17/06/2012
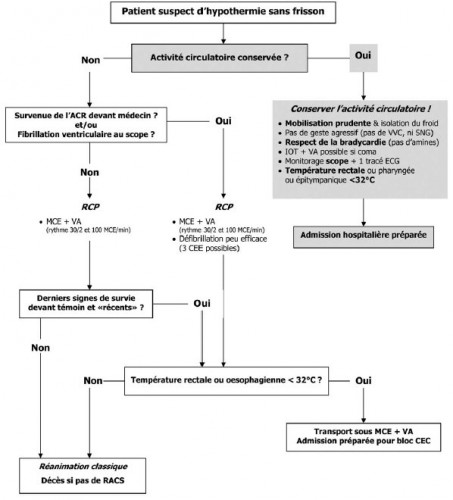
Prise en charge d’un blessé en hypothermie accidentelle
Prise en charge d’un malade en hypothermie accidentelle
Briot R et all. Réanimation (2010) 19, 607—615
ATTENTION le réchauffement préhospitalier a pour objectif de limiter l'hypothermie.
ATTENTION un réchauffement actif préhospitalier n'est pas indiqué si l'hypothermie est profonde
ATTENTION le réchauffement actif préhospitalier est d'autant plus efficace si la conscience et le frisson persistent
05/05/2012
Ready heat ou triple couche ?
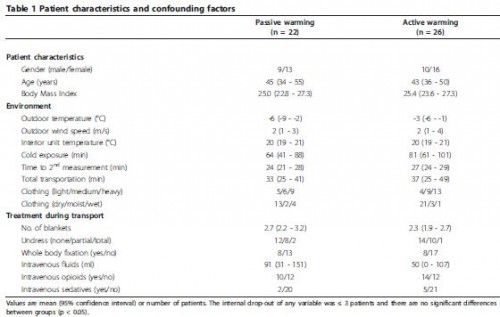
The effect of active warming in prehospital trauma care during road and air ambulance transportation - a clinical randomized trial.
Lundgren P. et all Scand J Trauma Resusc Emerg Med. 2011 Oct 21;19:59.
La prévention de l'hypothermie fait appel à des moyens de réchauffement cutanés passifs ( couverture renforcée type Rothco ou la couverture triple couche type blizzard blanket ) ou actifs (couverture ready-heat). Mais comment choisir ?
Le travail présenté ici démontre qu'en présence d'une hypothermie modérée supérieures à 35°C il n'est pas utile d'avoir recours à un moyen actif en terme de limitation de l'hypothermie dès lors que le frisson est conservé. Le seul gain porte sur un confort thermique accru.
BACKGROUND:
Prevention and treatment of hypothermia by active warming in prehospital trauma care is recommended but scientific evidence of its effectiveness in a clinical setting is scarce. The objective of this study was to evaluate the effect of additional active warming during road or air ambulance transportation of trauma patients.
METHODS:
Patients were assigned to either passive warming with blankets or passive warming with blankets with the addition of an active warming intervention using a large chemical heat pad applied to the upper torso. Ear canal temperature, subjective sensation of cold discomfort and vital signs were monitored.
RESULTS:
Mean core temperatures increased from 35.1°C (95% CI; 34.7-35.5°C) to 36.0°C (95% CI; 35.7-36.3°C) (p < 0.05) in patients assigned to passive warming only (n = 22) and from 35.6°C (95% CI; 35.2-36.0°C) to 36.4°C (95% CI; 36.1-36.7°C) (p < 0.05) in patients assigned to additional active warming (n = 26) with no significant differences between the groups. Cold discomfort decreased in 2/3 of patients assigned to passive warming only and in all patients assigned to additional active warming, the difference in cold discomfort change being statistically significant (p < 0.05). Patients assigned to additional active warming also presented a statistically significant decrease in heart rate and respiratory frequency (p < 0.05).
