17/01/2025
Conflit ukrainien: Pour de la chirurgie encore plus proche des combats
Du maintien des compétences: Un problème pour tous
Medical Training Falls Short at Army Combat Training Centers
Carius BM et Al. Military Medicine, Volume 190, Issue 1-2, January/February 2025, Pages 36–37
While combat arms project military strength and logistical support elements underwrite this power, medical support is vital for preservation of military life and readiness. We recently augmented different brigade rotations at an Army combat training center (CTC) as medical providers and find difficulty in confronting the depth and breadth of medical training inadequacies in support of this foundational training event. While we hope that our experiences are an aberrancy of isolated unit misfocus, the lack of medical training standards at Army CTCs demonstrates that rotational unit shortcomings are as much a byproduct of a systemic lack of medical training as individual organizations neglect. Despite coming from different backgrounds and experiences in medicine, the military, and CTC experience, we nevertheless came away with equally profound dismay at medical training shortfalls for both notional and real-world casualties.
As with most military forces, Army medics (medical occupational specialty 68W) are notably understrength and relatively inexperienced given exiting combat veterans and decreased deployments. Remaining medics disproportionately shoulder numerous administrative burdens, such as vehicle maintenance. This leaves little to no time to retain, refine, and practice basic skills initially taught in advanced individual training, let alone advance medical practices. Of dozens of medics we interacted with, all reported no substantial clinical opportunities to learn from direct supervision by a physician or physician assistant. Medics lacked essential pharmacotherapy understanding, including common medications like diphenhydramine and loperamide or emergent interventions such as epinephrine for anaphylaxis or pralidoxime for nerve agent exposure. The overwhelming majority acknowledged little clinical exposure beyond basic sick call. A small fraction of the few with combat experience expressed confidence with trauma management.
09/01/2025
Formation avant MEDEVAC Barkhane
ALR pour le médecin d'unité en situation isolée
02/01/2025
1 blessé sur 2 ne fait l'objet d'aucune mesure de sauvetage
Advancing Prehospital Combat Casualty Evacuation: Patients Amenable to Aeromedical Evacuation via Unmanned Aerial Vehicles
Maddry JK et Al. Mil Med. 2021 Feb 26;186(3-4):e366-e372.
Introduction: The U.S. military currently utilizes unmanned aerial vehicles (UAVs) for reconnaissance and attack missions; however, as combat environment technology advances, there is the increasing likelihood of UAV utilization in prehospital aeromedical evacuation. Although some combat casualties require life-saving interventions (LSIs) during medical evacuation, many do not. Our objective was to describe patients transported from the point of injury to the first level of care and characterize differences between patients who received LSIs en route and those who did not.
Materials and methods: We conducted a retrospective review of the records of traumatically injured patients evacuated between January 2011 and March 2014. We compared patient characteristics, complications, and outcomes based on whether they had an LSI performed en route (LSI vs. No LSI). We also constructed logistic regression models to determine which characteristics predict uneventful flights (no en route LSI or complications).
Results: We examined 1,267 patient records; 47% received an LSI en route. Most patients (72%) sustained a blast injury and injuries to the extremities and head. Over 78% experienced complications en route; the LSI group had higher rates of complications compared to the No LSI group. Logistic regression showed that having a blunt injury or the highest abbreviated injury scale (AIS) severity score in the head/neck region are significant predictors of having an uneventful flight.
Conclusion: Approximately half of casualties evaluated in our study did not receive an LSI during transport and may have been transported safely by UAV. Having a blunt injury or the highest AIS severity score in the head/neck region significantly predicted an uneventful flight.
01/01/2025
CrystalloIdes et choc hémorragique: Toujours d'actualité ?
Are crystalloid-based fluid expansion strategies still relevant in the first hours of trauma induced hemorrhagic shock?
Tubert P et Al.Crit Care. 2024 Dec 18;28(1):416.
OUI, mais
Background: Crystalloid-based fluid resuscitation has long been a cornerstone in the initial management of trauma-induced hemorrhagic shock. However, its benefit is increasingly questioned as it is suspected to increase bleeding and worsen coagulopathy. The emergence of alternative strategies like permissive hypotension and vasopressor use lead to a shift in early trauma care practices. Critical appraisal of current evidence is necessary to guide clinicians and outline research perspectives.
Main text: Current guidelines for managing trauma-induced hemorrhagic shock suggest titrating fluids and using vasopressors to achieve minimal blood pressure targets until hemorrhage is controlled. In case of traumatic brain injury with severe hemorrhage, blood pressure target increases. The scientific literature supporting these recommendations is limited, and several aspects remain the subject of ongoing scientific debate. The aim of this review is to evaluate the existing evidence on low-volume fluid resuscitation during the first hours of trauma management, with an emphasis on its integration with permissive hypotension, vasopressor use and cerebral perfusion pressure in traumatic brain injury. The review also highlights the limitations of current guidelines, particularly the lack of robust evidence supporting specific type of fluid, volumes and administration protocols tailored to specific trauma scenarios and populations.
