09/10/2024
Tourniquet en milieu froid: Des spécificités
Analysis of tourniquet pressure over military winter clothing and a short review of combat casualty care in cold weather warfare
Cold weather warfare is of increasing importance. Haemorrhage is the most common preventable cause of death in military conflicts. We analysed the pressure of the Combat Application Tourniquet® Generation 7 (CAT), the SAM® Extremity Tourniquet (SAMXT) and the SOF® Tactical Tourniquet Wide Generation 4 (SOFTT) over different military cold weather clothing setups with aleg tourniquet trainer. We conducted a selective PubMed search and supplemented this with own experiences in cold weather medicine. The CAT and the SAMXT both reached the cut off value of 180 mmHg in almost all applications. The SOFTT was unable to reach the 180 mmHg limit in less than 50% of all applications in some clothing setups. We outline the influence of cold during military operations by presenting differences between military and civilian cold exposure. We propose a classification of winter warfare and identify caveats and alterations of Tactical CombatCasualty Care in cold weather warfare, with a special focus on control of bleeding. The application of tourniquets over military winter clothing is successful in principle, but effectiveness may vary for different tourniquet models. Soldiers are more affected and impaired by cold than civilians. Militaryc ommanders must be made aware of medical alterations in cold weather warfare.
30/09/2024
En Ukraine ?
Lessons learned from the war in Ukraine for the anesthesiologist and intensivist: A scoping review
Jarrassier A. et Al Anaesth Crit Care Pain Med. 2024 Jul 30;43(5):101409.
--------------------------
Un point de situation particulièrement intéressant qui met en avant la nécessité de prendre en compte les spécificités de cette guerre à haute intensité: De nouvelles modalités lésionnelles notamment par les armes thermo-bariques, les difficultés de l'établissement d'une chaîne maîtrisée de prise en charge des blessés avec la réapparition du train comme vecteur d'évacuation, bien souvent la nécessité de porter la chirurgie au plus près des combats en s'appuyant sur les hôpitaux d'infrastructures, la difficulté de l'approvisionnement notamment en dérivés sanguins, la réapparition de la discussion sur le garrot, la nécessité de disposer d'équipes parfaitement formées et entraînées pour intervenir dans de telles conditions, la place tout à fait particulière et prééminente des anesthésistes-réanimateurs dans de telles situations.
Une bonne partie de ces constatations avaient été faites notamment lors de la crise COVID (histoire de l'EMR SSA de Mulhouse puis dans les DOM). Oui mais elles ont été oubliées noyées dans le quotidien.
Background
The war in Ukraine provides purposefully anesthesiologists and intensivists with important data for improving the management of trauma patients. This scoping review aims to investigate the specific management of war-related trauma patients, during the war in Ukraine, through an objective and comprehensive analysis.
Methods
A comprehensive search of the Embase, Medline, and Open Grey databases from 2014 to February 2024 yielded studies focusing on anesthesia and surgery. These studies were assessed by PRISMA and STROBE criteria and needed to discuss anesthesiology and surgical procedures.
Results
Of the 519 studies identified, 21 were included, with a low overall level of evidence. The studies covered 11,622 patients and 2470 surgical procedures. Most patients were Ukrainian men, 25–63 years old, who had sustained severe injuries from high-energy weapons, such as multiple rocket systems and combat drones. These injuries included major abdominal, facial, and extremity traumas. The surgical procedures varied from initial debridement to complex reconstructions. Anesthesia management faced significant challenges, including resource scarcity and the need for quick adaptability. Evacuations of casualties were lengthy, complex, and often involved rail transportation. Hemorrhage control with tourniquets was critical but associated with many complications. The very frequent presence of multi-resistant organisms required dedicated preventive measures and appropriated treatments. The need for qualified human resources underscored the importance of civilian-military cooperation.
Conclusion
This scoping review provides original and relevant insights on the lessons learned from the ongoing war in Ukraine, which could be useful for anesthesiologists and intensivists.