CONCLUSIONS:
In mildly hypothermic trauma patients, with preserved shivering capacity, adequate passive warming is an effective treatment to establish a slow rewarming rate and to reduce cold discomfort during prehospital transportation. However, the addition of active warming using a chemical heat pad applied to the torso will significantly improve thermal comfort even further and might also reduce the cold induced stress response.
| Tags : hypothermie
11/04/2012
Prise en charge des victimes d'avalanche ?
ICAR MEDCOM guidelines 2002
Il s'agit des recommandations de l'International Commission for Alpine Emergency Medicine
http://users.south-tyrolean.net/avalanche/pdf/Guidelines_...
Accidental Hypothermia
Accidental Hypothermia
Davis PR et all. J R Army Med Corps 2006; 152: 223-233
Une revue générale sur la prise en charge des hypothermies accidentelles. Il y en a d'autres mais son intérêt est d'être rédigée par nos collègues anglais
http://www.ramcjournal.com/2005/hostile_environments/davi...
12/02/2012
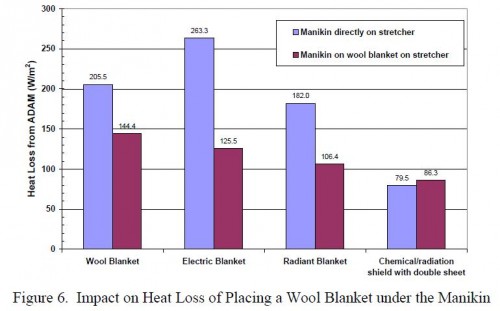
hypothermie: Isoler le blessé du brancard !
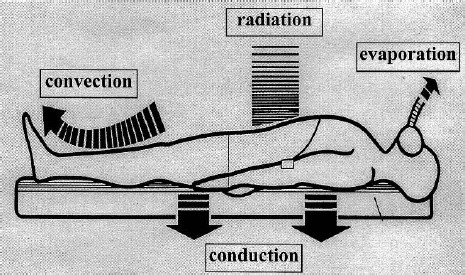
Les phénomènes de conduction ne doivent pas être négligés dans la génèse de l'hypothermie.
C'est ce que rappelle la publication suivante:
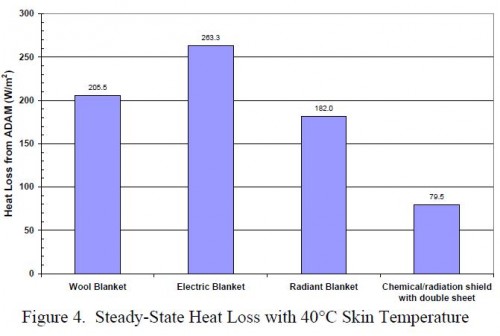
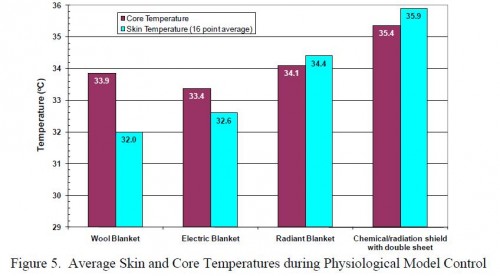
Assessment of Hypothermia Blankets Using an Advanced Thermal Manikin.
Rugh JP et All. Conference Paper NREL/CP-540-45888 July 2009
http://www.nrel.gov/vehiclesandfuels/ancillary_loads/pdfs...
| Tags : hypothermie
Hypothermie et couverture chimiques
Assessment of Hypothermia Blankets Using an Advanced Thermal Manikin.
Rugh JP et All. Conference Paper NREL/CP-540-45888 July 2009
http://www.nrel.gov/vehiclesandfuels/ancillary_loads/pdfs...
Elles sont efficaces. Elles ne doivent JAMAIS être placées au contact direct de la peau.
| Tags : hypothermie
05/02/2012
Hypothermie et la méthode de Hibbler
La méthode de hibbler est une méthode de prévention relativement simple faisant appel à la superposition d'au moins deux couvertures réflective +/- une source de chaleur. Le blessé doit être parfaitement emmailloté sans fuite d'air.
