17/07/2019
Drainage thoracique chez l'enfant: La règle des 4
Rule of 4's: Safe and effective pleural decompression and chest drain insertion in severely injured children.
The intersecting scenarios of multi-trauma, thoracic injury and traumatic cardiac arrest present some of the most demanding moments in paediatric trauma. For these reasons, decision support through teamwork, checklists, technology and guidelines are central to ensuring quality paediatric trauma care. The 'Rule of 4's' is a simple aide-memoire, which guides clinicians of all grades, expertise and distractedness in a reliable approach to injured children who require safe and effective emergency pleural decompression and timely insertion of a chest drain.

The Rule of 4's enables these important therapeutic goals to be met through: (i) four steps in a 'good plan'; (ii) fourth (or fifth) intercostal space as the basis for siting a 'good hole'; (iii) 4× uncuffed endotracheal tube size (4× [age/4 + 4]) to guide selection of a 'good tube'; and (iv) 4 cm mark for a 'good stop' to ensure the drain is in far enough but not too far.
| Tags : drainage thorax
12/10/2017
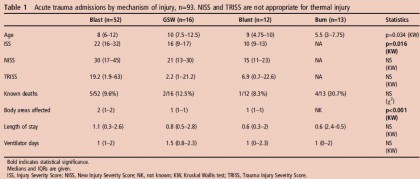
Chirurgie Pédiatrique en opex
10/01/2016
ERC 2015 Guidelines
10/12/2015
L'enfant blessé balistique: Vraiment spécial
Prehospital interventions in severely injured pediatric patients: Rethinking the ABCs
Sokol KK et Al. J Trauma Acute Care Surg. 2015;79: 983-990
-----------------------------------------------
Des résultats qui ne sont pas surprenants mais qui confirme la spécificités des trauma ballistiques et l'inadéquation d'algorithmes issus de la traumatologie routière.
-----------------------------------------------
BACKGROUND: The current conflict in Afghanistan has resulted in a high volume of significantly injured pediatric patients. The austere environment has demanded emphasis on prehospital interventions (PHIs) to sustain casualties during transport.
METHODS: The Department of Defense Trauma Registry was queried for all pediatric patients (e18 years) treated at Camp Bastion from 2004 to 2012. PHIs were grouped by Advanced Trauma Life Support categories into (1) airway (A) intubation or surgical airway; 2) breathing (B) chest tube or needle thoracostomy; and 3) circulation (C) tourniquet or hemostatic dressing. Outcomes were assessed based on injury severity, hemodynamics, blood products and fluids, as well as mortality rates.
RESULTS: There were 766 injured children identified with 20% requiring one or more PHIs, most commonly circulation (C, 51%) followed by airway (A, 40%) and breathing (B, 8.7%). The majority of C interventions were tourniquets (85%) and hemostatic dressings (15%). Only 38% of patients with extremity vascular injury or amputation received a C intervention, with a significant reduction in blood products and intravenous fluids associated with receiving a C PHI (both p G 0.05). A interventions consisted of endotracheal intubation for depressed mental status (Glasgow Coma Scale [GCS] score G 8). Among patients with traumatic brain injury, A interventions were associated with higher unadjusted mortality (56% vs. 20%, p G 0.01) and remained independently associated with increased mortality after multivariate adjustment (odds ratio, 5.9; p = 0.001). B interventions were uncommon and performed in only 2% of patients with no recorded adverse outcomes.
CONCLUSION: There is a high incidence of PHIs among pediatric patients with severe wartime injuries. The most common and effective were C PHI for hemorrhage control, which should remain a primary focus of equipment and training. A interventions were most commonly performed in the setting of severe traumatic brain injury but were associated with worse outcomes. B interventions seem safe and effective and may be underused
30/04/2014
Pédiatrie en OPEX: Vue US
| Tags : pédiatrie
14/01/2014
L'enfant traumatisé: Une rencontre CERTAINE
Management of children in the deployed intensive care unit at Camp Bastion, Afghanistan
Inwald DP, et al. J R Army Med Corps 2013;0:1–5. doi:10.1136/jramc-2013-000177
Background The deployed Intensive Therapy Unit (ITU) in the British military field hospital in Camp Bastion, Afghanistan, admits both adults and children. The purpose of this paper is to review the paediatric workload in the deployed ITU and to describe how the unit copes with the challenge of looking after critically injured and ill children.
Methods Retrospective review of patients <16 years of age admitted to the ITU in the British military field hospital in Camp Bastion, Afghanistan, over a 1-year period from April 2011 to April 2012.
Results 112/811 (14%) admissions to the ITU were paediatric (median age 8 years, IQR 6–12, range 1–16).80/112 were trauma admissions, 13 were burns, four were non-trauma admissions and 15 were readmissions.
Mechanism of injury in trauma was blunt in 12, blast (improvised explosive device) in 45, blast (indirect fire) in seven and gunshot wound in 16. Median length of stay was 0.92 days (IQR 0.45–2.65). 82/112 admissions (73%) were mechanically ventilated, 16/112 (14%) required inotropic support. 12/112 (11%) died before unit discharge. Trauma scoring was available in 65 of the 80 trauma admissions. Eight had Injury Severity Score or New Injury Severity Score >60, none of whom survived. However, of the 16 patients with predicted mortality >50% by Trauma Injury Severity Score, seven survived. Seven cases required specialist advice and were discussed with the Birmingham Children’s Hospital paediatric intensive care retrieval service. The mechanisms by which the Defence Medical Services support children admitted to the deployed adult ITU are described, including staff training in clinical, ethical and child protection issues, equipment, guidelines and clinical governance and rapid access to specialist advice in the UK.
Conclusions With appropriate support, it is possible to provide intensive care to children in a deployed military ITU.
| Tags : pédiatrie
15/07/2012
Aide mémoire d'anesthésie pédiatrique
| Tags : pédiatrie
15/04/2012
Borden Institute: Pédiatrie