02/04/2024
Les gestes US du Role 1 chez les américains
An Analysis of 13 Years of Prehospital Combat Casualty Care: Implications for Maintaining a Ready Medical Force
Schauer SG et Al. Prehosp Emerg Care. 2022 May-Jun;26(3):370-379.
----------------------------------
Des choses simples dans un contexte où les medevac étaient très rapides, ce qui n'est plus le cas. Poser des garrots est toujours nécessaires MAIS ne suffit plus. Les gestes sophistiqués de réanimation doivent absolument être maîtrisées. Cela passe par une autre vision, que celle actuelle, de la médicalisation de l'avant.
----------------------------------
Background:
Most potentially preventable deaths occur in the prehospital setting before reaching a military treatment facility with surgical capabilities. Thus, optimizing the care we deliver in the prehospital combat setting represents a ripe target for reducing mortality. We sought to analyze prehospital data within the Department of Defense Trauma Registry (DODTR).
Materials and methods:
We requested all encounters with any prehospital activity (e.g., interventions, transportation, vital signs) documented within the DODTR from January 2007 to March 2020 along with all hospital-based data that was available. We excluded from our search casualties that had no prehospital activity documented.
Results:
There were 28,950 encounters that met inclusion criteria. Of these, 25,897 (89.5%) were adults and 3053 were children (10.5%). There was a steady decline in the number of casualties encountered with the most notable decline occurring in 2014. U.S. military casualties comprised the largest proportion (n = 10,182) of subjects followed by host nation civilians (n = 9637). The median age was 24 years (interquartile range/IQR 21-29).
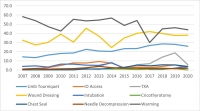
Most were battle injuries (78.6%) and part of Operation ENDURING FREEDOM (61.8%) and Operation IRAQI FREEDOM (24.4%). Most sustained injuries from explosives (52.1%) followed by firearms (28.1%), with serious injury to the extremities (24.9%) occurring most frequently. The median injury severity score was 9 (IQR 4-16) with most surviving to discharge (95.0%). A minority had a documented medic or combat lifesaver (27.9%) in their chain of care, nor did they pass through an aid station (3.0%). Air evacuation predominated (77.9%).
Conclusions:
Within our dataset, the deployed U.S. military medical system provided prehospital medical care to at least 28,950 combat casualties consisting mostly of U.S. military personnel and host nation civilian care. There was a rapid decline in combat casualty volumes since 2014, however, on a per-encounter basis there was no apparent drop in procedural volume.
16/09/2022
La chirurgie: Encore plus à l'avant
Treatment at Point of Injury. Forward movement of surgical assets to address non compressible truncal haemorrhage
Pilgrim CHC et Al. JMVH 2022, 30: 41-50.
-----------------------------------------------------
C'est la chirurgie qui va sauver les blessés du tronc. Encore faut il que ces blessés soient pris en charge par une équipe chirurgicale. D'où le principe de constituer de petites équipes chirurgicales mettant en oeuvre des techniques choisies et limitées dans un environnement très austère au plus près des combats. C'est le principe du module de chirurgie vitale. Les combats actuels (haute intensité mais avec des effectifs plutôt limités) prônent pour le développement de cette stratégie. Le document présenté est une réflexion australienne en la matière.
-----------------------------------------------------
Contemporary battlefield trauma surgery in the Middle East Region has been characterised by aeromedical evacuation by rotatory wing (RWAME) with relative impunity. Therefore, future health planning needs to consider an environment whereby RWAME movement may be degraded or denied by a near-peer, peer or superior threat. To that end, an exploration of alternative approaches to surgical management of injured personnel is pertinent. Life-saving surgical intervention may be delivered by deploying mobile surgical assets forward rather than
relying on evacuation of casualty rearward. Shortly after the arrival of surgical resources to the point of injury, temporising damage control procedures may begin, removing the delay associated with casualty preparation, package and transfer. Essentially, the concept is to significantly augment Role 1 activities for a time-limited period to increase the evacuation window allowing patients to survive that would otherwise die on the battlefield if rapid evacuation capability was degraded or denied. An exploration of the surgical procedures, anaesthetic considerations and transport logistics associated with these interventions is presented in this paper. Limitations on the concept include tactical training requirement of forward deployed medical staff, definition and description of surgical intervention offered and prerequisite civilian skillset, attendant load list, and considerations of anaesthetic delivery and casualty hold elements.