Il existe peu de littérature concernant la véritable efficacité des divers moyens employés. Le travail présenté par Thomassen et ses associés rappelle que des moyens simples sont aussi efficace que l'emploi de couvertures standards oude bubble Wrapp.
La fiche mémento sur l'hypothermie est accessible ici
23/01/2012
Prise en charge des gelures
10/12/2011
Military Mountaineering
07/05/2011
Hypothermie et traumatisé ne font pas bon ménage
Il est parfaitement démontré que l'hypothermie aggrave le pronostic vital des polytraumatisés. C'est un facteur indépendant de mortalité. Cette nouvelle publication le confirme. Elle précise par ailleurs que le risque d'hypothermie est accrue par un transport héliporté.
-------------------------------------------------
The incidence and significance of accidental hypothermia in major trauma—A prospective observational study
Ireland S et all.
Resuscitation 82 (2011) 300–306
Background
Serious sequelae have been associated with injured patients who are hypothermic (<35 °C) including coagulopathy, acidosis, decreased myocardial contractility and risk of mortality.
Aim
Establish the incidence of accidental hypothermia in major trauma patients and identify causative factors.
Method
Prospective identification and subsequent review of 732 medical records of major trauma patients presenting to an Adult Major Trauma Centre was undertaken between January and December 2008. Multivariate analysis was performed using logistic regression. Significant and clinically relevant variables from univariate analysis were entered into multivariate models to evaluate determinants for hypothermia and for death. Goodness of fit was determined with the use of the Hosmer–Lemeshow statistic.
Main results
Overall mortality was 9.15%. The incidence of hypothermia was 13.25%. The mortality of patients with hypothermia was 29.9% with a threefold independent risk of death: OR (CI 95%) 3.44 (1.48–7.99), P = 0.04. Independent determinants for hypothermia were pre-hospital intubation: OR (CI 95%) 5.18 (2.77–9.71), P < 0.001, Injury Severity Score (ISS): 1.04 (1.01–1.06), P = 0.01, Arrival Systolic Blood Pressure (ASBP) < 100 mm Hg: 3.04 (1.24–7.44), P = 0.02, and wintertime: 1.84 (1.06–3.21), P = 0.03.
Of the 87 hypothermic patients who had repeat temperatures recorded in the Emergency Department, 77 (88.51%) patients had a temperature greater than the recorded arrival temperature. There was no change in recorded temperature for four (4.60%) patients, whereas six (6.90%) patients were colder at Emergency Department discharge.
Conclusion
Seriously injured patients with accidental hypothermia have a higher mortality independent of measured risk factors. For patients with multiple injuries a coordinated effort by paramedics, nurses and doctors is required to focus efforts toward early resolution of hypothermia aiming to achieve a temperature >35 °C.
11/12/2010
Bubble Wrap et prévention de l'hypothermie ?
On sait que prévenir l'hypothermie est essentielle pour la survie d'un blessé.
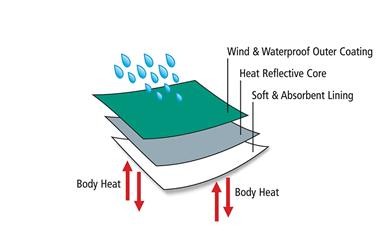
Les principales caractéristiques de la couverture idéale sont résumées sur ce schéma.
Nous disposons de nombreux moyens allant de la couverture simple, de la couverture renforcée, de la couverture triple couche et de la couverture chauffante. Tous les moyens de protection n'ont pas la même efficacité. Cette dernière est pour beaucoup liée à l'épaisseur des protections, leur caractère non compressible et hermétique ainsi que leur réflectivité (Lire). Une fiche mémo est disponible (Voir ici)
Nous connaissons tous également le système heatpac.
Mais savez vous que le films d'emballage à bulles (bubble wrap) sont très efficaces ( 1, 2).

Ces produits sont même commercialisés spécifiquement pour les besoins de santé.

