20/08/2012
L'intubation mieux qu'un dispositif supraglottique
Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest
Wang HE et all. Resuscitation 83 (2012) 1061–1066
-------------------------------------------------------------------
Lors de la prise en charge préhospitalière d'un arrêt cardiaque il vaut mieux intuber que mettre en place un dispositif laryngé. Les conclusions de ce travail interpellent car elles vont à l'encontre de certaines propositions d'emploi de dispositifs laryngés pour le contrôle préhospitalier des voies aériennes.
-------------------------------------------------------------------
Objective
To simplify airway management and minimize cardiopulmonary resuscitation (CPR) chest compression interruptions, some emergency medical services (EMS) practitioners utilize supraglottic airway (SGA) devices instead of endotracheal intubation (ETI) as the primary airway adjunct in out-of-hospital cardiac arrest (OHCA). We compared the outcomes of patients receiving ETI with those receiving SGA following OHCA.
We performed a secondary analysis of data from the multicenter Resuscitation Outcomes Consortium (ROC) PRIMED trial. We studied adult non-traumatic OHCA receiving successful SGA insertion (King Laryngeal Tube, Combitube, and Laryngeal Mask Airway) or successful ETI. The primary outcome was survival to hospital discharge with satisfactory functional status (Modified Rankin Scale ≤3). Secondary outcomes included return of spontaneous circulation (ROSC), 24-h survival, major airway or pulmonary complications (pulmonary edema, internal thoracic or abdominal injuries, acute lung injury, sepsis, and pneumonia). Using multivariable logistic regression, we studied the association between out-of-hospital airway management method (ETI vs. SGA) and OHCA outcomes, adjusting for confounders.
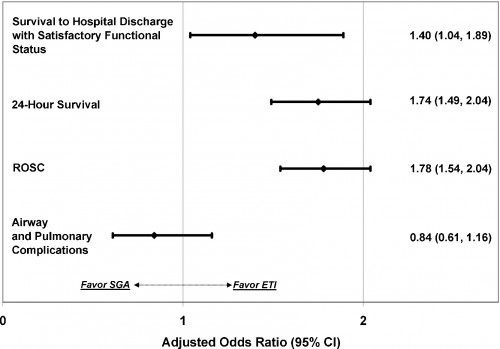
Of 10,455 adult OHCA, 8487 (81.2%) received ETI and 1968 (18.8%) received SGA. Survival to hospital discharge with satisfactory functional status was: ETI 4.7%, SGA 3.9%. Compared with successful SGA, successful ETI was associated with increased survival to hospital discharge (adjusted OR 1.40; 95% CI: 1.04, 1.89), ROSC (adjusted OR 1.78; 95% CI: 1.54, 2.04) and 24-h survival (adjusted OR 1.74; 95% CI: 1.49, 2.04). ETI was not associated with secondary airway or pulmonary complications (adjusted OR 0.84; 95% CI: 0.61, 1.16).
In this secondary analysis of data from the multicenter ROC PRIMED trial, ETI was associated with improved outcomes over SGA insertion after OHCA.

Les commentaires sont fermés.