16/12/2025
Quoi d'autre que le sang pour le choc hémorragique: ?
Adjuvant therapies for management of hemorrhagic shock: a narrative review
Daniel Y et Al. Crit Care. 2025 Mar 29;29(1):138
BackgroundSevere bleeding remains a leading cause of death in patients with major trauma, despite improvements in care during the acute phase, especially the application of damage control concepts. Death from hemorrhage occurs rapidly after the initial trauma, in most cases before the patient has had a chance to reach a hospital. Thus, the development of adjuvant drugs that would increase the survival of injured patients is necessary. Among the many avenues of research in this area, one is to improve cell survival during tissue hypoxia. During hemorrhagic shock, oxygen delivery to cells decreases and, despite increased oxygen extraction, anaerobic metabolism occurs, leading to acidosis, coagulopathy, apoptosis, and organ dysfunction.
Methods
We selected six treatments that may help cells cope with this situation and could be used as adjuvant therapies during the initial resuscitation of severe trauma patients, including out-of-hospital settings: niacin, thiazolidinediones, prolyl hydroxylase domain inhibitors, O-GlcNAcylation stimulation, histone deacetylase inhibitors, and adenosine–lidocaine–magnesium solution. For each treatment, the biological mechanism involved and a systematic review of its interest in hemorrhagic shock (preclinical data and human clinical trials) are presented.

Conclusion
Promising molecules, some of which are already used in humans for other indications, give us hope for human clinical trials in the field of hemorrhagic shock in the near future
13/12/2025
Ketamine intranasale: Bon pour le service ?
Breathing new life into pain management: a systematic review of nebulised ketamine for analgesia
Daniel Kirk D et Al. Scand J Trauma Resusc Emerg Med. 2025 Dec 4;33(1):196.
Background:
Acute pain accounts for 60-90% of presentations to the emergency department (ED), with 20-40% of patients reporting severe pain. Current management practices, including simple analgesics, opiates and anti-inflammatory drugs, are often inadequate or slow to reach peak effect, necessitating the exploration of alternative analgesics. Ketamine, acting primarily through N-methyl-D-aspartate (NMDA) receptor antagonism, presents a promising alternative due to its rapid onset. However, its nebulised form remains underutilised in clinical practice.
Aims and objectives:
This review evaluates the efficacy of nebulised ketamine in reducing pain in adult ED patients, alongside its side effect profile, optimal dosing, and potential as an alternative or adjunctive analgesic compared to other treatments.
Methods and design:
A systematic review utilising the PRISMA guidelines was conducted. Searches were carried out in Medline, Embase, PubMed, Science Direct, google scholar and Ovid databases from 2010 to May 2024, including studies containing objective analysis of pain control with nebulised ketamine. A two-sample t-test was used to assess statistical significance. Quality assessment was performed using the CASP tool, and bias was evaluated using the ROBINS-I and ROB2 tool.
Results:
Of 99 articles, 9 (5 randomised controlled trials, 3 case series and 1 case report) totalling 453 patients were included. All studies suggested improvement in pain scores with nebulised ketamine, with an average reduction of 42.5% and 70.4% over a 15 and 120-minute period respectively (p < 0.0001). Higher doses (1 mg/kg, 1.5 mg/kg) did not significantly improve pain compared to lower doses (0.7 mg/kg 0.75 mg/kg), with similar overall reductions reported across all four dosing regimens (p < 0.0003 or 0.0001).
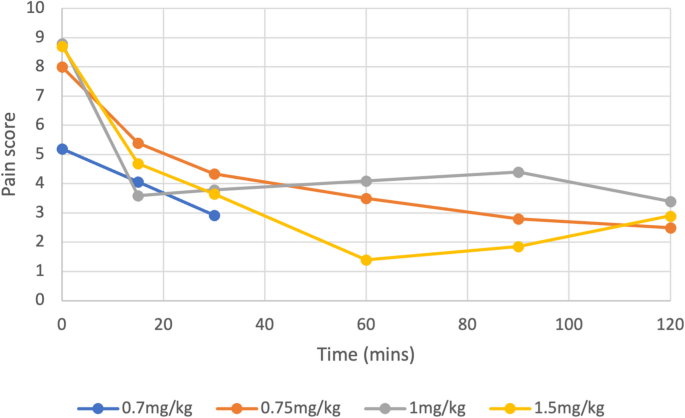
Nebulised ketamine was non-inferior to intravenous (IV) morphine, IV ketamine, nebulised dexmedetomidine, and Entonox, and had fewer side effects.