14/03/2021
Hydrazine: Qu'est ce que c'est ?
The Toxicity, Pathophysiology, and Treatment of Acute Hydrazine Propellant Exposure: A Systematic Review
Nguyen HN et Al. Mil Med. 2021 Feb 26;186(3-4):e319-e326.
-----------------------------------
L'hydrazine est employé comme combustible dans les fusées et dans les F16 américains en tant que combustible alimentant une unité de puissance de secours. Et cela n'est pas sans conséquence lors d'une intervention auprès d'un tel type d'aéronef.
-----------------------------------
Introduction:
Hydrazines are highly toxic inorganic liquids that are used as propellants in military and aviation industries, such as the U.S. Air Force F-16 Emergency Power Unit and SpaceX SuperDraco Rockets. The most commonly used derivatives include hydrazine, monomethylhydrazine, and 1,1-dimethylhydrazine (unsymmetrical dimethylhydrazine). Industrial workers in close contact with hydrazines during routine maintenance tasks can be exposed to levels well above the National Institute for Occupational Safety and Health relative exposure limits.
Materials and methods: A systematic review was performed using PubMed, Web of Science, Google Scholar, National Aeronautics and Space Administration Technical Server, and Defense Technical Information Center, and data related to hydrazine exposures were searched from inception to April 2020. Publications or reports addressing hydrazine toxicity, pathophysiology, and treatment of hydrazine fuel exposure were selected.
Results: Acute toxic exposures to hydrazine and its derivatives are rare. There are few case reports of acute toxic exposure in humans, and data are largely based on animal studies. The initial search identified 741 articles, manuscripts, and government reports. After screening for eligibility, 51 were included in this review. Eight articles reported acute exposures to hydrazine propellant in humans, and an additional 14 articles reported relevant animal data.
Conclusions: Exposure to small amounts of hydrazine and its derivatives can cause significant soft tissue injury, pulmonary injury, seizures, coma, and death. Neurologic presentations can vary based on exposure compound and dose. Decontamination is critical as treatment is mainly supportive. High-dose intravenous pyridoxine has been suggested as treatment for hydrazine-related neurologic toxicity, but this recommendation is based on limited human data. Despite recent research efforts to generate less toxic alternatives to hydrazine fuel, it will likely continue to have a role in military and aviation industries. Aerospace and military physicians should be aware of the toxicity associated with hydrazine exposure and be prepared to treat hydrazine toxicity in at-risk populations.
01/03/2021
Le traumatisé grave en milieu montagneux
Multiple trauma management in mountain environments - a scoping review.
Sumann, G. et al. Scand J Trauma Resusc Emerg Med 28, 117 (2020).
Background
Multiple trauma in mountain environments may be associated with increased morbidity and mortality compared to urban environments.
Objective
To provide evidence based guidance to assist rescuers in multiple trauma management in mountain environments.
Eligibility criteria
All articles published on or before September 30th 2019, in all languages, were included. Articles were searched with predefined search terms.
Sources of evidence
PubMed, Cochrane Database of Systematic Reviews and hand searching of relevant studies from the reference list of included articles.
Charting methods
Evidence was searched according to clinically relevant topics and PICO questions.
Results
Two-hundred forty-seven articles met the inclusion criteria. Recommendations were developed and graded according to the evidence-grading system of the American College of Chest Physicians. The manuscript was initially written and discussed by the coauthors. Then it was presented to ICAR MedCom in draft and again in final form for discussion and internal peer review. Finally, in a face-to-face discussion within ICAR MedCom consensus was reached on October 11th 2019, at the ICAR fall meeting in Zakopane, Poland.
Conclusions
Multiple trauma management in mountain environments can be demanding. Safety of the rescuers and the victim has priority. A crABCDE approach, with haemorrhage control first, is central, followed by basic first aid, splinting, immobilisation, analgesia, and insulation. Time for on-site medical treatment must be balanced against the need for rapid transfer to a trauma centre and should be as short as possible. Reduced on-scene times may be achieved with helicopter rescue. Advanced diagnostics (e.g. ultrasound) may be used and treatment continued during transport.
