for CC (M = 184 sec, 95% CI 144-225 sec) was significantly slower than for BAT (M = 135 sec, 95% CI 113-158 sec, p < 0.03) and TCK (M = 117 sec, 95% CI 93-142 sec, p < 0.005). Success was significantly greater for BAT (76%) than for TCK (40%, p < 0.02) and trended greater than CC (48%, p = 0.07).
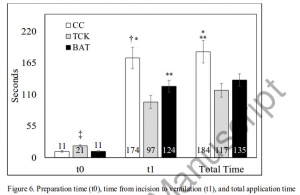
CC was rated significantly lower than TCK and BAT in ease of application, effectiveness, and reliability (each p < 0.01). User preference was significantly (p < 0.01) higher for TCK (58%) and BAT (42%) than for CC (0%). Improved CC blade design was the most common user suggestion.
CONCLUSION:
While this study was limited by the use of mannequins in a laboratory environment, present results indicate that none of these devices was ideal for performing SC. Based on slow application times, low success rates, and user feedback, the Control-Cric™ cannot be recommended until improvements are made to the blade design.
| Tags : airway
Airway Ultrasound
| Tags : airway
16/09/2018
Airway, pour être au RDV: S'entraîner
A Continuous Quality Improvement Airway Program Results in Sustained Increases in Intubation Success.
INTRODUCTION:
Airway management is a critical skill for air medical providers, including the use of rapid sequence intubation (RSI) medications. Mediocre success rates and a high incidence of complications has challenged air medical providers to improve training and performance improvement efforts to improve clinical performance.
OBJECTIVES:
The aim of this research was to describe the experience with a novel, integrated advanced airway management program across a large air medical company and explore the impact of the program on improvement in RSI success.
METHODS:
The Helicopter Advanced Resuscitation Training (HeART) program was implemented across 160 bases in 2015. The HeART program includes a novel conceptual framework based on thorough understanding of physiology, critical thinking using a novel algorithm, difficult airway predictive tools, training in the optimal use of specific airway techniques and devices, and integrated performance improvement efforts to address opportunities for improvement. The C-MAC video/direct laryngoscope and high-fidelity human patient simulation laboratories were implemented during the study period. Chi-square test for trend was used to evaluate for improvements in airway management and RSI success (overall intubation success, first-attempt success, first-attempt success without desaturation) over the 25-month study period following HeART implementation.
RESULTS:
A total of 5,132 patients underwent RSI during the study period. Improvements in first-attempt intubation success (85% to 95%, p < 0.01) and first-attempt success without desaturation (84% to 94%, p < 0.01) were observed. Overall intubation success increased from 95% to 99% over the study period, but the trend was not statistically significant (p = 0.311).
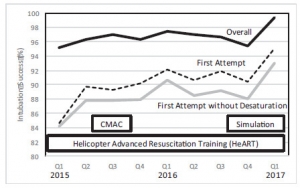
CONCLUSIONS:
An integrated advanced airway management program was successful in improving RSI intubation performance in a large air medical company.
| Tags : airway
15/09/2018
Aggressions collectives par arme de guerre
Coniotomie: Ne pas endommager le mandrin
Front-of-neck access and bougie trapping

| Tags : airway, coniotomie
10/09/2018
Settings standard for CCC
08/09/2018
Le TCCC dans la vraie vie
Survey of Casualty Evacuation Missions Conducted by the 160th Special Operations Aviation Regiment During the Afghanistan Conflict.
BACKGROUND:
Historically, documentation of prehospital combat casualty care has been relatively nonexistent. Without documentation, performance improvement of prehospital care and evacuation through data collection, consolidation, and scientific analyses cannot be adequately accomplished. During recent conflicts, prehospital documentation has received increased attention for point-of-injury care as well as for care provided en route on medical evacuation platforms. However, documentation on casualty evacuation (CASEVAC) platforms is still lacking. Thus, a CASEVAC dataset was developed and maintained by the 160th Special Operations Aviation Regiment (SOAR), a nonmedical, rotary-wing aviation unit, to evaluate and review CASEVAC missions conducted by their organization.
METHODS:
A retrospective review and descriptive analysis were performed on data from all documented CASEVAC missions conducted in Afghanistan by the 160th SOAR from January 2008 to May 2015. Documentation of care was originally performed in a narrative after-action review (AAR) format. Unclassified, nonpersonally identifiable data were extracted and transferred from these AARs into a database for detailed analysis. Data points included demographics, flight time, provider number and type, injury and outcome details, and medical interventions provided by ground forces and CASEVAC personnel.