Conclusion: Nebulised ketamine offers a viable alternative for pain management in emergency settings, providing effective analgesia with a favourable safety profile. Further multicentre trials with larger populations are recommended to confirm these findings and establish standardised dosing protocols for consideration in national guidance.
12/12/2025
TXA: 2g IV si trauma crânien
Optimal dose of tranexamic acid in traumatic brain injury: Systematic review and network meta-analysis of randomized controlled trials
Shu U et Al Journal of Trauma and Acute Care Surgery 98(5):p 816-823, May 2025.
BACKGROUND
Tranexamic acid (TXA) has been used to treat traumatic brain injury (TBI); however, no definitive conclusions have been drawn regarding its effectiveness or dosage. This study evaluated the optimal TXA dose for treating TBI using a network meta-analysis (NMA).
METHODS
Five databases were searched for peer-reviewed randomized controlled trials (RCTs) published from inception to May 2024. The inclusion criteria were as follows: (1) RCTs, (2) patients older than 1 month with TBI, (3) interventions of TXA and control, (4) primary outcomes of mortality and poor neurological outcomes and secondary outcomes of vascular occlusive events, and (5) full-text peer-reviewed articles. Two reviewers independently screened and extracted the data and assessed the risk of bias. Frequency-based NMA was performed using the Grading of Recommendations, Assessment, Development, and Evaluation working-group approach.
RESULTS
We included 10 RCTs comprising 11,237 patients with TBI. Placebo showed higher mortality compared with that of a 2-g bolus of TXA (risk ratio, 1.53; 95% confidence interval, 1.08–2.17). Higher mortality was observed with a 1-g bolus of TXA followed by 1-g maintenance TXA compared with that of a 2-g bolus of TXA (risk ratio, 1.44; 95% confidence interval, 1.02–2.03). No significant differences in poor neurological outcomes or vascular occlusive events were observed between the treatment groups.

CONCLUSION
Placebo and a 1-g bolus followed by 1-g maintenance TXA were associated with higher mortality rates than those of a 2-g bolus of TXA. No difference in vascular occlusive events was observed with either treatment, indicating that our NMA recommends 2 g of TXA. However, the data for the 2-g bolus of TXA were from a single study, and further research is needed to draw definitive conclusions.
Récapitulatif sur le remplissage vasculaire/Transfusion
Fluid resuscitation in trauma: What you need to know
Navpreet D et Al. Journal of Trauma and Acute Care Surgery 98(1):p 20-29, January 2025.
There have been numerous changes in resuscitation strategies for severely injured patients over the last several decades. Certain strategies, such as aggressive crystalloid resuscitation, have largely been abandoned because of the high incidence of complications and worsening of trauma-induced coagulopathy. Significant emphasis has been placed on restoring a normal coagulation profile with plasma or whole blood transfusion. In addition, the importance of the lethal consequences of trauma-induced coagulopathy, such as hyperfibrinolysis, has been easily recognized by the use of viscoelastic testing, and its treatment with tranexamic acid has been extensively studied. Furthermore, the critical role of early intravenous calcium administration, even before blood transfusion administration, has been emphasized.

Other adjuncts, such as fibrinogen supplementation with fibrinogen concentrate or cryoprecipitate and prothrombin complex concentrate, are being studied and incorporated in some of the institutional massive transfusion protocols. Finally, balanced blood component transfusion (1:1:1 or 1:1:2) and whole blood have become commonplace in trauma centers in North America. This review provides a description of recent developments in resuscitation and a discussion of recent innovations and areas for future investigation.
eFAST et thorax ouvert: Manque de sensibilité +++
Accuracy, reliability, and utility of the extended focused assessment with sonography in trauma examination in the setting of thoracic gunshot wounds
Miharu A et Al. Journal of Trauma and Acute Care Surgery 98(6):p 867-874, June 2025.