02/01/2020
Methoxyflurane en altitude ? Mais oui
WIlkes M et Al. Wilderness Environ Med. 2018 Sep;29(3):388-391.
Methoxyflurane is a volatile, fluorinated anesthetic agent with analgesic properties. Although no longer used as an anesthetic due to concerns regarding renal toxicity in high doses, it has enjoyed a resurgence as an inhaled analgesic in prehospital care and in the emergency department. The agent is nonflammable and leads to rapid, titratable analgesia without intravenous access. The Penthrox inhaler device is light, robust, and straightforward to administer. Consequently, it has been proposed as an ideal analgesic for the remote high altitude setting.

We report its use for procedural analgesia during suprapubic aspiration for acute urinary retention at a remote rescue post at night, in cold winter conditions, at 4470 m altitude in Machermo, Nepal. We found that methoxyflurane provided rapid, effective analgesia for our patient’s visceral and procedural pain. The inhaler was easy to administer, and the patient remained responsive to voice, with satisfactory oxygen saturation and respiratory rate throughout. We also briefly review the administration, dosing, efficacy, and safety of methoxyflurane and its role in remote medical care.
13/09/2019
Médecine et parachutisme dans les armées
29/07/2019
Methoxyflurane en altitude ? Mais oui
WIlkes M et Al. Wilderness Environ Med. 2018 Sep;29(3):388-391.
Methoxyflurane is a volatile, fluorinated anesthetic agent with analgesic properties. Although no longer used as an anesthetic due to concerns regarding renal toxicity in high doses, it has enjoyed a resurgence as an inhaled analgesic in prehospital care and in the emergency department. The agent is nonflammable and leads to rapid, titratable analgesia without intravenous access. The Penthrox inhaler device is light, robust, and straightforward to administer. Consequently, it has been proposed as an ideal analgesic for the remote high altitude setting.

We report its use for procedural analgesia during suprapubic aspiration for acute urinary retention at a remote rescue post at night, in cold winter conditions, at 4470 m altitude in Machermo, Nepal. We found that methoxyflurane provided rapid, effective analgesia for our patient’s visceral and procedural pain. The inhaler was easy to administer, and the patient remained responsive to voice, with satisfactory oxygen saturation and respiratory rate throughout. We also briefly review the administration, dosing, efficacy, and safety of methoxyflurane and its role in remote medical care.
16/03/2019
Irak/Syrie: Quelle activité ?
The First 30 Months Experience in the Non-Doctrinal Operation Inherent Resolve Medical Theater
Schauer SG et Al. Mil Med. 2018 Nov 5. doi: 10.1093/milmed/usy273
----------------------------------------------------
Les auteurs rapportent le soutien médical de combats menés essentiellement par des troupes amies. La lecture des fichiers associés à la publication s'impose. Pose de garrot et réchauffement sont les gestes préhospitaliers les plus fréquents. Il faut noter, au niveau des structures chirurgicales la fréquence des drainages thoraciques, des intubations et des laparotomies.
----------------------------------------------------
Introduction:
U.S. military forces were redeployed in 2014 in support of Operation Inherent Resolve (OIR), operating in an austere theater without the benefit of an established medical system. We seek to describe the prehospital and hospital-based care delivered in this medically immature, non-doctrinal theater.
Materials and Methods:
We queried the Department of Defense Trauma Registry (DODTR) for all encounters associated with OIR from August 2014 through June 2017. We sought all available prehospital and hospital-based data.
Results:
There were a total of 826 adults that met inclusion; 816 were from Iraq and the remaining 10 were from Syria. The median age was 21 years and the most frequent mechanism of injury was explosives (47.7%). Median composite injury severity scores were low (9, IQR 2.75-14) and the most frequent seriously injured body region was the extremities (23.0%). Most subjects (94.9%) survived to hospital discharge. Open fractures were the most frequent major injury (26.0%). In the prehospital setting, opioids were the most frequently administered medication (9.3%) and warming blanket application (48.7%) and intravenous line placement (24.8%) were the most frequent interventions. In the emergency department, Focused Assessment with Sonography in Trauma exams (64.3%) was the most frequently performed study and endotracheal intubations were the most frequent (29.9%) procedure. In the operating room, the most frequently performed procedure was exploratory laparotomy (12.3%).