RESULTS:
There were 227 patients transported during 129 CASEVAC missions conducted by the 160th SOAR. Three patients had unavailable data, four had unknown injuries or illnesses, and eight were military working dogs. Remaining were 207 trauma casualties (96%) and five medical patients (2%). The mean and median times of flight from the injury scene to hospital arrival were less than 20 minutes. Of trauma casualties, most were male US and coalition forces (n = 178; 86%). From this population, injuries to the extremities (n = 139; 67%) were seen most commonly. The primary mechanisms of injury were gunshot wound (n = 89; 43%) and blast injury (n = 82; 40%). The survival rate was 85% (n = 176) for those who incurred trauma. Of those who did not survive, most died before reaching surgical care (26 of 31; 84%).
CONCLUSION:
Performance improvement efforts directed toward prehospital combat casualty care can ameliorate survival on the battlefield. Because documentation of care is essential for conducting performance improvement, medical and nonmedical units must dedicate time and efforts accordingly. Capturing and analyzing data from combat missions can help refine tactics, techniques, and procedures and more accurately define wartime personnel, training, and equipment requirements. This study is an example of how performance improvement can be initiated by a nonmedical unit conducting CASEVAC missions.
Guy Charmot.

Guy Charmot est né le 9 octobre 1914 à Toulon dans une famille de fonctionnaires.
Ressentant très jeune la vocation coloniale, il entre en 1934 à l'Ecole du service de Santé militaire à Lyon. En 1939, il se trouve médecin-lieutenant d'active au 49e Régiment d'artillerie coloniale (49e RAC) dans le secteur de la Sarre.
Embarqué en mars 1940 pour la Haute-Volta, il passe en Gold Coast (Ghana) au début de juillet 1940 puis au Cameroun où il rallie les Forces françaises libres en septembre.
Affecté comme médecin au Bataillon de Marche n°4 (BM 4) dès sa formation, il part avec lui du Cameroun en décembre 1940 pour rejoindre en Palestine la 1ère Brigade Coloniale du lieutenant-colonel Génin.
Guy Charmot prend part à la campagne de Syrie en juin 1941 avec le BM 4 qui combat ensuite en Ethiopie avant de stationner au Liban pendant l'année 1942.
En janvier 1943, le Bataillon rejoint en Libye les rangs de la 2e Brigade Française Libre de la 1ère Division Française Libre.
Guy Charmot participe aux combats de Tunisie, faisant toujours preuve de beaucoup d'activité, de courage et de dévouement.
Guy Charmot se distingue particulièrement au cours des combats des 17 au 20 mai 1944 en Italie, poussant au plus loin ses postes de secours et sauvant ainsi plusieurs de ses camarades de combat par la rapidité de ses interventions sur la ligne de feu. Il reçoit la croix de la Libération des mains du général de Gaulle le 30 juin 1944 à Marcianise.
Il débarque en Provence avec la 1ère Division Française Libre en août 1944 et est blessé lors des combats pour la libération de Toulon.
Il prend part ensuite à la campagne de France jusqu'en 1945 terminant la guerre au massif de l’Authion dans les Alpes-Maritimes.
Médecin-capitaine à la fin de la guerre, il devient médecin des Hôpitaux d'Outre-mer et professeur agrégé du Service de Santé des Armées, effectuant de nombreux séjours en Afrique jusqu'en 1965. Spécialiste de la recherche en médecine tropicale, Guy Charmot démissionne avec le grade de médecin-colonel pour entrer au service de Recherches thérapeutiques de Rhône-Poulenc.
Professeur à l'Institut de médecine et d'épidémiologie africaine, il participe en outre à la rédaction de plusieurs ouvrages médicaux en collaboration et à 300 publications scientifiques. Ancien président de la Société de Pathologie exotique, il est élu, en 1994, membre de l'Académie des Sciences d'Outremer.
• Grand Officier de la Légion d'Honneur
• Compagnon de la Libération - décret du 20 novembre 1944
• Croix de Guerre 39/45 (4 citations)
• Chevalier des Palmes Académiques
• Chevalier de la Santé Publique
• Médaille Coloniale avec agrafe « Somalis »
• Médaille Commémorative 39/45
• Médaille Commémorative de la Campagne d'Italie
• Officier de l'Etoile Noire (Bénin)
| Tags : personnalité