------------------------------------------
eFAST en cas de thorax ouvert ? Et bien pas si sûr
------------------------------------------
BACKGROUND
The extended focused assessment with sonography in trauma (eFAST) examination includes additional thoracic views beyond the standard focused assessment with sonography in trauma examination. Its validation has predominantly been conducted in blunt trauma cases. Our aim was to evaluate the eFAST examination in a targeted population with penetrating thoracic trauma.
METHODS
Patients with thoracic gunshot wounds who underwent eFAST between 2017 and 2021 were included from a local trauma registry. Performance metrics for each component of eFAST in each window and pathological condition were analyzed across the entire population, as well as within two cohorts: survived and deceased patients. Chest tube placement rates were compared within true-positive and false-negative (FN) eFAST results for subgroups with pneumothorax or hemothorax.
Miharu A et Al. Journal of Trauma and Acute Care Surgery 98(6):p 867-874, June 2025.
RESULTS
A total of 288 patients were included (male, 91% male; Injury Severity Score ≥15, 48%; and died, 17%). Thirty-nine percent required chest tube, and 18% required urgent thoracic surgical intervention. Although specificity was high (91–100%) for all components, the sensitivity was less than 50% for all thoracic views, except for “no cardiac motion” (100% sensitivity). Sensitivity for pericardial fluid was 47%; for pneumothorax, 22%; for hemothorax, 36%; and for peritoneal fluid, 51% in the total population. Comparing survived versus deceased cohort, the eFAST sensitivity was higher among deaths for all components. The majority of patients (>70%) with a FN eFAST for pneumothorax or hemothorax received chest tube.

CONCLUSION
The eFAST examination showed highly variable performance metrics among patients with penetrating thoracic trauma, with all thoracic components demonstrating high specificity but low overall sensitivity. Urgent interventions were frequently received in patients with FN studies.
le x et M avant A. Transfuser avant d'intuber ?
Prioritizing circulation over airway in trauma patients with exsanguinating injuries: What you need to know.
Paula Ferrada P et Al. J Trauma Acute Care Surg. 2025 Jul 4.
----------------------------------------------------
Hemorrhage remains a leading cause of preventable trauma-related mortality, with early resuscitation and hemorrhage control serving as crucial interventions. Emerging evidence suggests that prioritizing circulation before airway (Circulation, Airway, and Breathing [CAB]) during initial resuscitation in patients with exsanguinating injuries can improve survival by avoiding the deleterious effects of postintubation hypotension. This article reviews current evidence supporting the CAB approach and outlines best practices across prehospital, emergency department, and operative settings. Delaying advanced airway management while focusing on immediate hemorrhage control and blood product resuscitation has been associated with decreased 24-hour and 30-day mortality. This review synthesizes findings from recent multicenter trials and literature supporting the CAB paradigm, with practical recommendations for implementation in trauma care systems.
----------------------------------------------------
07/12/2025
Thèse PSL innovants pour le blessé de guerre
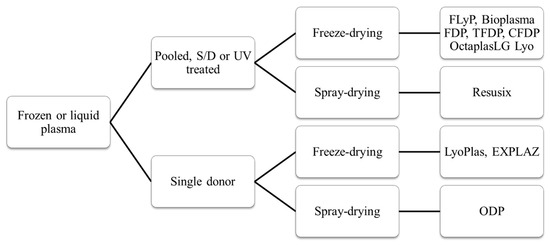
Vers un nouveau Plyo
Efficacy and safety of novel freeze-dried plasma products in a porcine combat casualty model
Dufour-Gaume F et Al. Transfusion. 2024 Sep;64(9):1670-1682
-----------
Le Plyo est un des produits phares développé par le CTSA. Les recherches continuent pour améliorer les caractérisques. C'est le sens de ce tavail qui porte sur du Plyo plus concentré ou enrichi en lyophylisat de plaquettes. Ce dernier produit parait particulièrement intéressant. l'industrie pharmaceutique n'est pas en reste puisqu'elle propose maintenant des alternatives au PLyo standard comme l'OctaplastLG considéré comme un médicament et non plus un dérivé du sang.