Conclusions:
Host nation military males injured by explosion comprised the majority of casualties. Open fracture was the most common major injury. Hence, future research should focus upon the unique challenges of delivering care to members of partner forces with particular focus upon interventions to optimize outcomes among patients sustaining open fractures.
24/01/2019
Soutien médical en Mer de Kara
09/12/2018
Tuerie massive: Les 30 premières min.
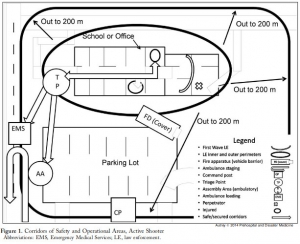
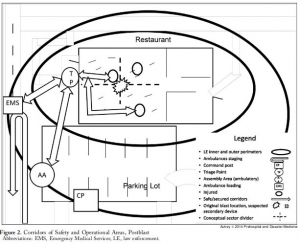
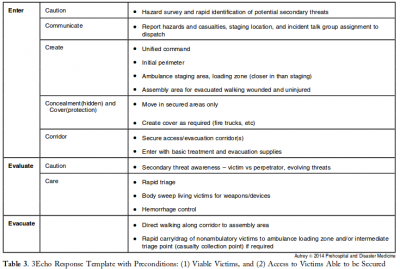
3 Echo: concept of operations for early care and evacuation of victims of mass violence
This report describes the successful use of a simple 3-phase approach that guides the initial 30 minutes of a response to blast and active shooter events with casualties: Enter, Evaluate, and Evacuate (3 Echo) in a mass-shooting event occurring in Minneapolis, Minnesota USA, on September 27, 2012. Early coordination between law enforcement (LE) and rescue was emphasized, including establishment of unified command, a common operating picture, determination of evacuation corridors, swift victim evaluation, basic treatment, and rapid evacuation utilizing an approach developed collaboratively over the four years prior to the event. Field implementation of 3 Echo requires multi-disciplinary (Emergency Medical Services (EMS), fire and LE) training to optimize performance.
This report details the mass-shooting event, the framework created to support the response, and also describes important aspects of the concepts of operation and curriculum evolved through years of collaboration between multiple disciplines to arrive at unprecedented EMS transport times in response to the event.
19/10/2018
Intubation dans le noir: Plutôt Poncho que JVN
OBJECTIVE:
Strict blackout discipline is extremely important for all military units. To be able to effectively determine wound characteristics and perform the necessary interventions at nighttime, vision and light restrictions can be mitigated through the use of tactical night vision goggles (NVGs). The lamp of the classical laryngoscope (CL) can be seen with the naked eye; infrared light, on the other hand, cannot be perceived without the use of NVGs. The aim of the study is to evaluate the safety of endotracheal intubation (ETI) procedures in the darkunder tactically safe conditions with modified laryngoscope (ML) model.
METHODS:
We developed an ML model by changing the standard lamp on a CL with an infrared light-emitting diode lamp to obtain a tool which can be used to perform ETI under night conditions in combination with NVGs. We first evaluated the safety of ETI procedures in prehospital conditions under darkness by using both the CL and the ML for the study, and then researched the procedures and methods by which ETI procedure could be performed in the dark under tactically safe conditions. In addition, to better ensure light discipline in the field of combat, we also researched the benefits, from a light discipline standpoint, of using the poncho liner (PL) and of taking advantage of the oropharyngeal region during ETIs performed by opening the laryngoscope blades directly in the mouth and using a cover. During the ETI procedures performed on the field, two experienced combatant staff simulated the enemy by determining whether the light from the two different types of laryngoscope could be seen at 100-m intervals up to 1,500 m.
