14/12/2023
Des gants non stériles pour le parage des plaies ?
Sterile vs Nonsterile Gloves for the Repair of Wounds and Lacerations: A Systematic Review and Meta-Analysis
Haman Y et Al.JAMA Surg. 2023 Dec 13. doi: 10.1001/jamasurg.2023.5814.
Le recours au port de gants stériles n'est pas utile lors du parage de plaies en condition d'isolement et de recomplètement difficile.

Brûlures: Pensez au phosphore blanc !
Evidence for chemical burns by white phosphorus in Armenian soldiers during the 2020 Nagorno-Karabakh war
Son Brutyan S et Al. Injury. 2021 Apr;52(4):1100-1101.
La reconnaissance précoce des brûlures au phosphore blanc est fondamentale du fait du risque d'arrêt cardiaque liée à une hypocalcémie majeure. L'élimination rapide des particules de phosphore, le refroidissement des zones touchées par pansement humide et la réanimation hydroélectrolytique bien conduite sont essentiels. Pendant la guerre du Haut-Karabakh de 2020, les chirurgiens et les spécialistes des soins intensifs du Centre national des brûlés d'Erevan, en Arménie, ont été confrontés à un afflux important de brûlés présentant des brûlures creusantes, fluorescente à l'observation sous lumière ultraviolette et associées à une hypocalcémie profonde. Une meilleure sensibilisation aux conséquences des blessures par phosphore blanc est spécifique et peut sauver des vies.
| Tags : phosphore
Dispositifs supraglottiques:Pléthore ?
Review of Commercially Available Supraglottic Airway Devices for Prehospital Combat Casualty Care
07/12/2023
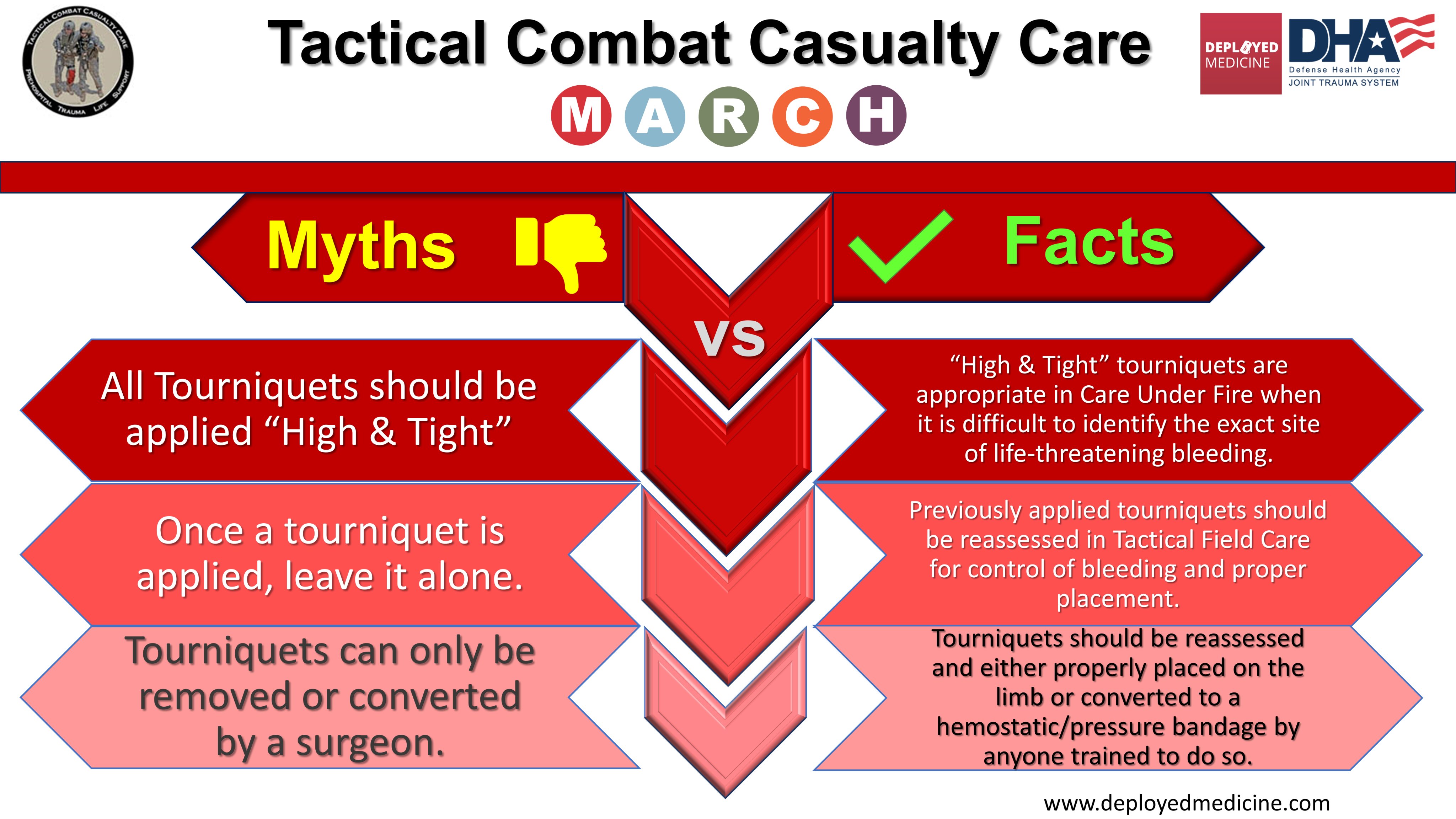
Histoires de conversion du garrot
Rethinking limb tourniquet conversion in the prehospital environment
John B Holcomb JB et Al. J Trauma Acute Care Surg . 2023 Dec 1;95(6):e54-e60.
