29/11/2020
Pneumothorax: Votre doigt compte
28/11/2020
Kétamine: Recommendations de l'ACEP
| Tags : kétamine
27/11/2020
Trauma du larynx: Faites une échographie !
Novel role of focused airway ultrasound in early airway assessment of suspected laryngeal trauma
Adi et al. Ultrasound J (2020) 12:37
Case presentation
We report a case series that illustrate the diagnostic value of focused airway ultrasound in the diagnosis of laryngeal trauma in patients presenting with blunt neck injury.
Conclusion
Early recognition, appropriate triaging, accurate airway evaluation, and prompt management of such injuries are essential. In this case series, we introduce the potential role of focused airway ultrasound in suspected laryngeal trauma, and the correlation of these exam findings with that of computed tomography (CT) scanning, based on the Schaefer classification of laryngeal injury.
26/11/2020
Recommandations voyageurs 2024
23/11/2020
Médicine tactique: Apport de la période afghane
Evolution of Pararescue medicine during operation Enduring Freedom
Stephen Rush S. et Al. Mil Med . 2015 Mar;180(3 Suppl):68-73.
This article highlights recent advances made in U.S. Air Force Pararescue Medical Operations in relation to tactical evacuation procedures. Most of these changes have been adopted and adapted from civilian medicine practice, and some have come from shared experiences with partner nations. Patient assessment includes a more comprehensive evaluation for hemorrhage and indications for hemorrhagic control. Ketamine has replaced morphine and fentanyl as the primary sedative used during rapid sequence intubation and procedural sedation. There has been an increasing use of the bougie to clear an airway or nasal cavity that becomes packed with debris. Video laryngoscopy provides advantages over direct laryngoscopy, especially in situations where there are environmental constraints such as the back of a Pave Hawk helicopter. Intraosseous access has become popular to treat and control hemorrhagic shock when peripheral intravenous access is impractical or impossible. Revisions to patient treatment cards have improved the efficacy and compliance of documentation and have made patient handoff more efficient. These improvements have only been possible because of the concerted efforts of U.S. Air Force and partner platforms operating in Afghanistan.
15/11/2020
Solutés hypersalés: Sûrs pour la coagulation
The effect of hypertonic saline and mannitol on coagulation in moderate traumatic brain injury patients
Wang H et Al. Am J Emerg Med. 2017 Oct;35(10):1404-1407
-------------------------------------
Du moins pour le salé à 3%, administré ici pendant 3 jours.
-------------------------------------
Background:
Hyperosmolar therapy, using either hypertonic saline (HTS) or mannitol (MT), is considered the treatment of choice for intracranial hypertension, a disorder characterized by high intracranial pressure (ICP). However, hyperosmolar agents have been postulated to impair coagulation and platelet function. The aim of this study was to identify whether HTS and MT could affect coagulation in moderate traumatic brain injury (TBI) patients.
Methods: In this prospective and randomized double-blind study, we included adult patients with moderate TBI. Patients were divided into two groups according to the type of hypertonic solution administered. Group A patients received 20% MT and group B patients received 3% HTS. Rotational thromboelastometry (ROTEM) parameters were used to assess coagulation and platelet function.
Results:
ROTEM parameters included CT (clotting time), CFT (clot formation time), maximum clot firmness (MCF) measured by MCF (EXTEM and INTEM), MCF (FIBTEM) and standard coagulation tests (p>0.05). No significant differences were found between the two groups. Moreover, ROTEM parameters did not show significant changes at different time points after administration of the hyperosmolar solutions (p>0.05).
Conclusions: Overall, use of 3% HTS and 20% MT for the control of ICP did not significantly affect patients' coagulation function. Therefore, hyperosmotic solution is safe and does not increase the risk of intracranial rebleeding.
14/11/2020
TraumCast: Episode 10
Blessure de la tête et du cou
11/11/2020
TraumCast: Episode 9
Brûlé grave de guerre
TraumCast: Episode 8
Blessures par explosion
Inhibition de l'histone déacetylsae pour l'hémorragie
Histone deacetylase 6 inhibition improves survival in a swine model of lethal hemorrhage, polytrauma, and bacteremia
Biesterveld BE et Al. J Trauma Acute Care Surg . 2020 Nov;89(5):932-939.