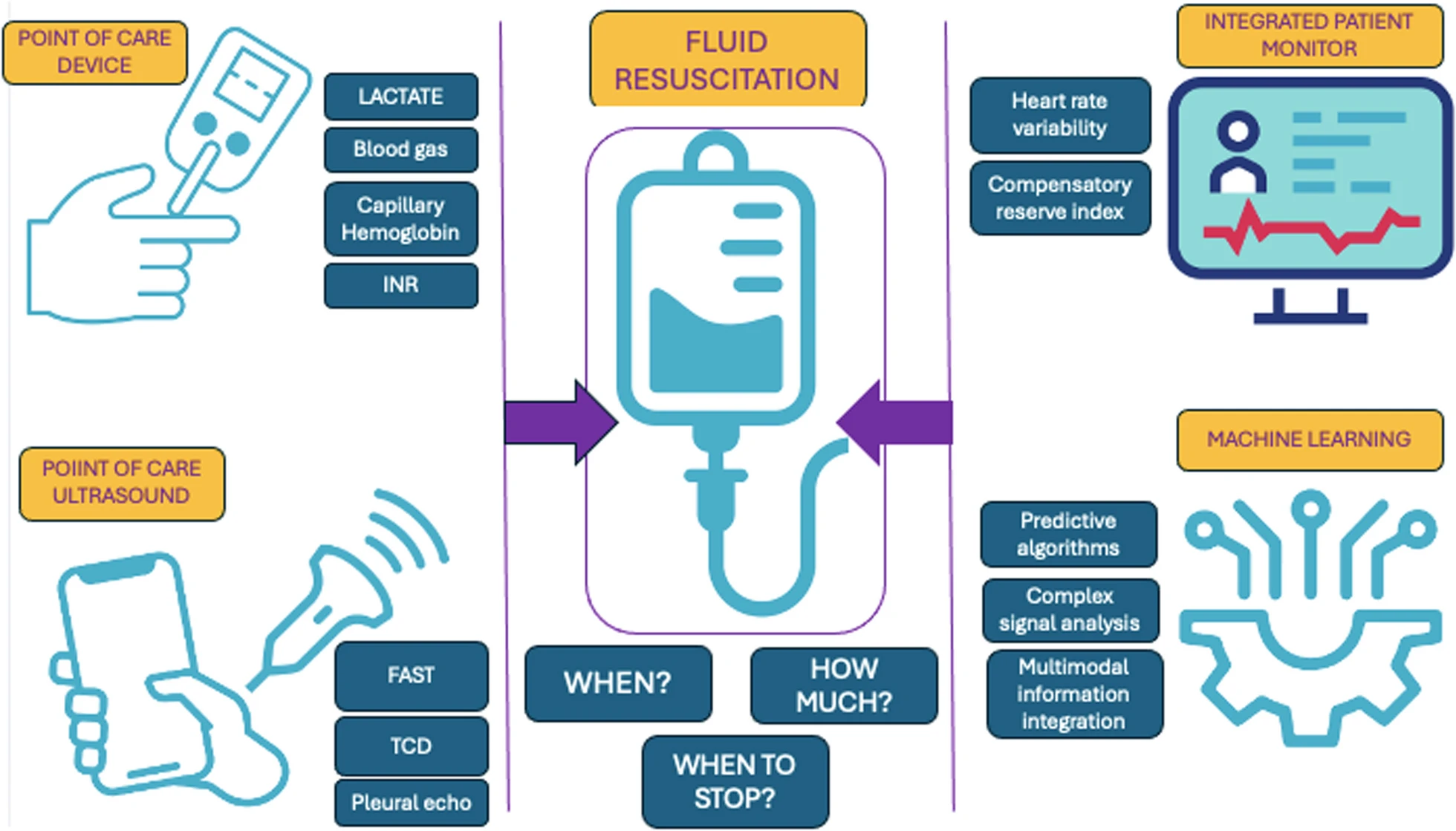
Emerging technologies such as point-of-care diagnostics, integrated monitoring systems, and machine learning hold promise for enhancing clinical decision-making in trauma care. These innovations could play a crucial role, ultimately helping clinicians address critical unanswered questions in trauma management and improve patient survival.
Conclusions: Crystalloid-based resuscitation remains relevant in early trauma care, but its application must be reassessed considering recent evidence and evolving practices. Further research is essential to refine fluid resuscitation guidelines, particularly in defining safe fluid volumes and the role of vasopressors. The integration of advanced monitoring technologies may offer new opportunities to optimize trauma care and improve outcomes.