----------------------------------------
Un plaidoyer pour un emploi large MAIS raisonné qui doit être ENSEIGNE et notamment la problématique de sa conversion. Ceci est d'autant plus important que les délais d'évacuations risquent d'être longs.
----------------------------------------
We have highlighted the issue of overuse of tourniquets and described why tourniquet conversion and replacement should be taught and done in the prehospital setting.
Clic sur l'image pour accéder au document
01/12/2023
Histoire de FiO2
Maximizing Oxygen Delivery in Portable Ventilators.
Blakeman T. et Al. Mil Med. 2022 Feb 4:usab561. doi: 10.1093/milmed/usab561
Background:
Military transport of critically ill/injured patients requires judicious use of resources. Maintaining oxygen (O2) supplies for mechanically ventilated is crucial. O2 cylinders are difficult to transport due to the size and weight and add the risk of fire in an aircraft. The proposed solution is the use of a portable oxygen concentrator (POC) to supply O2 for mechanical ventilation. As long as power is available, a POC can provide an endless supply of O2. Anecdotal evidence suggests that as little as 3 L/min of O2 could manage as many as 2/3 of the mechanically ventilated military aeromedical transport patients.
Materials and methods:
We evaluated two each of the AutoMedx SAVe II, Hamilton T1, Zoll 731, and Ventec VOCSN portable ventilators over a range of settings paired with 1 and 2 Caire SAROS POCs at ground level and simulated altitudes of 8,000 feet, 16,000 feet, and 22,000 feet. The Ventec VOCSN has the capability of utilizing an internal O2 concentrator that uses pulsed dose technology, which was also evaluated. Each ventilator was attached to a Michigan Instruments Training Test Lung. Output from the POC was bled into each ventilator via the mechanism provided with each device. A Fleisch pneumotach was used to measure delivered tidal volume (VT), and a fast-response O2 analyzer was used to measure FiO2 within the simulated lung. Ventilator parameters and FiO2 were continuously measured and recorded at each altitude. One-way analysis of variance was used to determine statistically significant differences (P < .05) in FiO2 between ventilators and among the same ventilator model at each testing condition.
Results:
Delivered FiO2 varied widely between ventilator models and between devices of the same model with some testing conditions. Differences in FiO2 between ventilators at a majority (98.5%) of testing conditions were statistically significant (P < .05) but not all were clinically important. The Zoll 731 delivered the highest and most consistent FiO2 over all ventilator/POC settings at all altitudes. Differences in FiO2 at a given ventilator/POC setting from ground level to 22,000 feet were not clinically important (<5%) with this device. The VOCSN utilizing the integrated internal O2 concentrator delivered the lowest FiO2 across all ventilator/POC settings and altitudes. Due to the inability of the SAVe II to operate at the minute ventilation and positive end expiratory pressure (PEEP) settings required by the testing protocol, the device was only tested at one ventilator setting. The Hamilton T1 failed to operate appropriately at the highest VT/PEEP setting at 16,000 feet and all but one ventilator setting at 22,000 feet. The delivered FiO2 was not included in the analysis for those ventilator settings. The highest delivered FiO2 was 0.85 ± 0.05 at the 250 mL VT setting using 2 POCs (P < .0001) at ground level with the Zoll 731.
Conclusions:
Oxygen delivery utilizing POCs is dependent upon multiple factors including ventilator operating characteristics, ventilator settings, altitude, and the use of pulsed dose or continuous flow O2. Careful patient selection would be paramount to provide safe mechanical ventilation using this method of O2 delivery.
Military Medicine