---------------------
Le TXA fait partie de l'arsenal thérapeutique en cas d'hémorragie sévère d'origine traumatique. Cela pourrait être également le cas des inhibiteurs de l'histone déacétylsae, famille de l'acide valproïque - Dépakine-
---------------------
Background: Trauma is the leading cause of death for young Americans. Nonspecific histone deacetylase inhibitors, such as valproic acid, have been shown to improve survival in preclinical models of lethal trauma, hemorrhage, and sepsis. The doses needed to achieve a survival benefit are higher than Food and Drug Administration-approved doses, and the nonspecificity raises concerns about unintended adverse effects. The isoform-specific histone deacetylase 6 inhibitor, ACY-1083, has been found to be as efficacious as valproic acid in a rodent model of hemorrhagic shock. We hypothesized that ACY-1083 treatment would improve survival in a swine model of lethal hemorrhage, polytrauma, and bacteremia.
Methods: Swine were subjected to 45% blood volume hemorrhage, brain injury, femur fracture, rectus crush, splenic and liver lacerations, and colon injury. After 1 hour of shock (mean arterial pressure, 30-35 mm Hg), animals were randomized to normal saline resuscitation (control) or normal saline plus ACY-1083 30 mg/kg treatment (n = 5/group). After 3 hours (simulating delayed evacuation), packed red blood cells and antibiotics were administered, the colon injury was repaired, and the abdomen was closed. Animals were then monitored for another 4 hours. Survival was assessed using Kaplan-Meier and log-rank test.
Results: This combination of injuries was lethal. All animals became bacteremic, in addition to the severe hemorrhagic shock. Survival in the control group was 0%, and ACY-1083 treatment increased survival to 80% (p = 0.019). There was no difference in the brain lesion size between the groups.
Conclusion: A single dose of ACY-1083 markedly improves survival in an otherwise lethal model of polytrauma, hemorrhagic shock, and bacteremia.
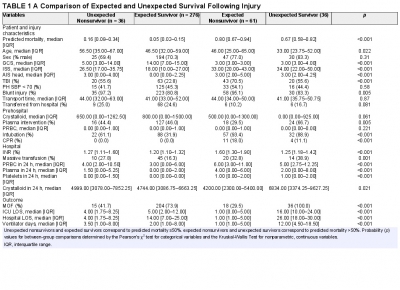
Plasma préhospitalier. Surtout pour certains
Characterization of unexpected survivors following a prehospital plasma randomized trial
J Trauma Acute Care Surg. 2020 Nov;89(5):908-914
Background: Prehospital plasma improves survival for severely injured trauma patients transported by air ambulance. We sought to characterize the unexpected survivors, patients who survived despite having high predicted mortality after traumatic injury.
Methods: The Prehospital Air Medical Plasma trial randomized severely injured patients (n = 501) to receive either standard care (crystalloid) or two units of prehospital plasma followed by standard care fluid resuscitation. We built a generalized linear model to estimate patient mortality. Area under the receiver operating characteristic curve was used to evaluate model performance. We defined unexpected survivors as patients who had a predicted mortality greater than 50% and survived to 30 days. We characterized patient demographics, clinical features, and outcomes of the unexpected survivors. Observed to expected (O/E) ratios and Z-statistics were calculated using model-estimated mortality for each cohort.
Results: Our model predicted mortality better than Injury Severity Score or Revised Trauma Score parameters and identified 36 unexpected survivors. Compared with expected survivors, unexpected survivors were younger (33 years [24, 52 years] vs. 47 years [32, 59 years], p = 0.013), were more severely injured (Injury Severity Score 34 [22, 50] vs. 18 [10, 27], p < 0.001), had worse organ dysfunction and hospital resource outcomes (multiple organ failure, intensive care unit, hospital length of stay, and ventilator days), and were more likely to receive prehospital plasma (67 vs. 46%, p = 0.031).
Nonsurvivors with high predicted mortality were more likely to receive standard care resuscitation (p < 0.001). Unexpected survivors who received prehospital plasma had a lower observed to expected mortality than those that received standard care resuscitation (O/E 0.56 [0.33-0.84] vs. 1.0 [0.73-1.32]). The number of prehospital plasma survivors (24) exceeded the number of predicted survivors (n = 10) estimated by our model (p < 0.001).
Conclusion: Prehospital plasma is associated with an increase in the number of unexpected survivors following severe traumatic injury. Prehospital interventions may improve the probability of survival for injured patients with high predicted mortality based on early injury characteristics, vital signs, and resuscitation measures.
03/11/2020
TraumCast: Episode 7
Stratégies transfusionnelles