-----------
Background
Hemorrhagic shock is well documented as a leading cause of preventable fatalities among military casualties. During military operations plasma can be transfused while waiting for whole blood. This study was conducted to assess the safety and efficacy of two new freeze-dried plasma formulations in a porcine model of traumatic hemorrhagic shock.
Study Design and Methods
In the face of species-specific transfusion, transfusible blood products were derived from porcine sources. The efficacy of three lyophilized plasma (LP) formulations was evaluated: lyophilized plasma (LP), concentrated lyophilized plasma (CLP), and platelet-rich concentrated lyophilized plasma (PCLP). Pigs were subjected to multi-trauma and hemorrhagic shock. Ninety minutes post-shock induction, the animals were treated with one of the three lyophilized products. Monitoring included systolic blood pressure and cardiac output. Point-of-care and laboratory diagnostic tests were used to assess renal function, real-time hemostasis (ROTEM), and coagulation. Histological examinations of kidney, lung, and muscle tissues were conducted 4 h after shock induction.
Results
CLP and PCLP significantly improved systolic blood pressure and cardiac output and positively influenced base excess, creatinine, various ROTEM, and coagulation markers compared with standard LP without histologic modification. No adverse effect was associated with the transfusion of any of the plasma products throughout the experimental procedures.
Conclusion
Both CLP and PCLP exhibit promising therapeutic potential for managing hemorrhagic shock in scenario where whole blood supplies are limited. However, the distinct physiological and coagulation characteristics of the swine model necessitate further investigation using humanized preclinical models to fully understand their clinical applicability and constraints
Plasma: Un point en 2024
Dried Plasma for Major Trauma: Past, Present, and Future
05/12/2025
Point US sur l'emploi du TXA
Tranexamic acid in trauma: A joint position statement and resource document of NAEMSP, ACEP, and ACS-COT
Prehospital use of tranexamic acid (TXA) has grown substantially over the past decade despite contradictory evidence supporting its widespread use. Since the previous guidance document on the prehospital use of TXA for injured patients was published by the National Association of EMS Physicians, the American College of Surgeons Committee on Trauma, and the American College of Emergency Physicians in 2016, new research has investigated outcomes of patients who receive TXA in the prehospital setting. To provide updated evidence-based guidance on the use of intravenous TXA for injured patients in the emergency medical services (EMS) setting, we performed a structured literature review and developed the following recommendations supported by the evidence summarized in the accompanying resource document.
The National Association of EMS Physicians, the American College of Surgeons Committee on Trauma, and the American College of Emergency Physicians recommends:
• Prehospital TXA administration may reduce mortality in adult trauma patients with hemorrhagic shock when administered after lifesaving interventions.
• Prehospital TXA administration appears safe, with low risk of thromboembolic events or seizure.
• The ideal dose, rate, and route of prehospital administration of TXA for adult trauma patients with hemorrhagic shock has not been determined. Current evidence suggests EMS agencies may administer either a 1-g intravenous/intraosseous dose (followed by a hospital-based 1-g infusion over 8 hours) or a 2-g intravenous/intraosseous dose as an infusion or slow push.
• Prehospital TXA administration, if used for adult trauma patients, should be given to those with clinical signs of hemorrhagic shock and no later than 3 hours post-injury. There is no evidence to date to suggest improved clinical outcomes from TXA initiation beyond this time or in those without clinically significant bleeding.
• The role of prehospital TXA in pediatric trauma patients with clinical signs of hemorrhagic shock has not been studied, and standardized dosing has not been established. If used, it should be given within 3 hours of injury.
• Prehospital TXA administration, if used, should be clearly communicated to receiving health care professionals to promote appropriate monitoring and to avoid duplicate administration(s).
• A multidisciplinary team, led by EMS physicians, that includes EMS clinicians, emergency physicians, and trauma surgeons should be responsible for developing a quality improvement program to assess prehospital TXA administration for protocol compliance and identification of clinical complications.
02/12/2025
Les drones changent la donne