Cette vidéo illustre la mise en oeuvre de ce produit Vidéo à voir.
07/11/2010
Réchauffer ACTIVEMENT le blessé sédaté
Un article à lire
Body temperature of trauma patients on admission to hospital: a comparison of anaesthetised and non-anaesthetised patients.
Langhelle A et all. Emerg Med J. 2010 Oct 20. [Epub ahead of print]
Abstract
Background Hypothermia at hospital admission has been found to independently predict increased mortality in trauma patients. Objectives To establish if patients anaesthetised in the prehospital phase of care had a higher rate of hypothermia than non-anaesthetised patients on admission to hospital. Methods Retrospective review of admission body temperature in 1292 consecutive prehospital trauma patients attended by a physician-led prehospital trauma service admitted to The Royal London Hospital between 1 July 2005 and 31 December 2008. Results 38% had a temperature recorded on admission. There was a significant difference in body temperature between the anaesthetised group (N=207) and the non-anaesthetised group (N=287): mean (SD) 35.0 (2.1) vs 36.2 (1.0)°C, respectively (p<0.001). No significant seasonal body temperature variation was demonstrated. Conclusion This study confirmed that patients anaesthetised in the prehospital phase of care had a significantly lower admission body temperature. This has led to a change in the author's prehospital practice. Anaesthetised patients are now actively surface heated and have whole body insulation to prevent further heat loss in an attempt to conserve body temperature and improve outcome. This is an example of best in-hospital anaesthetic practice being carried out in the prehospital phase.
En pratique
Le recours à l'association Ready Heat Blanket II, Blizzard Blanket et charlotte thermolite est impératif en cas de sédation préhospitalière (Voir ici). La prudence est de mise en cas d'hypothermie sévère sans frissons (voir ici). On rappelle simplement l'importance de prévenir l'installation de la triade hypoxie/coagulopathie/acidose lors de la prise en charge d'un blessé choqué hémorragique (Voir ici)
18/07/2010
Prévenir l'hypothermie sans source d'énergie électrique est possible !
Un article à lire:
Current Practice of Thermoregulation During the Transport of Combat Wounded - Nesbitt M. et all., J Trauma 69(1) Supplement:S162-S167, July 2010.
Voici l'abstract:
"AB Background: This study evaluated the progress in the treatment and prevention of hypothermia in combat wounded since the October 2, 2006 Joint Theater Trauma System Clinical Practice Guideline (CPG) publication and evaluated the frequency of use and effectiveness of the methods described in the CPG. Methods: The authors used data obtained from the Joint Trauma Theater Trauma Registry maintained by the US Army Institute of Surgical Research for our analysis. Results: The issuance of the CPG was associated with a decrease in the incidence of hypothermia (p value = <0.0001). None of the thermoregulatory methods were associated with significantly higher overall temperatures when compared with the others (p value = 0.1062-0.3686) or with hypothermia (p value = 0.1367-0.7992); however, lack of entered prehospital data resulted in a suboptimal number of patients for evaluation in this portion of the study. The wool blanket was the most commonly used thermoregulatory method (prehospital, 72%; interfacility, 49%). Conclusions: (1) The incidence of hypothermia decreased after the issuance of the JTTS CPG. (2) The standard Army wool blanket is the most commonly used thermoregulatory method during transport in theater. (3) This study did not find a significant difference in the capability of maintaining temperatures between the different thermoregulatory methods used in theater during either prehospital or interfacility transport, or in the incidence of hypothermia between patients presenting from the site of injury or from interfacility transport. (4) Data collected before a Level III facility is not consistently entered into the Joint Theater Trauma Registry. (C) 2010 Lippincott Williams & Wilkins, Inc."
En pratique:
- Vous avez en dotation la couverture triple couche Blizzard Blanket, la couverture chauffante Ready Heat Blanket II et la charlotte. L'approvisionnement se fait en articles séparés.
- La fiche mémento ici explique les principes généraux de la prévention de l'hypothermie
| Tags : hypothermie