RESULTS:
In all scenarios, performing observations with an NVG was more advantageous for the enemy than with the naked eye. The best measure that can be taken against this threat by the paramedic is to ensure tactical safety by having an ML and by opening the ML inside the mouth with the aid of a PL. The findings of the study are likely to shed light on the tactical safety of ETI performed with NVGs under darkness.
CONCLUSION:
Considering this finding, we still strongly recommend that it would be relatively safer to open the ML blade inside the mouth and to perform the procedures under a PL. In chaotic environments where it might become necessary to provide civilian health services for humanitarian aid purposes (Red Crescent, Red Cross, etc.) without NVGs, we believe that it would be relatively safer to open the CL blade inside the mouth and to perform the procedures under a PL.
Pour voir: Etre dans le bleu!
Safest light in a combat area while performing intravenous access in the dark.
INTRODUCTION:
Cannulation for the administration of intravenous fluids is integral to the prehospital management of injured military patients. However, this may be technically challenging to undertake during night-time conditions where the use of light to aid cannulation may give the tactical situation away to opponents. The aim of this study was to investigate the success and tactical safety of venepuncture under battlefield conditions with different colour light sources.
METHOD:
The procedure was carried out with naked eye in a bright room in the absence of a separate light source, with a naked eye in a dark room under red, white, blue and green light sources and under an infrared light source while wearing night vision goggles (NVGs). The success, safety, degree of difficulty and completion time for each procedure were then explored.
RESULTS:
All interventions made in daylight and in a dark room were found to be 100% successful. Interventions performed under infrared light while wearing NVGs took longer than under other light sources or in daylight. Interventions performed under blue light were tactically safer when compared with interventions performed under different light sources.
CONCLUSION:
Blue light offered the best tactical safety during intravenous cannulation under night-time conditions and is recommended for future use in tactical casualty care. The use of NVGs using infrared light cannot be recommended if there is the possibility of opponents having access to the technology.
25/09/2018
Intervenir sur une tuerie massive: Un savoir faire à acquérir
This report describes the successful use of a simple 3-phase approach that guides the initial 30 minutes of a response to blast and active shooter events with casualties: Enter, Evaluate, and Evacuate (3 Echo) in a mass-shooting event occurring in Minneapolis, Minnesota USA, on September 27, 2012. Early coordination between law enforcement (LE) and rescue was emphasized, including establishment of unified command, a common operating picture, determination of evacuation corridors, swift victim evaluation, basic treatment, and rapid evacuation utilizing an approach developed collaboratively over the four years prior to the event. Field implementation of 3 Echo requires multi-disciplinary (Emergency Medical Services (EMS), fire and LE) training to optimize performance.
This report details the mass-shooting event, the framework created to support the response, and also describes important aspects of the concepts of operation and curriculum evolved through years of collaboration between multiple disciplines to arrive at unprecedented EMS transport times in response to the event.
18/03/2018
Combat en montagne: Soutien médical
Challenges of Military Health Service Support in Mountain Warfare
Raimund Lechner et Al. https://doi.org/10.1016/j.wem.2018.01.006
------------------
Un environnement hostile pour des blessés particuliers et des équipes médicales dont l'entraînement doit être au plus haut. Lire aussi
------------------
Introduction
History is full of examples of the influence of the mountain environment on warfare. The aim of this article is to identify the main environmental hazards and summarize countermeasures to mitigate the impact of this unique environment.
Methods
A selective PubMed and Internet search was conducted. Additionally, we searched bibliographies for useful supplemental literature and included the recommendations of the leading mountain medicine and wilderness medicine societies.
Results
A definition of mountain warfare mainly derived from environmental influences on body functions is introduced to help identify the main environmental hazards. Cold, rugged terrain, hypoxic exposure, and often a combination and mutual aggravation of these factors are the most important environmental factors of mountain environment. Underestimating this environmental influence has decreased combat strength and caused thousands of casualties during past conflicts. Some marked differences between military and civilian mountaineering further complicate mission planning and operational sustainability.
Conclusions
To overcome the restrictions of mountain environments, proper planning and preparation, including sustained mountain mobility training, in-depth mountain medicine training with a special emphasize on prolonged field care, knowledge of acclimatization strategies, adapted time calculations, mountain-specific equipment, air rescue strategies and makeshift evacuation strategies, and thorough personnel selection, are vital to guarantee the best possible medical support. The specifics of managing risks in mountain environments are also critical for civilian rescue missions and humanitarian aid.
17/01/2018
Guide de médecine rurale AUS
12/11/2017
Retex du soutien d'une opération aéroportée
-----------------------------
Un publication déjà ancienne, mais l'expérience rapportée est assez unique et porte sur l'emploi d'une antenne chirurgicale et des conditions d'emploi lors des premières heures.
-----------------------------
Flying directly from its home station in Vicenza, Italy, the 173rd Airborne Brigade committed itself to the invasion of Iraq on the night of March 26, 2003. Representing the establishment of a northern front, approximately 1,000 paratroopers jumped into an isolated valley on a mission to secure and to hold the Bashur airstrip. This article describes the unique challenges of medical preparation for the mission, injuries sustained on the jump, and lessons learned. Emphasis is placed on the use of a policy of delayed evacuation until clarification of diagnosis.
Lunettes de vision nocturne: Une aide ? A voir !
-----------------------------------
Des résultats bien étonnants quand on connait les problèmes de profondeur de champ inhérents à l'emploi de dispositifs de vision nocturne, surtout monoculaires. Comme toujours maîtriser le geste en conditions normales, maîtriser l'outil de vision et s'entraîner dans ces conditions. Lire également 1, 2, 3
-----------------------------------
BACKGROUND:
In the patients with multiple and serious trauma, early applications of life-saving procedures are related to improved survival. We tried to experimentally determine the feasibility of life-saving interventions that are performed with the aid of night vision goggles (NVG) in nighttime combat scenario.
METHODS:
Chest tube thoracostomy (CTT), emergency cricothyroidotomy (EC), and needle thoracostomy (NT) interventions were performed by 10 combatant medical staff. The success and duration of interventions were explored in the study. Procedures were performed on the formerly prepared manikins/models in a bright room and in a dark room with the aid of NVG. Operators graded the ease of interventions.
RESULTS:
All interventions were found successful. Operators stated that both CTT and EC interventions were more difficult in dark than in daytime (p<0.05). No significant difference was observed in the difficulty in the NT interventions. No significant difference was observed in terms of completion times of interventions between in daytime and in dark scenario.
CONCLUSION:
The operators who use NVGs have to be aware of that they can perform their tactic and medical activities without taking off the NVGs and without the requirement of an extra light source.
| Tags : vision nocturne
21/01/2017
Gelures graves: Plus tôt la thrombolyse
Severe frostbite is associated with high levels of morbidity through loss of digits or limbs. The aim of this study was to examine the salvage rate following severe frostbite injury. Frostbite patients from 2006 to 2014 were identified in the prospectively maintained database at a single urban burn and trauma center. Patients with imaging demonstrating a lack of blood flow in limbs/digits were included in the analysis (N = 73). The Hennepin Frostbite Score was used to quantify frostbite injury and salvage. This score provides a single value to assess each individual patient's salvage rate. The majority of patients with perfusion deficits were male (80%) with an average age of 42 years (range 11-83 years). Patients requiring amputation tended to be older (P = .002), have more tissue impacted by frostbite (P < .001), and experienced a longer time from rewarming to thrombolytic therapy (P = .001). A majority of patients (62%) received thrombolytic treatment. The percentage of patients requiring amputation was lower and the salvage rate was higher in patients treated with thrombolytics; however, the differences failed to reach statistical significance (P = .092 and P = .061, respectively). The rate of salvage decreases as the time from rewarming to thrombolytic therapy increases. Regression analysis demonstrates an additional 26.8% salvage loss with each hour of delayed treatment (P = .006). When the amount of tissue at risk for amputation is included in the model, each hour delay in thrombolytic treatment results in a 28.1% decrease in salvage (P = .011). This study demonstrates a significant decrease in limb/digit salvage with each hour of delayed administration of thrombolytics in patients with severe frostbite
| Tags : gelures